What Kind of Bundle Branch Block?
By Ken Grauer, MD
Professor Emeritus in Family Medicine, College of Medicine, University of Florida
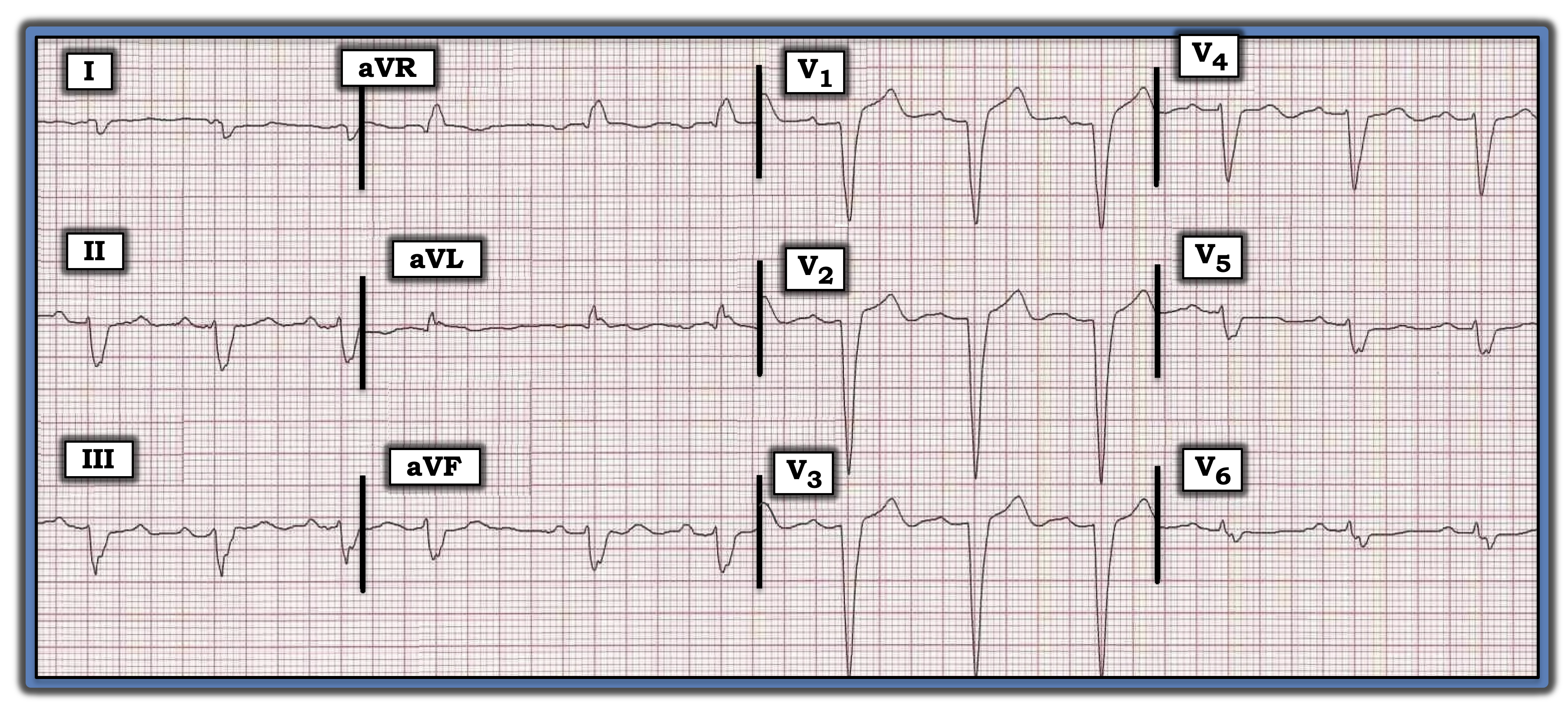
What is the optimal way to describe the conduction defect in the figure below?
Background: One of the areas in which experienced interpreters differ greatly is in their description of conduction defects. Assuming QRS widening in a supraventricular rhythm is not the result of hyperkalemia or other toxicity, and assuming the patient has not been diagnosed with Wolff-Parkinson-White syndrome, classification of 12-lead ECG conduction disturbances can be simplified into one of three basic categories: right bundle branch block (RBBB), left bundle branch block (LBBB), or intraventricular conduction defect (IVCD).
The tracing in the figure illustrates this concept. The rhythm is sinus, as determined by the upright P wave with fixed PR interval in lead II. The QRS complex clearly is wide (i.e., longer than 0.12 seconds in duration).
• Although the negative QS complexes in the anterior leads of the tracing are consistent with LBBB, the required upright, monophasic QRS complex in lateral leads I and V6 is lacking. Therefore, this is not LBBB.
• This tracing also is not consistent with RBBB since there is no positivity at all in right-sided lead V1.
• By the process of elimination, the optimal way to describe QRS morphology in this tracing is IVCD.
What is IVCD? The ECG appearance of IVCD is difficult to characterize. Instead of representing a discrete defect within the conduction system (as is typically the case with RBBB and LBBB), IVCD often is the result of a series of other pathophysiologic processes, such as prior infarction and/or scarring from cardiomyopathy.
• It is difficult to be specific about ongoing events for this tracing. The QRS complex is fragmented (i.e., with marked notching in multiple leads), suggesting significant underlying heart disease. But we cannot diagnose recent, or even previous, infarction because of the unusual pattern of QRS widening.
• There is some ST elevation in the anterior leads, but considering the presence of IVCD (and the depth of anterior S waves), this does not appear acute. The remaining leads on the tracing show nonspecific ST-T wave changes.
Bottom Line: Using IVCD as a clinical classification for QRS widening not attributable to RBBB or LBBB simplifies ECG classification without sacrificing the accuracy of interpretation. Clinical correlation and comparison with prior tracings will be needed for appropriate management, and to determine which ECG changes are “new” vs. “old.”
For more information about and further discussion of this case, please visit here.
Assuming QRS widening in a supraventricular rhythm is not the result of hyperkalemia or other toxicity, and assuming the patient has not been diagnosed with Wolff-Parkinson-White syndrome, classification of 12-lead ECG conduction disturbances can be simplified into one of three basic categories. The tracing in the figure illustrates this concept.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
