Updates on Syncope
October 1, 2022
Related Articles
-
Echocardiographic Estimation of Left Atrial Pressure in Atrial Fibrillation Patients
-
Philadelphia Jury Awards $6.8M After Hospital Fails to Find Stomach Perforation
-
Pennsylvania Court Affirms $8 Million Verdict for Failure To Repair Uterine Artery
-
Older Physicians May Need Attention to Ensure Patient Safety
-
Documentation Huddles Improve Quality and Safety
AUTHORS
Taylor Cesarz, MD, Emergency Medicine Resident, PGY-2, University of Central Florida/HCA Healthcare GME (Greater Orlando); Resident Instructor, University of Central Florida College of Medicine
Shayne Gue, MD, FACEP, FAAEM, Director of Education, University of Central Florida/HCA Healthcare GME (Greater Orlando); Assistant Professor of Emergency Medicine, University of Central Florida College of Medicine
PEER REVIEWER
Catherine A. Marco, MD, Professor of Emergency Medicine, Penn State Health — Milton S. Hershey Medical Center, Penn State College of Medicine
EXECUTIVE SUMMARY
- Syncope is defined as an acute loss of consciousness that is abrupt in onset, short duration, with rapid recovery and with spontaneous recovery without intervention. It is common and often seen in the emergency department (ED). Despite evaluation, the cause of syncope in most patients will remain unknown.
- Syncope has three main causes: cardiac, reflex-mediated, and orthostatic. In the ED, evaluation is focused on determining the symptoms/activities leading up to the event, the symptoms at the time of the event, and the symptoms following the event.
- All patients who present with syncope should have a 12-lead electrocardiogram (ECG) performed in the ED. Those with an abnormal ECG should be considered for further testing either on an outpatient or inpatient basis. There are several risk stratifying scores that help to differentiate between low- and high-risk individuals.
- Other diagnostic studies in the ED should be guided by the history and physical exam. Beyond the 12-lead ECG, there is little evidence that more diagnostic testing is needed in low-risk individuals.
Definition of the Problem
Syncope is defined as a self-limiting, sudden onset loss of consciousness (LOC) with associated loss of postural tone.1 Further, it must include four major elements: it must be transient, abrupt in onset, short in duration, and have a rapid spontaneous recovery without intervention.2 The transient LOC should not be associated with trauma as an inciting factor. Nontraumatic transient LOC can be divided into further subcategories, including psychogenic, epileptic, rare causes, and syncope.
Relevancy
Syncope is a common problem experienced among the adult population, accounting for about 1% to 5% of emergency department (ED) visits and 1% to 6% of hospital admissions.2-5 About 25% of people who experience syncope will seek care from an ED.4 One study found that from 2006 to 2013, the rate of ED visits for syncope increased by 21%.6 Average hospital length of stay for a syncopal admission is 5.5 days.7 Admissions for syncope have an economic burden of $2.4 billion per year.8
Syncopal episodes have a significant effect on quality of life. Patients who experience syncope demonstrate increases in functional impairment similar to those of patients with chronic diseases, such as rheumatoid arthritis and chronic back pain.9 From a psychosocial perspective, patients with syncope have impairment at a similar level to patients with psychiatric diagnoses, including anxiety and depression. Recurrence of syncope after an initial episode occurs in 10% to 27.5% of patients within two years, depending on risk factors.10 Syncope leads to reduced function regarding activities of daily living, particularly driving, daily life routines, exercise, and sleep, likely because of a fear of recurrence.11,12
Epidemiology
Because the definition of syncope has evolved over time, studies characterizing the incidence and epidemiology have been inconsistent. Some studies include seizures, syncope secondary to trauma, hypoglycemia, intoxication, and transient ischemic attack (TIA) as etiologies of syncope, which by current definitions are separate disease entities. This makes it difficult to accurately determine the true prevalence of syncope.
Despite this, it remains evident that syncope is a common phenomenon. Studies have found overall incidence rates of syncope of 6.2-17.2 per 1,000 person-years.3,13 The lifetime cumulative incidence of syncope is high, up to 35% to 41%, with increased rates seen in women (41%) as compared to men (28%).13,14 There is a 35% recurrence rate.7 With regard to age, syncope presents in a trimodal distribution, with higher prevalence at ages 20, 60, and 80 years, with a tendency for females to present five to seven years after males in the last age group.3 Multiple studies demonstrate higher rates of syncope with increasing age.3,13 One study found that syncope incidence rates ranged from 8-22 per 1,000 person-years for ages 10-69 years, with a notable rise in incidence rates to 40.2 per 1,000 person-years in ages 70-79 years and 81.2 per 1,000 person-years in ages > 80 years.3
Of patients presenting with syncope, an estimated 32% to 40% are admitted to the hospital, a value that increases with age, with a rate of 58% for patients > 80 years of age.7,15 The cost associated with admission is approximately $8,759, with increases for ages > 50 years and for those requiring cardiac procedures, including placement of a pacemaker or implantable cardioverter-defibrillator (ICD).16 The average costs associated with these interventions are $24,040 and $77,917, respectively.
Mortality rates in patients with syncope depend largely on the underlying cause. The mortality rate for syncope is low, with an overall rate of 0.28%.16 Mortality is significantly higher in patients with cardiac etiology compared to non-cardiac etiology, with rates of 50.5% and 30%, respectively, at five years.17 This likely is due to the presence of structural heart disease, specifically congestive heart failure (CHF), which is an independent predictor of mortality.18 In addition to CHF, other predictors of one-year mortality include age > 45 years, history of ventricular arrhythmia, and history of an abnormal electrocardiogram (ECG), with mortality as high as 80% in patients with three to four of these risk factors.
Pathophysiology
The pathophysiology of syncope depends on the cause of syncope. However, each etiology generally results in one final common pathway: global cerebral hypoperfusion.7 A rapid decrease in blood pressure (BP) has been shown to decrease perfusion, which in short bursts (as short as 6-8 seconds) can precipitate a syncopal episode.19 Usually, this is caused by a temporary decrease in cardiac output (CO) or in systemic vascular resistance (SVR), resulting in a low BP leading to hypoperfusion.2,16
Syncope can be classified further into three main causes: cardiac, reflex-mediated, and orthostatic.2,20 Among these, reflex-mediated is the most common, followed by cardiac, and, finally, orthostatic.13 Of note, in the vast majority of syncope cases, the cause is unknown.
