Tachycardia in the Emergency Department: Part II
November 1, 2023
Related Articles
-
Echocardiographic Estimation of Left Atrial Pressure in Atrial Fibrillation Patients
-
Philadelphia Jury Awards $6.8M After Hospital Fails to Find Stomach Perforation
-
Pennsylvania Court Affirms $8 Million Verdict for Failure To Repair Uterine Artery
-
Older Physicians May Need Attention to Ensure Patient Safety
-
Documentation Huddles Improve Quality and Safety
AUTHOR
Rahul Rege, MD, Assistant Professor of Emergency Medicine, Penn State Health – Milton S. Hershey Medical Center, PA
PEER REVIEWER
Frank LoVecchio, DO, FACEP, Vice-Chair for Research, Medical Director, Samaritan Regional Poison Control Center, Emergency Medicine Department, Maricopa Medical Center, Phoenix, AZ
EXECUTIVE SUMMARY
- In many conditions, sinus tachycardia occurs as a compensatory response to maintain cardiac output and oxygen delivery to vital organs.
- Re-entry is the mechanism for many tachydysrhythmias, including atrioventricular nodal re-entrant tachycardia (AVNRT), atrioventricular re-entrant tachycardia (AVRT), and ventricular tachycardia.
- Adrenergic stimulation is the primary mechanism for arrhythmias due to enhanced automaticity.
- Triggered activity and delayed after-depolarization are implicated in the torsades de pointes arrhythmia.
- A narrow or normal QRS duration during a tachydysrhythmia indicates ventricular activation is via a healthy His-Purkinje system.
- Vagal maneuvers have a 20% to 40% success rate for terminating re-entrant supraventricular tachycardias.
- Adenosine should be avoided in patients with Wolff-Parkinson-White syndrome because about 15% of such patients have adenosine-sensitive bypass tracts that can precipitate a cardiac arrest if used during a tachydysrhythmia.
- Synchronized cardioversion should be used for tachydysrhythmias in unstable patients with a pulse.
This issue completes the two-part series on tachycardia. This issue will finish the discussion of additional causes of tachycardia, address management, and conclude by covering some challenging issues with this arrhythmia.
— J. Stephan Stapczynski, MD, Editor
Neurologic Causes of Tachycardia
Numerous anatomic and physiological links exist between the central nervous system (CNS) and the heart, with several CNS pathologies able to directly cause tachycardia.1 Sympathetic pre-ganglionic neurons are located in the T1-L2 segments in the spinal cord and receive inputs from the hypothalamus and medulla. These neurons innervate the heart as well as other organs, including the adrenal medulla, stimulating the release of norepinephrine and epinephrine.2 These neurotransmitters act directly on the β1 receptors on the heart to stimulate sinus node automaticity, increase excitability of the His-Purkinje system, and stimulate contractility of the myocardium to cause tachycardia.2
Primary neurologic complaints that have been shown to cause tachycardia include seizure, stroke, intracranial hemorrhage, traumatic brain injury, and primary headaches. While the detailed review of every neurologic illness implicated in tachycardia is too broad for the scope of this review, understanding the link between the nervous system and the heart is important for the emergency provider to conduct a thorough evaluation and identify underlying diagnoses.
