
HICprevent
This award-winning blog supplements the articles in Hospital Infection Control & Prevention.
Outbreak: A Bad Bug in a Burn Unit
August 4th, 2023
By Gary Evans, Medical Writer
As infection control worst-case scenarios go, it doesn’t get much more challenging than a carbapenem-resistant Acinetobacter baumannii (CRAB) outbreak in a burn unit.
Carbapenem-resistant A. baumannii is given the highest threat rating of “urgent” by the Centers for Disease Control and Prevention (CDC), in part because it can linger in the environment and transfer resistance to other bacteria via mobile plasmids.
Thus, infection preventionists faced the challenge of identifying and containing a dangerous pathogen in the 11-bed burn unit at Bridgeport (CT) Hospital in March 2022. Since carbapenem is a last-line antibiotic, treatment options are very limited and burn patients are already at high risk of infections of any type because of the loss and damage of protective tissues.
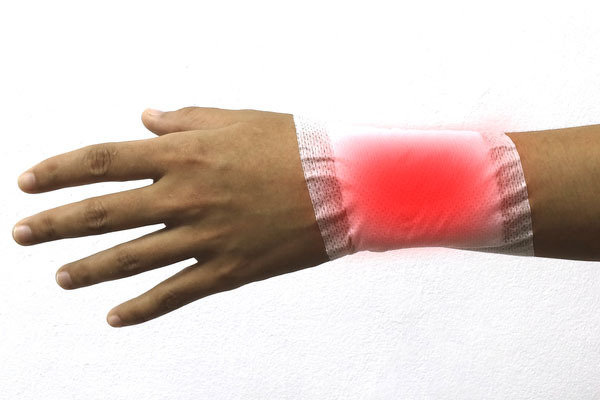
“[Infections] are the most common cause of morbidity and mortality, but the diagnosis is very unclear and complicated,” said Christina Murdzek, MHS, M(ASCP), CIC, infection prevention program manager of Hartford Healthcare in North Haven, CT. “The main signs that we look for in infections — warmth, edema, redness — those are already present with our burn patients.”
Murdzek described the outbreak and the interventions used to stop transmission at the 2023 conference of the Association for Professionals in Infection Control and Epidemiology (APIC).
“So, when we’re looking for an infection, we’re looking for a change in the appearance or the smell of the wound, and those are very subjective,” she said.
In addition, IPs in burn units look for emerging clinical conditions like hyperthermia, hypothermia, a decline in mental status, or signs of respiratory distress, she said.
“Unfortunately, those things [appear] very far along in the progression of an infection,” Murdzek said. “Even microbiological diagnosis of an infection is very unclear, as cultures are often mixed with all the patient’s flora.”
Enhanced infection control measures and rigorous environmental cleaning were implemented to prevent transmission of CRAB within the unit. At one point, the burn unit was shut down temporarily to do deep environmental decontamination and eradicate any possible reservoirs of CRAB.
It remains somewhat undetermined how the multidrug-resistant gram negative pathogen got into the unit, but the epidemiology points to a patient that was admitted after receiving burn care overseas.
However, given the diagnostic obstacles and some bureaucratic delays with the laboratory, the index patient was not officially diagnosed with CRAB until 17 days after admission to the unit.
The presumed index patient and two subsequent patients had genetically matched strains of A. baumannii, confirming transmission had occurred. The second patient acquired CRAB before the first patient had been diagnosed, meaning enhanced infection control and environmental cleaning measures had not been put in place yet.
“Our first patient passed away while in the hospital,” Murdzek said. “Patients two and three were released.’
Uncertain source
Given the delay in identifying the multidrug-resistant pathogen, it was not safe to assume that the first patient was the definitive source of the outbreak within the burn unit.
“It’s very easy to jump to the conclusion that our index patient brought this in, but we talked about the fact that it was 13 days into that patient’s admission when we took that first culture,” she said. “That’s a long time to make the assumption that that patient brought it in from their healthcare stay. It could have very easily come from a source within the hospital.”
Once CRAB was identified, the state health department and hospital and physician leadership were notified.
“We notified our nurses, our physicians, the OR staff, the housekeeping staff, nutrition, respiratory therapy, and physical therapy,” she said, adding that other patients and family members on the unit were also alerted.
“We didn’t want anyone to be scared or get this mass hysteria when they came in and they saw that things weren’t the same than they were the day before,” Murdzek said.
The unit implemented “enhanced contact precautions” that are used when high-impact pathogens like Candida auris are discovered.
“It’s contact precautions with a little added boost,” she said.
The measures included wearing a gown and gloves, favoring alcohol rubs for hand hygiene, and use of dedicated equipment for known cases. The unit environment was also a major concern, as researchers have found that this pathogen can persist in the environment for prolonged periods.
“Examination of clinical isolates has shown that most strains of A. baumannii can survive for at least 20 days on dry surfaces, with some strains capable of surviving over 3 months,” one study reported. “During outbreaks, A. baumannii has been found on a wide range of surfaces in clinical environments, including bed rails, pillows, mattresses, tables, and ventilators. The specific molecular mechanisms that allow A. baumannii to persist on dry surfaces are not entirely clear.”
Among the stepped up cleaning measures in the burn unit was the use of a bleach product for the last cleaning of the day. “We also did a ‘double clean’ or a supervised clean,” Murdzek said. “That’s ensuring that the clean is happening — we’re not missing any areas. So, somebody’s watching, saying ‘you missed a spot’ or your cleaning practices are [incorrect].”
The outbreak ended with the third infected patient, but the unit has to remain vigilant because of the vulnerability of burn patients and the measures used to care for them. For example, hydrotherapy uses a water spray so intense that is also called “hydrosurgery.”
“It’s a lot more than a bath,” she told APIC attendees. “It’s the removal of tissue and dried pus, and it’s a very complicated process. If you have burn patients that are being cared for in your hospital, you have to be involved as an infection preventionist. You have to talk to your practitioners about balancing the risks and the benefits [in burn patient care]. There are benefits, but also a lot of risks.”
For more on this story, see the next issue of Hospital Infection Control & Prevention.
Gary Evans, BA, MA, has written numerous articles on infectious disease threats to both patients and healthcare workers for more than three decades. These include stories on healthcare-associated infections like MRSA, C. diff and a panoply of emerging multidrug resistant gram negative bacteria and fungi like Candida auris. In an era of pandemic pathogens, he has covered HIV, SARS, pandemic influenza, MERS, Ebola and SARS-CoV-2. Evans has been honored for excellence in analytical reporting five times by the National Press Club in Washington, DC.