The first etiology of syncope is cardiac, which can be divided into three subcategories, including arrhythmia, structural heart disease, and others. All of these subcategories share a common mechanism of decreasing cardiac output.2 Both primary arrhythmias and arrhythmias induced by medications can result in syncope.2,20,21 Structural heart disease, including valvular disorders, cardiac masses, and pericardial tamponade, all can decrease CO leading to low BP and hypoperfusion. Other structural disorders of the entire vascular system, including pulmonary embolism, aortic dissection, and pulmonary hypertension, are included in this category.2,20
Reflex-mediated syncope is the result of abnormal vasodilation and bradycardia, usually caused by some trigger.2,20,21 Subcategories of reflex-mediated syncope include cardioinhibitory syncope, vasodepressor syncope, and mixed type.2 In cardioinhibitory syncope, a trigger leads to bradycardia, which in turn decreases CO, leading to lower BP and global hypoperfusion. Vasovagal syncope, situational syncope, and carotid sinus syncope fall under this category, assuming that bradycardia is the predominant mechanism, and they are further defined based on their triggers.2,20 These types of syncope also may be categorized as a vasodepressor type of syncope, in the event they have a predominant mechanism of decreased SVR.2 Additionally, reflex syncope can result from a mix of these two phenomena if both mechanisms occur concurrently.
Finally, orthostatic syncope is the result of transient global hypoperfusion due to an inappropriate drop in BP caused by positional changes.2,20,22 It is diagnosed when there is a decrease in BP ≥ 20 mmHg systolic or ≥ 10 mmHg diastolic or an increase in heart rate (HR) ≥ 30 beats per minute with standing.20,21 This includes three different subcategories: decreased venous return, structural deficiencies of the autonomic nervous system (ANS), and drug-induced autonomic nervous failure (ANF). Decreased venous return occurs as a result of venous pooling and volume loss, which includes etiologies such as hemorrhage and gastrointestinal (GI) loss of fluid.2,22 ANS damage can be both primary and secondary. Both types result in a mix of low CO and SVR. Parkinson’s disease, multiple system atrophy, Lewy body dementia, and pure autonomic failure all are examples of primary ANS damage. Secondary ANS damage occurs with diabetes, amyloidosis, uremia, and spinal cord injuries. Lastly, drug-induced ANF results in pure SVR-induced syncope. Common drugs that may cause this include alcohol, vasodilators, diuretics, and antidepressants.2 Proper technique for obtaining orthostatic vital signs as well as the limitations of this tool are discussed in the Diagnostic Studies section.
Clinical Features
Typically, patients will present with the chief complaint of temporary LOC. Initially, it is important for the physician to determine if the LOC is due to syncope or another etiology, such as TIA, seizure, hypoglycemia, or intoxication. To differentiate if the temporary LOC is due to syncope or other causes, physicians should ask the four questions in Table 1.
Table 1. Four Questions to Identify Syncope |
Four questions can be used to identify if a transient loss of consciousness is syncopal or secondary to another etiology. If the answer to all four questions is yes, then transient loss of consciousness likely is syncopal in nature. 1. Is there a complete loss of consciousness with loss of postural tone? 2. Is the loss of consciousness rapid in onset? 3. Is loss of consciousness temporary? 4. Are symptoms explained by global cerebral hypoperfusion? |
Emergency physicians can think about the syncopal history in three sections: what happened before, during, and after the syncopal event. Providers should ask about prodromal symptoms, including nausea, vomiting, diaphoresis, warmth, abdominal pain, chest pain, dyspnea, and palpitations.23,24 Prodromal symptoms of nausea, warmth, or abdominal pain are most commonly associated with reflex-mediated or vasovagal syncope. Syncope that occurs rapidly without prodromal symptoms or symptoms of palpitations, chest pain, or dyspnea is more concerning for a cardiac etiology.
In terms of the actual syncopal event, providers should elicit the mechanism of syncope. Important details include what the patient was doing when the syncopal event occurred, including sitting, prolonged standing, changing position from lying down or sitting to standing, or exertion. Syncope in the setting of positional changes occurs frequently with syncope secondary to orthostatic hypotension. Other essential historical findings about the setting include if the syncope was preceded by strong emotion, a painful stimulus, or a medical procedure, as these would signify possible vasovagal syncope. Patients who had onset of syncope preceded by micturition, defecation, or deglutition may have situational syncope. Syncope triggered by neck turning or placement of clothing around the neck (i.e., tie, scarf, or shirt collar) may be related to carotid hypersensitivity.25 Syncope in the setting of exertion or while sitting is more characteristic of cardiac etiology.21,23,24 It is helpful to ask about witnesses or video footage of the event to verify the history.26 If possible, physicians should obtain information about any shaking or rhythmic movements, any skin color changes, duration of LOC, or any loss of bowel/bladder continence during the event, since these may signify other non-syncopal causes of LOC.2,27
Lastly, physicians should ask about recovery from the syncopal event, including any residual symptoms (chest pain, dyspnea, nausea, vomiting, or abdominal pain) and how soon the patient returned to their baseline mental status.2,23 Patients with a prolonged return to baseline or continued state of altered mental status may be having a postictal period from a seizure or a toxic/metabolic/infectious encephalopathy rather than a syncopal event.23 See Table 2 for a summary of important historical findings in syncope.
Table 2. Historical Factors and Their Association with Various Types of Syncope |
Cardiac
Reflex-Mediated
Orthostatic
|
Because syncope can result in injury, providers also should include pertinent trauma history, including whether any head strike occurred; whether the patient has any head, neck, back, chest, abdominal, or extremity pain; whether the patient is ambulatory; and whether the patient is on any anticoagulation.26 Providers can perform a trauma exam focusing on any head or neck injuries, spine exam, and musculoskeletal and skin evaluation.
Relevant past medical history includes any history of cardiac disease, such as coronary artery disease, aortic stenosis, CHF, and arrhythmia.23,28 These would point to a potential cardiac cause of syncope. Physicians also should ask about any past medical history of seizures.25 Providers should take a complete medication history, specifically asking about medications that are arrhythmogenic (antiarrhythmics, antibiotics, or psychotropics) and medications that can cause autonomic system failure (alpha-adrenergic blockers, nitrates, or diuretics).26,29 Similarly, a family history of sudden cardiac death is concerning for a possible cardiac etiology of syncope.23 Social history, including any alcohol or drug use, should be assessed to rule out intoxication as a potential contributor to symptoms.25
In addition to a thorough history about the syncopal event, the physician should obtain a review of systems to rule out life-threatening diagnoses on the differential. This includes questions regarding risk factors for pulmonary embolism, such as hypercoagulability, pleuritic chest pain, and dyspnea.26 Abdominal pain, vomiting, diarrhea, or history of bloody stool or black tarry stool can be indicative of gastrointestinal (GI) losses/hypovolemia or hemorrhage secondary to abdominal aortic aneurysm rupture, GI bleed, or ectopic pregnancy. Furthermore, because cardiac syncope is associated with a higher morbidity and mortality, a review of systems also should thoroughly evaluate for any existing cardiac disease. Therefore, history taking should elicit symptoms of CHF or structural heart disease. Relevant history and physical exam findings include exertional chest pain or dyspnea, orthopnea, paroxysmal nocturnal dyspnea, weight gain, and lower extremity swelling.