Endocrine Causes of Tachycardia
Hyperthyroidism, a condition in which the thyroid gland produces and secretes inappropriately high amounts of thyroid hormone, has a prevalence in the United States of approximately 1.2%.3 The most common causes of hyperthyroidism include Graves’ disease, toxic multinodular goiter, and toxic adenoma.3 At a cellular level, increased levels of circulating thyroid hormone have direct and indirect effects on cardiac muscle and blood vessels, leading to increased activation of the sinoatrial node, faster myocyte contraction, and decreased refractory period.4
Pheochromocytoma is a rare catecholamine-producing tumor, which arises from chromaffin cell lines in the adrenal medulla or paraganglia.5 Through direct stimulation of both β-adrenergic and α-adrenergic receptors, these patients typically present with tachycardia and hypertension.5 While this diagnosis rarely is made in the emergency department, patients can present in extremis with tachydysrhythmias, hypertensive emergency, and high-output heart failure.4
Diabetes is one of the most common conditions present in the world today and can have several detrimental effects on cardiovascular health. Studies have shown that the presence of hypoglycemia in people with diabetes can cause both atrial and ventricular premature beats as well as sustained tachydysrhythmias leading to increased morbidity and mortality.6 It is hypothesized that glycemic variability with hypoglycemia causes significant oxidative stress, inflammation, and endothelial dysfunction, which can lead to sympathetic stimulation causing tachycardia.6 Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) are known to cause significant intravascular volume depletion and lead to sympathetic stimulation in the presence of a stressor.7
Pulmonary Causes of Tachycardia
Diminished lung function can directly cause tachycardia. In the presence of a pulmonary embolism (PE), the most common vital sign abnormality is tachycardia.8 Physiologically, a PE can lead to tachycardia by increasing afterload on the right ventricle, which requires the heart rate to increase to maintain cardiac output. Tachycardia in the presence of a PE serves as an independent risk factor for adverse outcomes.8
Chronic obstructive pulmonary disease (COPD) has a strong association with multifocal atrial tachycardia. During a COPD exacerbation, hypoventilation along with hypoxemia can lead to a ventilation and perfusion mismatch, and the body attempts to compensate and maintain oxygenation by increasing the heart rate. COPD has been shown to independently increase atrial ectopy and atrial tachydysrhythmias.9
Pathophysiology
Cardiac Output
The role of the heart is to supply the body with oxygenated blood to maintain cellular metabolism. Cardiac output, measured in liters/minute, is obtained by multiplying heart rate and stroke volume. Logically, any decrease in the stroke volume leads to an increase in the heart rate as a compensatory response to maintain cardiac output.10 Stroke volume is dependent on preload, afterload, and cardiac contractility.
Preload, the amount of ventricular stretch prior to contraction, correlates with the blood volume in the ventricle.10 Preload largely depends on ventricular filling. Conditions that result in reduced intravascular volume or obstruct venous return decrease ventricular filling and preload. The resultant decrease in stroke volume stimulates a compensatory tachycardia. Blood and fluid loss can lead to decreased intravascular volume. Tension pneumothorax and cardiac tamponade decrease preload by mechanically obstructing the venous return of blood.11
Afterload is the force against which the ventricles must act to eject blood.10 Conditions that increase ventricular afterload, such as pulmonary embolism, pulmonary hypertension, and hypertensive emergency, increase the force the heart needs to pump against, which leads to an increase in heart rate and contractility.11 Paradoxically, in cases of distributive shock, such as sepsis or anaphylaxis, a reduction in afterload is seen along with tachycardia. This is due to the release of inflammatory mediators, which not only decrease the afterload but can lead to decreased contractility and compensatory tachycardia.11
Contractility is the strength with which the ventricles contract and is dependent on the health of the cardiac muscle. If the muscle is unable to contract with the necessary force to eject blood, the heart rate will increase in compensation to maintain the cardiac output needed for organ function. (See Figure 1.) Conditions that are known to decrease contractility include myocardial ischemia/infarction, cardiomyopathies, decompensated heart failure, and cardiogenic shock.11
Figure 1. Formula for Cardiac Output10 |
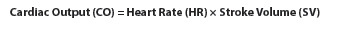 |
Oxygen Carrying Capacity
Additionally, another physiologic component that is implicated in tachycardia is the oxygen carrying capacity of blood. When looking at the formula, the main components that affect the arterial oxygen carrying capacity include the amount of oxygen that can be bound to hemoglobin as well as the amount of oxygen dissolved in blood. (See Figure 2.) When the blood oxygen content is decreased, the heart may attempt to compensate by increasing the heart rate. Conditions such as anemia, which decrease the hemoglobin, or other hematologic conditions that lead to abnormal or poorly functioning hemoglobin, can lead to decreased oxygen carrying capacity.12
Figure 2. Formula for Arterial Oxygen Content11 |
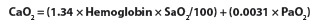 |
SaO2 = arterial hemoglobin oxygen saturation; PaO2 = partial pressure of oxygen |
Toxicologic conditions, such as methemoglobinemia and carbon monoxide poisoning, also can lead to decreased oxygen carrying capacity. Given the importance of the pulmonary system in gas exchange and oxygenating blood, primary pulmonary conditions such as pneumonia, pulmonary fibrosis, and COPD lead to decreased oxygenation of the blood and can lead to a tachycardic presentation.8,9
Sympathetic Stimulation
As an appropriate physiologic response to stress states, tachycardia is the result of increased sympathetic stimulation to increase cardiac output. By increasing the heart rate, the body attempts to compensate for decreases in stroke volume and to meet increased metabolic demands.