When performing the physical exam, physicians should obtain a complete set of vital signs with particular attention paid to the HR and BP. Obtaining orthostatic vital signs may be helpful in narrowing down the differential diagnosis to syncope secondary to orthostatic hypotension. A complete cardiovascular exam is critical to identify irregular heart rhythms, murmurs, and stigmata of chronic heart disease, such as an S3 gallop or jugular venous distension.26-28 A focused trauma exam should be performed based on the patient’s historical findings, with particular attention to signs of head trauma or cervical spine injury.28 Physicians should perform a neurologic exam to evaluate the patient’s mental status and assess for any focal neurologic deficits. Prolonged changes in mental status are not consistent with true syncope and may point to another etiology, such as metabolic encephalopathy or seizure.26,28,29 Similarly, focal neurologic deficits are consistent with a cerebrovascular cause of LOC, such as TIA or stroke.24,26,28 Rectal examination may be indicated if history points to GI bleed as a potential cause of volume loss or anemia.26 See Figure 1 for a summary of physical exam findings in the syncope evaluation.
Figure 1. Physical Exam Findings in Syncope |
|
 | Neurologic
Head, Eyes, Ears, Nose, and Throat
Heart
Respiratory
Abdominal/Gastrointestinal
Musculoskeletal
Skin
Extremities
Vital Signs
|
Diagnostic Studies
According to the American Heart Association (AHA) 2017 Syncope Guidelines, all emergency physicians should obtain an ECG during the initial evaluation of patients presenting with syncope (Class I, Level B evidence).1 This is one of the only recommendations that applies to every patient with syncope. Although prognosis and management may not change based on ECG, studies show an increased risk of arrhythmia within 30 days with certain ECG findings, including non-sinus rhythm, frequent premature ventricular contractions (PVC), shortened PR interval, first degree atrioventricular (AV) block, complete left bundle branch block (LBBB), and findings consistent with ischemia.30 Although it will only identify about 5% of syncope etiologies, it is noninvasive and low cost, making it a useful diagnostic tool.26,31 If there is high suspicion for arrhythmia based on history, patients should be placed on continuous telemetry while in the ED to detect any arrhythmia potentially missed by ECG.25
There are many different potential findings on ECG in the setting of syncope, including, but not limited to, bradycardia, sick sinus syndrome, tachyarrhythmias (ventricular tachycardia, atrial fibrillation/flutter), AV block, prolonged QT/torsades de pointes, Brugada syndrome, hypertrophic obstructive cardiomyopathy (HOCM), and Wolff-Parkinson-White (WPW) pattern.32 See Table 3 for a systematic approach to evaluating the ECG in patients presenting with syncope. Figures 2-8 show common ECG findings in the more rare, but not to miss, arrhythmogenic causes of syncope.
Table 3. Five Steps to Analyze ECG in Syncope |
Step 1: Rate
Step 2: Rhythm
Step 3: Intervals
Step 4: Strains and Blocks
Step 5: ST Segments
Miscellaneous
|
* Also may indicate non-arrhythmic etiologies, including pulmonary embolism, hemorrhage, hypervolemia, sepsis, aortic dissection ECG: electrocardiogram; AV: atrioventricular; SVT: supraventricular tachycardia; VT: ventricular tachycardia; VF: ventricular flutter; WPW: Wolff-Parkinson-White; LGL: Lown-Ganong-Levine syndrome; LBBB: left bundle branch block; RBBB: right bundle branch block; HOCM: hypertrophic obstructive cardiomyopathy |
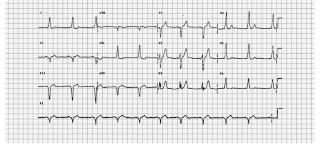
Figure 2. “Not to Miss” ECG Findings in Syncope: Various Stages of AV Block |
1st degree AV block: PR interval >200 ms. (benign) |
Type I second degree AV block (Mobitz I): gradually lengthening PR interval followed by an eventual dropped QRS. (benign) |
Type II second degree AV block (Mobitz II): fixed PR interval, followed by a dropped QRS. |
Type III/complete AV block: complete dissociation of atrial and ventricular contraction. The P waves and R waves will be regularly spaced, but with no apparent relation to each other.32,42 |
Source: Npatchett - Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=47645793 |
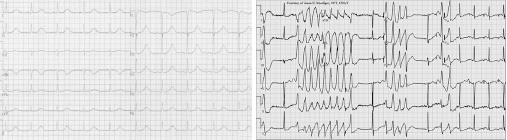
Figure 3. “Not to Miss” ECG Findings in Syncope: Wolff-Parkinson-White |
Wolff-Parkinson-White (WPW): Presence of an accessory pathway (bundle of Kent), which bypasses the AV node leading to early but slower ventricular depolarization resulting in characteristic findings including shortened PR interval < 120 ms and a delta wave (slurred upstroke of QRS). QRS may be widened and T wave inversions may be present.43 |
 |
Source: Michael Rosengarten BEng, MD. McGill - EKG World Encyclopedia http://cme.med.mcgill.ca/php/index.php , courtesy of Michael Rosengarten BEng, MD.McGill, CC BY-SA 3.0, https://commons.wikimedia.org/... |
Figure 4. “Not to Miss” ECG Findings in Syncope: Lown-Ganong-Levine Syndrome |
Lown-Ganong-Levine syndrome: Similar to Wolff-Parkinson-White in that an accessory pathway is present; however, the pathway is located in AV node, so the ECG will show a shortened PR interval, but no delta wave.32 |
 |
Source: https://www.wikiwand.com/en/Lown%E2%80%93Ganong%E2%80%93Levine_syndrome |
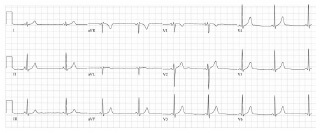
Figure 5. “Not to Miss” ECG Findings in Syncope: Torsades de Pointes |
|
Torsades de Pointes: Twisting of the points or oscillation of amplitude of QRS around the isoelectric line resulting in polymorphic ventricular tachycardia associated with QTc prolongation.49 |
|
 | |
Sources: CardioNetworks: Googletrans - CardioNetworks: De-Acquired_longQT.jpg, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=83863836.Jer5150 - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=19738256 |
|
Figure 6. “Not to Miss” ECG Findings in Syncope: ARVD |
Arrhythmogenic right ventricular dysplasia (ARVD): Genetic disorder with fatty infiltration of right ventricle with characteristic ECG findings of T wave inversions in V1-V3, epsilon wave (deflection at end of QRS), V1-V3 QRS widening, and prolonged S wave upstroke in V1-V3.50 |
 |
Sources: The original uploader was Ksheka at English Wikipedia. - Transferred from en.wikipedia to Commons., CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=2281018CardioNetworks: Drj - CardioNetworks: Arvd_ecg1.png, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=24365205 |
Figure 7. “Not to Miss” ECG Findings in Syncope: Brugada Syndrome |
Brugada syndrome: Inherited Na channelopathy that can lead to syncope and sudden cardiac death. Type I coved ST elevation in V1, V2, V3 with descent to inverted T wave. May have a right bundle branch block appearance. Type 2 shows saddleback ST segment elevations in V2-V3.63 |
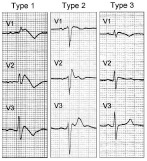 |
Source: Napolitano C, Priori SG. Brugada syndrome. Orphanet J Rare Dis. 1, 35. 2006. doi:10.1186/1750-1172-1-35. PMID 16972995., CC BY 2.0, https://commons.wikimedia.org/w/index.php?curid=3900813 |
Figure 8. “Not to Miss” ECG Findings in Syncope: HOCM |
Hypertrophic obstructive cardiomyopathy (HOCM): Genetic disorder leading to septal thickening resulting in signs of left ventricular hypertrophy and characteristic needle/dagger like Q waves (present in lateral and sometimes in inferior leads). It is the most common cause of sudden cardiac death.64 |
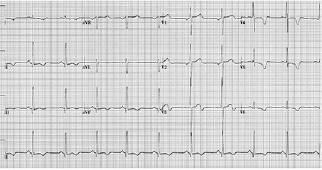 |
Source: W.G. de Voogt, MD, PhD, SLAZ, The Netherlands - W.G. de Voogt, MD, PhD, SLAZ, The Netherlands, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=24370726 |
Orthostatic vital signs should be obtained if history and physical exam findings support that diagnosis. The proper technique involves measurement of BP while lying supine, followed by measurement of BP after three minutes of standing, with positive results including either a decrease in systolic BP ≥ 20 mmHg, decrease in diastolic BP ≥ 10 mmHg, overall drop in BP to ≤ 90 mmHg systolic, or increase in HR ≥ 30 beats per minute.2 While orthostatic vital signs may be helpful in patients with a clinical picture suggestive of orthostatic hypotension, they are not diagnostic.33,34 Physicians should be aware of the limitations of this diagnostic tool and use it appropriately, considering all alternative etiologies. One observational study found no difference in 30-day serious outcomes between older adults with or without positive orthostatic vital signs.35 Many elderly patients may exhibit positive orthostatic vital signs regardless of the etiology of syncope, and the presence of positive orthostatics may mislead the physician into ruling in a benign diagnosis without fully evaluating more serious etiologies.34
Additional testing may be helpful based on specific history and physical exam findings (Class IIa, Level B evidence).1,26,36 For example, a complete blood count may be indicated if evaluating for anemia in the setting of potential hemorrhagic etiology of syncope or if planning to use a risk stratification tool.26 It also may be useful if history is pointing toward sepsis to evaluate white blood cell count, lactic acid, and blood cultures. A beta-human chorionic gonadotropin should be obtained in any female patient of reproductive age who presents with syncope to rule out ectopic pregnancy. A point of care (POC) glucose may be useful if ruling out hypoglycemia as a cause of LOC. While specific testing may be indicated in certain cases, the AHA recommends against routine comprehensive laboratory screening unless the history and physical exam point to specific etiologies of syncope (Class III, Level B).1,36
Several tests are overused in evaluating syncope. Although troponin commonly is ordered, elevated levels are not always associated with cardiac syncope.34 Troponins should be ordered judiciously, only when there is suspicion for acute coronary syndrome (ACS) based on the history. While an elevated brain natriuretic peptide (BNP) has been shown to have an association with cardiac syncope, it has an unknown effect on clinical decision-making and should be ordered only if there is suspicion of heart failure.1 Similarly, testing for pulmonary embolism should be performed only if the history and physical exam indicate this as a possible cause of the patient’s presentation.34 Previous studies have demonstrated that pulmonary embolism occurs in less than 1% of patients presenting with syncope, so there is no utility for routine screening in the ED.37 Computed tomography (CT) of the head is another test commonly overused in the ED evaluation of syncope.38 One study found that head CTs were ordered in 57% of patients and only yielded diagnostic results in 1% of these patients.1,34 The AHA syncope guidelines recommend against routine use of head CT/neuroimaging (Class III, Level B). Similarly, in the 2014 Choosing Wisely Campaign, the American College of Emergency Physicians (ACEP) recommended against routine head CT in syncope evaluation.39 Use should be limited to specific situations for which there is concern for head trauma secondary to syncope or there is high suspicion for stroke based on history and physical exam.1,39 Other factors that have been associated with abnormal CT findings in the setting of syncope include history of malignancy, focal neurologic deficits, and age > 60 years.40 See Table 4 for a summary of diagnostic workup of syncope.
Table 4. Diagnostic Workup for Syncope Evaluation |
|
CT: computed tomography; hCG: human chorionic gonadotropin |
Differential Diagnosis
The differential diagnosis for syncope is broad, but providers can remember various etiologies by understanding the pathophysiology of syncope. Just as the pathophysiology can be split into categories of cardiac, reflex-mediated, and orthostatic hypotension (all of which lead to lower BP and global hypoperfusion via decreases in either the CO or SVR), so too can the differential diagnosis.
When a patient is presenting with LOC, it is important to consider additional causes, other than syncope, that may be life-threatening. These are etiologies of LOC that do not meet the four criteria of syncope (transient, rapid onset, short duration, and spontaneous recovery).30 Some of these causes are outlined in Table 5.