The three main mechanisms of tachydysrhythmias are re-entry, abnormal automaticity, and triggered activity.
Re-entry. Re-entry tachycardia is a self-sustaining cardiac rhythm in which the action potential propagates in a circular closed loop manner.13 This mechanism is a disorder of impulse conduction rather than one of impulse generation. In normal conduction, the action potential is initiated in the sinoatrial node and travels via atrial pathways down to the atrioventricular (AV) node and via the His-Purkinje system to the ventricular myocardium.13 Re-entry circuits can be located in atrial or ventricular myocardium, in the AV node, and in a circuit created by an AV bypass tract and the His-Purkinje system.
Re-entry can be caused by a variety of factors, including electrolyte abnormalities, channelopathies, genetic mechanisms, and structural abnormalities that can lead to the formation of scar tissue and cardiac remodeling.13 A re-entry circuit requires two different pathways with different refractory periods for the arrhythmia to initiate, and electrical connections at either end for the arrhythmia to be sustained.13
Re-entry is initiated by a premature beat occurring in the presence of a circuit that has one refractory and one non-refractory limb. The impulse travels through the non-refractory limb, depolarizes the myocardium, and subsequently travels through the previously refractory limb. If the conduction characteristics and refractory periods of the two limbs are complementary, an electrical signal can be sustained around this loop with repetitive depolarization of the atria and ventricles.
Re-entry has been implicated in several tachydysrhythmias, such as atrioventricular nodal re-entrant tachycardia (AVNRT), atrioventricular re-entrant tachycardia (AVRT), atrial flutter, and ventricular tachycardia. Evaluation and identification of re-entrant circuits often requires an electrophysiological evaluation.
Enhanced Automaticity. Tachydysrhythmias caused by enhanced/abnormal automaticity have two main points of origin: enhanced automaticity of cells that have pacemaker capabilities and abnormal automaticity in diseased tissue.14 Enhanced automaticity is caused by increased steepness of phase 4 depolarization. (See Figure 3.) This results in premature attainment of the threshold membrane needed for the cell to depolarize.14
Figure 3. Transmembrane Action Potential in Pacemaker Cells |
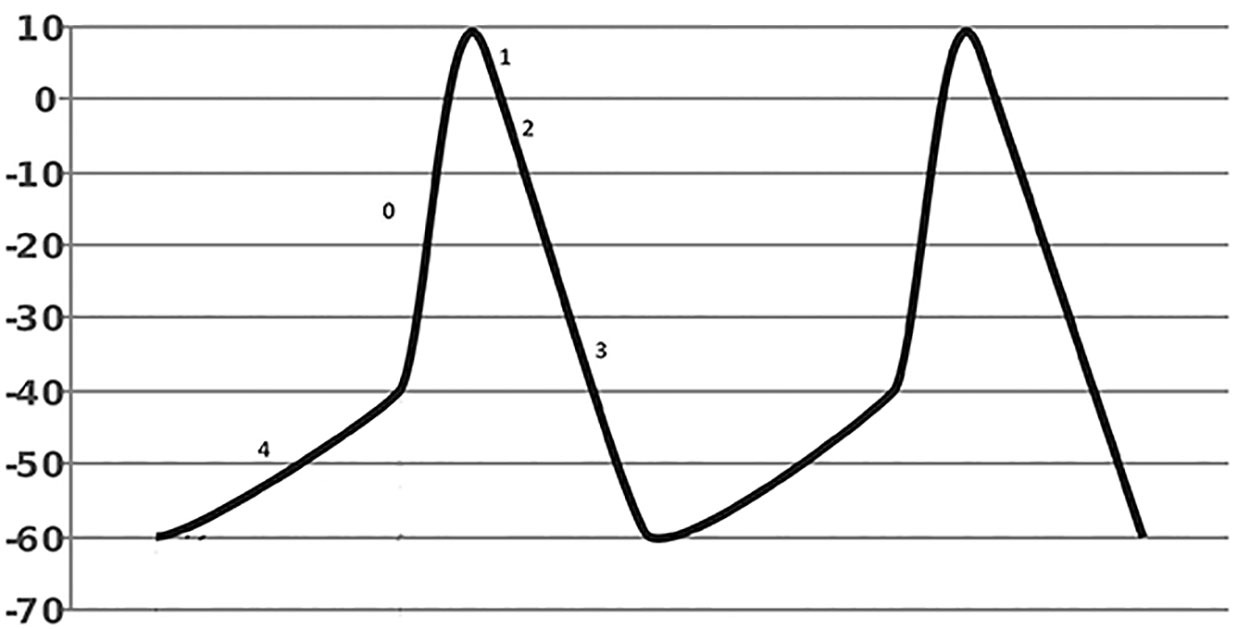 |
Source: Wikimedia Commons. Diberri. Updated July 14, 2009. Figure modified from original. https://creativecommons.org/licenses/by-sa/3.0/deed.en |
Adrenergic stimulation is the main mechanism causing these tachycardias. Abnormal automaticity is defined as spontaneous phase 4 depolarization, which occurs in cells that do not have native pacemaker-like function.14 Commonly, this is seen in cardiac myocytes that have been injured by an ischemic or surgical event.