Table 5. Non-Syncopal Causes of Loss of Consciousness |
Neurologic
Trauma-Induced
Metabolic
Toxicologic/Environmental
|
Management
By definition, syncope is transient and involves a rapid return to normal baseline, so most patients should not need extensive management in the ED setting. Physicians should attempt to identify an underlying cause of syncope and, if possible, provide targeted treatment. However, a large majority of patients presenting with syncope will not have an underlying cause identified while in the ED, so the most important aspect of management is risk stratification, which is discussed later.
Management of syncope for some patients may begin in the prehospital/emergency medical services (EMS) setting. EMS providers may be able to gather history from the patient and witnesses.27,30 EMS should obtain vital signs and POC glucose to rule out hypoglycemia as a cause of symptoms.30 An ECG should be obtained to evaluate for ischemia or arrhythmia.27,30 If there is concern for stroke as a cause of LOC, then stroke assessment should be performed by EMS providers to determine an appropriate transport destination.27
Similar to the diagnostic workup, management of patients with syncope depends largely on etiology determined from the history and physical exam. Immediate stabilization is necessary if hemodynamic instability is present. In patients in whom the provider suspects an etiology that may lead to hypovolemia (GI losses or bleed, hemorrhage secondary to ectopic pregnancy or ruptured abdominal aortic aneurysm, or concern for volume depletion due to sepsis), intravenous (IV) fluids or blood products should be provided.25 If patients are presenting with acute chest pain concerning for myocardial ischemia, appropriate treatment for ACS should be provided. If an arrhythmia is present, acute management, including medications, cardioversion, or defibrillation, may be warranted.
Further studies may be performed in the inpatient setting. Inpatient evaluation and management of syncope may include cardiac imaging, telemetry monitoring, cardiac stress testing, electrophysiologic studies (EPS), and tilt table testing.1 There is limited utility of routine cardiac imaging including echocardiography, cardiac CT, and cardiac magnetic resonance imaging (MRI) in the inpatient setting. Echocardiography should be performed if there is high concern for valvular disease and can lead to a diagnosis in 48% of patients with suspected cardiac syncope (Class IIa, Level B). The utility of cardiac CT or MRI is more limited and should be reserved for patients who have suspected pulmonary embolism, cardiac sarcoidosis, or arrhythmogenic right ventricular dysplasia (ARVD) as suspected etiologies of syncope. Stress testing may be considered in patients who have exertional syncope (Class IIa, Level C).1,41 Telemetry is a valuable diagnostic tool, but only if there is high suspicion for an arrhythmogenic cause of syncope (Class 1, Level B). Routine use of continuous telemetry has a diagnostic yield of less than 5%.1 Ambulatory cardiac monitoring (Holter monitors, external loop recorders, patch recorder) may be considered in a subset of patients.41 For patients with recurrent symptoms that are unexplained after initial diagnostic workup, an ICD may be considered (Class IIa, Level B).1 Electrophysiologic studies may be performed in patients with suspected cardiac disease, with a diagnostic yield of 50%. However, it should not be done in patients with normal ECG and normal cardiac structure and function, with low suspicion for arrhythmia (Class II, Level B). Routine electroencephalogram (EEG) testing is not recommended, unless historical features indicate seizure (Level III, Class B). Carotid imaging is recommended against, since carotid stenosis is not consistent with the mechanism global hypoperfusion of syncope (Class III, Level B). Lastly, tilt table testing is indicated in patients with suspected vasovagal syncope, orthostatic syndromes, distinguishing convulsive syncope from epilepsy, and evaluating for psychogenic causes of syncope (Class IIa, Level B).
Additional Aspects
There is controversy regarding use of carotid sinus massage in the diagnostic evaluation of syncope.25 Carotid sinus hypersensitivity is an abnormal baroreceptor reflex that occurs with manipulation of the carotid sinus.1 Diagnosis is made when carotid sinus massage reproduces syncope, asystole > 3 seconds, AV block, or drop of > 50 mmHg in systolic BP.2,30 However, there are several contraindications to performing this test, including history of TIA or stroke within three months, known carotid stenosis, carotid bruit, history of peripheral arterial disease, history of coronary artery disease, history of myocardial infarction within three months, and history of ventricular arrhythmias. It is a current recommendation by both the AHA and European Society of Cardiology to perform carotid sinus massage in the evaluation of undifferentiated syncope in patients > 40 years of age.1,2 Despite these recommendations, studies have demonstrated low diagnostic yield (13.7%) of carotid sinus massage, especially in patients ages 40-59 years.44 Therefore, the utility is unclear on the routine use of this test, especially in patients in the age range of 40-59 years.
There are many safety considerations in patients with syncope. One study has shown that patients diagnosed with syncope have twice the risk of having a motor vehicle collision.45 Guidelines regarding driving recommendations in patients with syncope remain unclear.46 Some sources recommend a driving restriction of six months for any patient with syncope.47 Other sources acknowledge the many nuances of syncope, including low rates of recurrence while driving, different types of syncope having different warning signs/prodromal symptoms that can help prevent accidents in the setting of proper education, and how different etiologies of syncope have different risks of recurrence.46 In addition to risk while driving, there is an associated 1.4-fold increased risk of occupational accidents in patients diagnosed with syncope. This risk increases in patients with recurrent syncope.48 Patients with syncope have a 31.3% two-year risk of job termination. This was associated with mental health morbidities, including depression. Occupational injuries requiring hospital evaluation are higher in the manual occupational sector. It is imperative for clinicians to recognize both the individual patient safety risks, public health risks, and higher risk of morbidities after a diagnosis of syncope. Providers should educate patients on trigger avoidance, recognition of prodromal symptoms, and counterpressure maneuvers to try to prevent motor vehicle collisions and occupational injuries.
Various decision tools can be used to risk stratify patients when determining an appropriate disposition. Individual tools and how to use them will be discussed in more detail in the Disposition section. However, it is important to note that the clinical application of these tools is limited. It currently is a Class IIb, Level B recommendation to use risk stratification tools, but it is important to recognize the potential pitfalls associated with these tools. Many of these tools require specific laboratory tests that have been shown to be limited in diagnostic utility. Furthermore, these risk stratification tools have not been shown to be more sensitive in ruling out high-risk syncope than clinical gestalt.1
Another consideration regarding disposition of the syncopal patient is the use of observation units.1,41 Recent studies have demonstrated that observation units for syncope lead to shorter hospital stays and lower healthcare cost ($1,400 for ED observation in comparison to $2,420 for hospitalization) with no effect on all-cause mortality.51 However, additional research has indicated that the use of observation units does not lead to any increased diagnosis rate or patient satisfaction rate. Furthermore, there is no consensus on what constitutes an observation unit for syncope.1,51 Studies of various ED observation units use different resources available (cardiac monitoring, echocardiography, tilt table testing, stress testing, or an on-call electrophysiologist) and have varying observation time periods.52 There also is uncertainty regarding application of structured ED observation protocols to rural EDs or EDs without these resources. Currently, it is a Class IIa, Level B recommendation to use structured ED observation protocols to reduce hospital admissions for syncope.1 Further studies are needed to determine appropriate observation times, diagnostic testing and resources, and selection of patients meeting criteria for observation units.51,52
Disposition
While it is still the emergency physician’s role to perform a diagnostic evaluation to rule out potential life-threatening etiologies of syncope, an estimated 50% of patients will not receive a definitive diagnosis of the underlying cause of syncope in the ED.53 Therefore, it is important for the physician to be able to risk stratify patients based on history and physical exam findings to determine appropriate disposition.26 For patients with an unclear etiology of syncope, providers can stratify into low-risk, medium-risk, and high-risk categories based on the criteria in Tables 6 and 7.54 Patients are considered high risk if they have one high-risk characteristic, low risk if they have one or more low-risk characteristics and absence of high-risk factors, and medium risk if they do not meet either of these criteria.
Table 6. Low-Risk Factors for Syncope1,30,54,55 |
History
Physical Exam
Electrocardiogram
|
Table 7. High-Risk Factors for Syncope1,30,54,55 |
History
Physical Exam
Electrocardiogram
Labwork
|
WPW: Wolff-Parkinson-White; ARVD: arrhythmogenic right ventricular dysplasia; HOCM: hypertrophic obstructive cardiomyopathy |
Consider admission for patients who are deemed high risk. In addition, patients who are identified to have a serious medical condition in the ED should be considered for admission (Class I, level B).1 Some examples of conditions that meet these criteria include arrhythmias, cardiac ischemia, severe aortic stenosis, pericardial tamponade, hypertrophic obstructive cardiomyopathy, prosthetic valve dysfunction, aortic dissection, pulmonary embolism, acute heart failure, severe anemia, GI bleed, major traumatic injury, or persistent vital sign abnormalities. Patients meeting criteria for low-risk syncope or those who have a clinical picture consistent with vasovagal syncope can be discharged safely (Class IIa, Level C).1,54 Patients who are at intermediate risk may require further evaluation.
There are several risk stratification tools used to evaluate syncope that may be useful in these cases (Class IIb, Level B).1,36 One decision-making tool is the San Francisco Syncope Tool, which uses several criteria, remembered with the mnemonic CHESS.56
C: CHF history
H: Hematocrit < 30%
E: ECG abnormality
S: Shortness of breath
S: Systolic BP < 90 mmHg
A patient is considered high risk if they have any one of the listed features.26 When initially designed, the rule was found to have a 96% sensitivity and 62% specificity for syncope with serious outcomes within seven days.56 However, other studies failed to reproduce this high sensitivity and suggest that use of the score actually may increase unnecessary admissions.26,57
The Canadian Syncope Risk Score (CSRS) is another decision-making tool that stratifies patients into different risk categories using the criteria in Table 8.
Table 8. Risk Stratification of the Canadian Syncope Risk Score |
|||
Risk Categories |
Score |
Overall Risk |
Range |
Predisposition to vasovagal symptoms |
+1 |
Very low risk |
-3 to -2 |
History of heart disease |
+1 |
Low risk |
-1 to 0 |
Any systolic blood pressure < 90 mmHg or > 180 mmHg |
+2 |
Medium risk |
1 to 3 |
Elevated troponin |
+2 |
High risk |
4 to 5 |
Abnormal QRS axis (< 30 or > 90 degrees) |
+1 |
Very high risk |
6 to 11 |
QRS duration > 130 ms |
+1 |
||
Correct QT interval > 480 ms |
+2 |
||
Vasovagal syncope |
+2 |
||
Cardiac syncope |
+2 |
||
This tool evaluated serious 30-day outcomes, including arrhythmic and non-arrhythmic conditions.58 One validation study found a rate of serious 30-day outcomes of 0.3% and 0.7% in the very low and low-risk groups, respectively. Rates of serious outcomes for the medium, high, and very high-risk groups were 8.0%, 19.2%, and 51.3%, respectively.58,59 This tool was found to have a sensitivity of 97.8% and a specificity of 44.3%. This tool may be more useful for patients who are lower risk, since it did not include patients with serious outcomes obvious on presentations, in contrast to the San Francisco Syncope rule. One limitation of this tool is its application to the United States population, since it is largely studied in Canadian EDs among patients with different comorbidities, access to resources, and different healthcare systems. In one external validation of the CSRS in the U.S. population, the CSRS performed similarly to clinical judgment.60
The Faint score uses several factors, similar to the San Francisco Syncope Rule, to determine if a patient is at high risk for a 30-day serious cardiac event, specifically for patients > 60 years old.61 (See Table 9.)
Table 9. The Faint Score |
|
Heart failure |
+1 |
History of arrhythmia |
+1 |
Abnormal ECG |
+1 |
Elevated BNP |
+2 |
Elevated troponin |
+1 |
ECG: electrocardiogram; BNP: brain natriuretic peptide |
|
For scores of 0 vs. ≥ 1, there was a 96.7% sensitivity and a 22.2% specificity for serious cardiac outcome.62 This risk stratification tool has not been externally validated, making it less useful in stratifying for disposition.55
The Osservatorio Epidemiologica sulla Sincope nel Lazio (OESIL) score is a tool developed in Italy that predicts one-year mortality in syncope patients using four criteria listed in Table 10.55 Using this tool, mortality at one year was 0.8% for 1 point, 19.6% for 2 points, 34.7% for 3 points, and 57.1% for 4 points.61 The creators of the tool recommend discharge in patients who are low-risk (0-1 point) and admission for high-risk patients (2-4 points).
Table 10. Characteristics of the OESIL Score |
|
Age > 65 years |
+1 |
Cardiovascular disease |
+1 |
No prodromal symptoms |
+1 |
Abnormal ECG |
+1 |
OESIL: Osservatorio Epidemiologica sulla Sincope nel Lazio; ECG: electrocardiogram |
|
All of these decision-making tools require diagnostic laboratory tests that are not routinely recommended in syncope evaluation, unless there is a high suspicion for specific etiologies on history or physical exam.1 Of note, ACEP published in its review on the AHA 2017 syncope guidelines that there is no evidence that risk-stratification scores are superior to clinical judgment.41 They should be used judiciously in specific cases where patients are considered intermediate-risk to help support clinician disposition decisions.