Triggered Activity. Triggered activity refers to after-depolarizations that can be early or late depending on when they arise in the action potential.14 Triggered activity is different from enhanced/abnormal automaticity in that the depolarizations are not automatic and they are dependent on preceding action potentials.14
Triggered activity and delayed after-depolarizations often are implicated in torsades de pointes (a form of polymorphous ventricular tachycardia found in QT prolongation syndromes) and cyclic-amp-mediated catecholamine surge.15 This leads to the accumulation of intracellular calcium resulting in oscillations of the membrane potential following completion of phase 3 repolarization.14,15
Clinical Features
Given the variety of clinical conditions that can cause tachycardia, it is important to recognize that these patients can have different presentations and chief complaints when presenting to the emergency department. Ultimately, the patient’s complaint and presentation depend on the underlying diagnosis as well as the severity of illness. The first step in the evaluation of every patient presenting with tachycardia is to obtain a full set of vital signs.
The combination of tachycardia and hypotension, typically described as a systolic blood pressure less than
90 mmHg, is an indicator of serious illness and may represent a shock state requiring emergent resuscitation.10 Additionally, the presence of fever, hypoxemia, or tachypnea can be indicative of systemic illness, such as sepsis, and help to guide additional diagnostic and therapeutic interventions.10
Subsequently, the emergency clinician should conduct a detailed history and review of systems for every patient who presents with tachycardia to identify potential underlying etiologies and guide the diagnostic and therapeutic approach. In conjunction with the history and review of systems, performing a detailed physical exam is paramount in the evaluation of the tachycardic patient to guide the diagnostic workup and therapeutic approach.
The next step in evaluation of the tachycardic patient is to obtain an electrocardiogram (ECG). With an ECG, the emergency clinician is able to conduct rhythm analysis and determine the presence of a tachydysrhythmia, which can guide the diagnostic and therapeutic approach. Importantly, obtaining an ECG allows the emergency clinician to conduct a rhythm analysis to determine the presence of a tachydysrhythmia.
The ECG should be inspected to determine the ventricular rate and assess whether the tachycardia is supraventricular or ventricular in nature. Classic tachydysrhythmias have a characteristic ventricular rate, but the overlap is such that the rate alone cannot be used for diagnostic purposes. Supraventricular tachydysrhythmias generally have a narrow or normal QRS complex (QRS duration < 120 msec) because depolarization of the ventricles most often is via a healthy His-Purkinje system.
Tachydysrhythmias with a wide QRS complex can be ventricular in origin or supraventricular in origin with aberrant conduction through the ventricles, termed aberrant infranodal conduction. The distinction between supraventricular tachycardia (SVT) with aberrant conduction and ventricular tachycardia can be challenging and will be discussed later in this article.
Analysis of the PR interval, QRS duration, and QT interval can serve as important diagnostic indicators about the presence of aberrant conduct due to conditions such as Wolff-Parkinson-White (WPW) syndrome, bundle-branch blocks, toxidromes such as tricyclic antidepressant overdose, and electrolyte derangements related to potassium, calcium, and magnesium levels.16,17
Assessing the ST segment and the T waves across leads can be early indicators of conditions such as cardiac ischemia.18 Of all the diagnostic modalities available, the ECG serves as one of the most powerful tools in when assessing the tachycardic patient.
At the discretion of the emergency clinician, additional laboratory tests and imaging may aid in the diagnostic workup. In the correct clinical setting, tests such as a basic metabolic panel, magnesium and phosphorus levels, complete blood count, thyroid studies, troponin, and imaging can aid in determining the underlying cause of a patient’s tachycardia.19,20
Management
Management of patients presenting to the emergency department with tachycardia is centered on using the history, physical examination, and diagnostic approach to guide therapeutics and resuscitation. A unique aspect of management of the tachycardic patient is determining whether the tachycardia is caused by underlying illness or whether the tachycardia is a result of the primary tachydysrhythmia. Early identification of tachydysrhythmias is important to guiding therapeutic approach and illustrates the utility of obtaining an ECG in an undifferentiated tachycardic patient.
Management of Tachydysrhythmias
Vagal Maneuvers. The term vagal maneuver encompasses a variety of techniques that are employed to abruptly and transiently increase vagal parasympathetic tone and slow conduction through the AV node.21 Vagal maneuvers are useful for two purposes: terminating or converting tachydysrhythmias where the AV node is involved in the sustained re-entry circuit and slowing conduction through the AV node to assist in the diagnosis of those arrhythmias of supraventricular origin. Vagal maneuvers also may be useful in distinguishing supraventricular tachycardia from ventricular tachycardia by slowing the rate of conduction in the AV node.21 (See Figure 4.)
Figure 4. Rhythm Strip Showing Transient Atrioventricular Block from Carotid Sinus Massage |
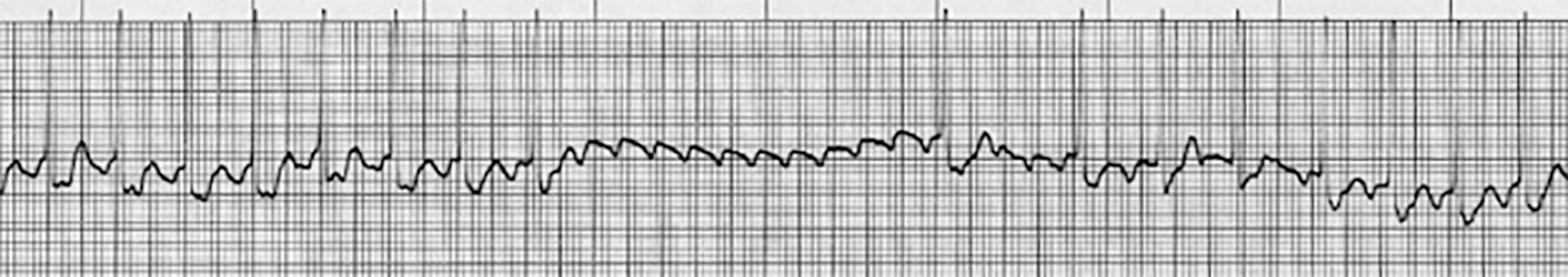 |
The flutter waves are more visible during the transient AV block. Source: Courtesy of J. Stephan Stapczynski, MD. |
When used early in appropriate patients, vagal maneuvers have been documented to have a success rate of 20% to 40% of conversion back into sinus rhythm for SVT tachydysrhythmias.21 These maneuvers have shown the greatest efficacy in AVNRT, AVRT, and atrial tachycardias with re-entrant circuits located within the AV node.21
The Valsalva maneuver was first described in 1936 and is performed by having the patient take in a large breath, hold it in, and bear down with contraction of the chest wall and diaphragm for at least 10 seconds before slowly releasing the air in the lungs. During the strain phase, the increased intrathoracic pressure restricts venous return, and blood pressure falls. During the release phase, the return of blood to the thorax increases stroke volume and the blood pressure increases, stimulating the parasympathetic system. Thus, it is during the release phase that the parasympathetic response is seen. Forceful coughing also can simulate a brief vagal response, although it usually is too short for therapeutic or diagnostic purposes.22
Cold applied to the patient’s face, such as from an ice bag or facial immersion, also can elicit a vagal response.22 This technique is more effective in children compared to adults for conversion of AVNRT or AVRT.