Summary
Syncope is a common ED chief complaint that often results in over-ordering of tests and unnecessary admission to the hospital, with significant economic impact. Syncope is, by definition, a transient, abrupt LOC that is self-limiting and the result of global hypoperfusion secondary to a drop in BP from decreased CO or decreased SVR. The differential diagnosis is broad and can be categorized into cardiac, reflex-mediated, and orthostatic syncope. A majority of patients will not receive a clear diagnosis of the cause of their syncope in the ED. Rather, the main focus of the emergency medicine physician is to risk stratify the patient based on the history and physical exam. A 12-lead ECG is the only test that is routinely recommended in evaluating syncope. Other diagnostics should be ordered on the basis of history and physical exam findings. When determining the disposition of a patient, physicians should know factors that are associated with high- and low-risk syncope. Decision-making tools can be used to help determine disposition for intermediate-risk patients but do not perform better than clinical gestalt.
REFERENCES
- Shen WK, Sheldon RS, Benditt DG, et al. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2017;70:e39-e110.
- Task Force for the Diagnosis and Management of Syncope; European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA); et al. Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J 2009;30:2631-2671.
- Ruwald MH, Hansen ML, Lamberts M, et al. The relation between age, sex, comorbidity, and pharmacotherapy and the risk of syncope: A Danish nationwide study. Europace 2012;14:1506-1514.
- Brignole M, Menozzi C, Bartoletti A, et al. A new management of syncope: Prospective systematic guideline-based evaluation of patients referred urgently to general hospitals. Eur Heart J 2006;27:76-82.
- Shen WK, Decker WW, Smars PA, et al. Syncope evaluation in the emergency department study (SEEDS): A multidisciplinary approach to syncope management. Circulation 2004;110:3636-3645.
- Anand V, George S, Benditt D, et al. Trends of emergency department visits for syncope/collapse in USA: Analysis of 2006-2013 National Emergency Department Sample Database. Circulation 2018;134:1-1.
- da Silva RM. Syncope: Epidemiology, etiology, and prognosis. Front Physiol 2014;5:471.
- Sun BC. Quality-of-life, health service use, and costs associated with syncope. Prog Cardiovasc Dis 2013;55:370-375.
- Linzer M, Pontinen M, Gold DT, et al. Impairment of physical and psychosocial function in recurrent syncope. J Clin Epidemiol 1991;44:1037-1043.
- Brignole M, Vardas P, Hoffman E, et al. Indications for the use of diagnostic implantable and external ECG loop recorders. Europace 2009;11:671-687.
- van Dijk N, Sprangers MA, Colman N, et al. Clinical factors associated with quality of life in patients with transient loss of consciousness. J Cardiovasc Electrophysiol 2006;17:998-1003.
- Linzer M, Gold DT, Pontinen M, et al. Recurrent syncope as a chronic disease: Preliminary validation of a disease-specific measure of functional impairment. J Gen Intern Med 1994;9:181-186.
- Soteriades ES, Evans JC, Larson MG, et al. Incidence and prognosis of syncope. N Engl J Med 2002;347:878-885.
- Ganzeboom KS, Mairuhu G, Reitsma JB, et al. Lifetime cumulative incidence of syncope in the general population: A study of 549 Dutch subjects aged 35-60 years. J Cardiovasc Electrophysiol 2006;17:1172-1176.
- Sun BC, Emond JA, Camargo CA Jr. Characteristics and admission patterns of patients presenting with syncope to U.S. emergency departments, 1992-2000. Acad Emerg Med 2004;11:1029-1034.
- Alshekhlee A, Shen WK, Mackall J, Chelimsky TC. Incidence and mortality rates of syncope in the United States. Am J Med 2009;122:181-188.
- Kapoor WN. Evaluation and outcome of patients with syncope. Medicine (Baltimore) 1990;69:160-175.
- Kapoor WN. Current evaluation and management of syncope. Circulation 2002;106:1606-1609.
- Stephenson JB. Fits and Faints. Cambridge University Press; 1990.
- Patel PR, Quinn JV. Syncope: A review of emergency department management and disposition. Clin Exp Emerg Med 2015;2:67-74.
- Quinn J, D’Souza P. Approach to syncope. In: Mattu A, Swadron S, eds. CorePendium. CorePendium, LLC. Updated July 15, 2021. https://www.emrap.org/corependium/chapter/recn9iTEoblED2hWk/Approach-to-Syncope#h.bu7vj83ee8ea.
- Kapoor WN. Syncope. In: Walker HK, Hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd ed. Butterworths; 1990. https://www.ncbi.nlm.nih.gov/books/NBK224/
- Syncope. In: Stern SC, Cifu AS, Altkorn D. eds. Symptom to Diagnosis: An Evidence-Based Guide, 3e. McGraw Hill; 2014. https://accessmedicine.mhmedical.com/content.aspx?bookid=1088§ionid=61700616
- Long B. Syncope: The latest on clinical work-up and management. emDOCs.net. Published Sept. 10, 2015. http://www.emdocs.net/syncope-the-latest-on-clinical-work-up-and-management/#_ENREF_1
- Welsh J, Welsh T. Evaluation of syncope in the emergency department. Emerg Med Rep 2015;36:261-272.
- Huff JS, Decker WW, Quinn JV, et al. Clinical policy: Critical issues in the evaluation and management of adult patients presenting to the emergency department with syncope. Ann Emerg Med 2007;49:431-444.
- Radulović M, Čolaković G, Emiš-Vandlik N, et al. Prehospital treatment of syncope. Naucni casopis urgentne medicine - Halo 194 2019;25:84-91.
- Long B. Vascular causes of syncope. emDOCs.net. Published June 2, 2015. http://www.emdocs.net/vascular-causes-of-syncope/
- Tisdale JE, Chung MK, Campbell KB, et al. Drug-induced arrhythmias: A scientific statement from the American Heart Association. Circulation 2020;142:e214-e233.
- Morris J. Emergency department management of syncope. Emerg Med Pract 2021;23:1-24.
- Lambert M. Practice guidelines: ACEP policy on evaluating patients with syncope in the emergency department. Am Fam Physician 2008;78:516-518.
- Wonnacott D. Medical Concept: ECGs in Syncope. CanadiEM. https://canadiem.org/medical-concept-ecgs-in-syncope/. Published Sept. 21, 2015.