Carotid sinus massage (CSM) is another vagal maneuver performed by pressing and massaging in a small circular motion over the carotid sinus for 10 seconds. This area contains baroceptors that provide feedback to maintain blood pressure and control cardiac output. Stimulation of these receptors causes parasympathetic activation, which slows conduction through the AV node.22
Caution should be used in performing this maneuver. CSM should only be performed over one side at a time, and it should be avoided in elderly patients with vascular disease and audible bruits because it can lead to plaque dislodgement and possible stroke.22
Of the vagal maneuvers described in the literature, the modified Valsalva maneuver has been shown to be the most effective in converting patients back into sinus rhythm along with decreased need for pharmacologic agents.23 The maneuver is performed by having the patient perform a standard Valsalva maneuver while supine by blowing through a 10-mL syringe for 15 seconds during the strain phase and at the end of the strain, their legs raised to a 45-degree angle for 15 seconds during the release phase.23
The investigators in this study measured exhalation pressure and set a target of 40 mmHg.23 Such pressure monitoring may be impractical in an emergency setting, and patients with poor lung capacity or pulmonary disease may not be able to exhale with the required pressure.
Antiarrhythmic Medications
Since the publication of the Vaughan Williams classification of antiarrhythmic medications in the 1970s, there has been an increased understanding of the nuances of cardiac conduction, with several new medications being developed to assist in the management of tachydysrhythmias. (See Table 1.) While a comprehensive review of all medications and mechanisms at the cellular level is outside the scope of this review, it is important for the emergency clinician to understand the fundamentals of cardiac conduction and the therapeutic use of medications in the emergent setting. (See Table 2.)
Table 1. Vaughan Williams Classification of Antiarrhythmic Medications |
|||
Class |
Medication |
Class |
Medication |
IA |
|
III |
|
IB |
|
IV |
|
IC |
|
Other |
|
II |
|
||
Table 2. Commonly Used Antiarrhythmic Medications in the Emergency Department |
|||
Medication |
Uses |
Dosing |
Pharmacokinetics |
Adenosine |
Conversion of AVNRT/AVRT to sinus rhythm |
First dose: 6 mg IV, may give two additional doses of 12 mg IV |
Onset: 20-30 sec Duration: 60-90 sec Half-life: < 10 sec |
Digoxin |
Used in atrial fibrillation/atrial flutter AVNRT/AVRT in patients with decompensated heart failure |
0.5 mg IV then 0.25 mg IV q4 hrs until effective |
Onset: 5-30 min Half-life: 36-48 hrs |
Magnesium sulfate |
Torsades de pointes |
1-2 g IV over 1-2 mins |
Onset: Immediate Duration: 30 min |
Procainamide |
Stable wide complex tachycardia or AVNRT/AVRT |
100 mg IV over 2 mins q 5 mins for a maximum dose of 17 mg/kg. May start infusion at 1-4 mg/min if effective |
Onset: 5-10 min Half-life: 2.5-4.7 hrs |
Lidocaine |
Ventricular arrhythmias |
Loading dose: 1-1.5 mg/kg may bolus 0.5-0.75 mg/kg q 5-10 mins until max dose 3 mg/kg |
Onset: 45-90 secs Duration: 10-20 min Half-life: 90-120 min |
Flecainide |
Atrial fibrillation |
200-300 mg PO once |
Half-life: 12-27 hrs |
Esmolol |
Supraventricular tachydysrhythmias |
Bolus 500 mcg/kg IV and start infusion at 50 mcg/kg/min |
Onset: 1-4 min Duration: < 30 min Half-life: 9 min |
Metoprolol |
Supraventricular tachydysrhythmias |
5 mg IV q 5 mins up to 15 mg max |
Half-life: 3-7 hrs |
Amiodarone |
Wide complex tachycardia AVNRT/AVRT |
Vfib/pulseless v-tach: 300 mg IV loading dose with 150 mg prn Stable wide complex tachycardia or AVNRT/AVRT: 150 mg over 10 mins followed by 1 mg/min infusion over 6 hrs |
Half-life: 58 days |
Sotalol |
Ventricular tachycardia |
75-150 mg IV q 12 hrs |
Onset: 2-3 hrs (oral), 5-10 min (IV) Duration: 8-16 hrs Half-life: 12 hrs |
Ibutilide |
Atrial fibrillation/atrial flutter |
Loading dose 1 mg with repeat dose 10 min after if needed |
Onset: 20-30 min Duration: 24 hrs Half-life: 2-12 hrs |
Diltiazem |
Hemodynamically stable supraventricular tachycardias |
Loading: 0.25 mg/kg max 20 mg Consider additional bolus at 0.35 mg/kg max 25 mg after 15 mins Infusion: 5-15 mg/hr |
Onset: 2-3 min Duration: 1-3 hrs Half-life: 3-5 hrs |
Verapamil |
Hemodynamically stable supraventricular tachycardias |
5-10 mg IV with additional 10 mg after 30 mins |
Half-life: 4-20 hrs |
AVNRT: atrioventricular nodal re-entrant tachycardia; AVRT: atrioventricular re-entrant tachycardia; IV: intravenous; PO: orally; Vfib: ventricular fibrillation; v-tach: ventricular tachycardia; prn: as needed |
|||
Pacemaker Cells
In pacemaker cells, there are three distinct phases of ion movement that lead to spontaneous rhythmic depolarization. (See Figure 3.) Phase 4 represents the slow depolarization of pacemaker cells toward the potential threshold and is referred to as the funny current (If). It is achieved by the activation of hyperpolarization-activated cyclic nucleotide gate channels (HCN channels), which allow sodium (Na+) entry into the cell.