- Schaffer JT, Keim SM, Hunter BR, et al. Do orthostatic vital signs have utility in the evaluation of syncope? J Emerg Med 2018;55:780-787.
- Staiert D. Low risk syncope – pearls and pitfalls. emDOCs.net. Published Aug. 20, 2018. http://www.emdocs.net/low-risk-syncope-pearls-and-pitfalls/
- White JL, Hollander JE, Chang AM, et al. Orthostatic vital signs do not predict 30 day serious outcomes in older emergency department patients with syncope: A multicenter observational study. Am J Emerg Med 2019;37:2215-2223.
- Ernst J. Syncope: ED updates from the 2017 AHA/ACC/HRS clinical policy. emDOCs.net. Published Feb. 12, 2018. http://www.emdocs.net/syncope-ed-updates-2017-aha-acc-hrs-clinical-policy/
- Costantino G, Ruwald MH, Quinn J, et al. Prevalence of pulmonary embolism in patients with syncope. JAMA Intern Med 2018;178:356-362.
- Hatharasinghe AT, Etebar K, Wolsky R, et al. An assessment of the diagnostic value in syncope workup: A retrospective study. HCA Healthcare Journal of Medicine 2021;2(6). doi:10.36518/2689-0216.1306
- Choosing Wisely. Avoid CT of the head in asymptomatic adult patients in the emergency department with syncope, insignificant trauma and a normal neurological evaluation. Published Oct. 27, 2014. https://www.choosingwisely.org/clinician-lists/acep-avoid-head-ct-for-asymptomatic-adults-with-syncope/
- Ozturk K, Soylu E, Bilgin C, et al. Predictor variables of abnormal imaging findings of syncope in the emergency department. Int J Emerg Med 2018;11:16.
- Quinn JV, Stiell IG, McDermott DA, et al. Derivation of the San Francisco syncope rule to predict patients with short-term serious outcomes. Ann Emerg Med 2004;43:224-232.
- Knabben V, Chhabra L, Slane M. Third-degree atrioventricular block. In: StatPearls. StatPearls Publishing; May 22, 2022.
- Conte J. ECG pointers: Syncope and Wolff-Parkinson-White. emDOCs.net. Published Feb. 12, 2019. http://www.emdocs.net/ecg-pointers-syncope-and-wolf-parkinson-white/
- Humm AM, Mathias CJ. Unexplained syncope: Is screening for carotid sinus hypersensitivity indicated in all patients aged >40 years? J Neurol Neurosurg Psychiatry 2006;77:1267-1270.
- Numé AK, Gislason G, Christiansen CB, et al. Syncope and motor vehicle crash risk: A Danish nationwide study. JAMA Intern Med 2016;176:503-510.
- Curtis AB, Epstein AE. Syncope while driving: How safe is safe? Circulation 2009;120:921-923.
- Sorajja D, Nesbitt GC, Hodge DO, et al. Syncope while driving: Clinical characteristics, causes, and prognosis. Circulation 2009;120:928-934.
- Numé A-K, Kragholm K, Carlson N, et al. Syncope and its impact on occupational accidents and employment: A Danish nationwide retrospective cohort study. Circ Cardiovasc Qual Outcomes 2017;10:e003202.
- Cohagan B, Brandis D. Torsade de pointes. In: StatPearls. StatPearls Publishing; Aug. 11, 2021.
- Buttner R, Burns E. Arrhythmogenic right ventricular dysplasia (ARVD). Life in the Fast Lane. Published Jan. 31, 2022. https://litfl.com/arrhythmogenic-right-ventricular-dysplasia-arvd/
- Spiro W, Ditkowsky J, Sharma VK, et al. Patient outcomes in emergency department observation units for syncope. EM Resident. Published June 11, 2021. https://www.emra.org/emresident/article/syncope-observation/
- Firouzbakht T, Shen ML, Groppelli A, et al. Step-by-step guide to creating the best syncope units: From combined United States and European experiences. Auton Neurosci 2022;239:102950.
- Patel PR, Quinn JV. Syncope: A review of emergency department management and disposition. Clin Exp Emerg Med 2015;2:67-74.
- Costantino G, Sun BC, Barbic F, et al. Syncope clinical management in the emergency department: A consensus from the first international workshop on syncope risk stratification in the emergency department. Eur Heart J 2016;37:1493-1498.
- Blau A. Syncope in the ED: Who can go home? emDOCs.net. Published Feb. 14, 2021. http://www.emdocs.net/syncope-in-the-ed-who-can-go-home/
- Quinn JV, Stiell IG, McDermott DA, et al. Derivation of the San Francisco syncope rule to predict patients with short-term serious outcomes. Ann Emerg Med 2004;43:224-232.
- Sun BC, Mangione CM, Merchant G, et al. External validation of the San Francisco syncope rule. Ann Emerg Med 2007;49:420-427.
- Ramzy MM. Validation of the Canadian syncope risk score. REBEL EM. Published April 20, 2020. https://rebelem.com/validation-of-the-canadian-syncope-risk-score/
- Thiruganasambandamoorthy V, Sivilotti MLA, Le Sage N, et al. Multicenter emergency department validation of the Canadian Syncope Risk Score. JAMA Intern Med 2020;180:737-744.
- Ramzy MM. External validation of the Canadian Syncope Risk Score. REBEL EM. Published July 8, 2021. https://rebelem.com/external-validation-of-csrs/
- Colivicchi F, Ammirati F, Melina D, et al. Development and prospective validation of a risk stratification system for patients with syncope in the emergency department: The OESIL risk score. Eur Heart J 2003;24:811-819.
- Probst MA, Gibson T, Weiss RE, et al. Risk stratification of older adults who present to the emergency department with syncope: The FAINT Score. Ann Emerg Med 2020;75:147-158.
- Mitchell LB. Brugada syndrome. Merck Manuals Professional Edition. Updated January 2021. https://www.merckmanuals.com/professional/cardiovascular-disorders/arrhythmias-and-conduction-disorders/brugada-syndrome
- Buttner R, Burns E. Hypertrophic cardiomyopathy (HCM). Life in the Fast Lane. Published May 22, 2022. https://litfl.com/hypertrophic-cardiomyopathy-hcm-ecg-library/
Syncope is a common ED chief complaint that often results in over-ordering of tests and unnecessary admission to the hospital, with significant economic impact. The main focus of the emergency medicine physician is to risk stratify the patient based on the history and physical exam.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