Phase 0 represents depolarization and occurs at around -40 mV. At this point, voltage-gated calcium channels open, leading to an influx of calcium (Ca2+). This leads to a faster rate of depolarization and inactivates the HCN channels. Once peak action potential is achieved, Ca2+ channels begin to close, and potassium (K+) channels open, leading to an efflux of potassium ions and repolarization of the membrane.
Additionally, inputs by the sympathetic and parasympathetic nervous system affect heart rate by changing the intervals between impulses.24 While many pharmacologic agents have an effect on the cardiac conduction system, this review will focus on those most commonly used in the emergent setting.
Adenosine
Adenosine is a nucleoside base, which acts on purinergic adenosine receptors throughout the body. For the treatment of tachycardia, it acts on the receptors found within the AV nodal tissue and peripheral vasculature.25 Conduction time within the AV node is slowed by activation of potassium channels, leading to potassium being driven out of the cell, which inhibits calcium influx.25
Adenosine is recommended as a first-line medication in specific re-entrant tachycardias involving the AV node, including AVNRT, orthodromic AVRT, and antidromic AVRT. Given that antidromic AVRT is wide complex, the diagnosis should be certain, and adenosine should not be given in cases of ventricular tachycardia.25
Adenosine has a rapid onset of action and a half-life of less than 10 seconds. Side effects and symptoms also are relatively short-lived. The common adverse effects include skin flushing, lightheadedness, nausea, sweating, nervousness, numbness, and a feeling of impending doom; however, these effects are very transient. More serious but less common adverse effects include cardiac arrhythmias, premature atrial and ventricular contractions, AV block, cardiac ischemia, hypotension, and prolonged asystole.
Its use is contraindicated in patients with known hypersensitivity to adenosine, patients with clinically active bronchospasm, and patients with known accessory pathways, such as WPW syndrome.
Patients with WPW can have adenosine-sensitive or insensitive pathways, which are identified by electrophysiologic studies. These studies obtain information regarding location, SVT inducibility, local AV interval, and interval from delta wave onset to ventricular activation. Approximately 15% of patients have been shown to have adenosine-sensitive WPW.
Since determining the properties of the accessory pathway is outside the scope of the emergency clinician, it is advised to avoid this medication altogether in patients with WPW when they present to the emergency department with tachydysrhythmias.25,26
Class I Antiarrhythmic Medications
Class I medications bind to sodium channels and have effects on phase 0 depolarization, the action potential duration, and refractory period.
Class IA antiarrhythmic medications diminish the sodium influx, prolong the cardiac action potential, and increase the refractory period through intermediate association/dissociation.24 In the emergency department, procainamide is the most used agent from this class specifically to treat supraventricular tachycardia in the setting of WPW.24 Other drugs in this class, including quinidine, ajmaline, and disopyramide, have limited use in the emergency setting.
Class IB antiarrhythmic medications work similarly to class IA but are known to have fast association/dissociation.24 In the emergency department, lidocaine is the medication most commonly used from this class for treatment of ventricular tachydysrhythmias according to the Advanced Cardiac Life Support (ACLS) guidelines.24 Other medications in this class include mexiletine, phenytoin, and tocainide.24
Class IC antiarrhythmic medications have the slowest association/dissociation with sodium channels affecting the slope of phase 0 depolarization, with no effect on action potential duration or refractory period.24 Drugs in this class, including flecainide, propafenone, encainide, and moricizine, have limited application in the emergency setting. However, patients may be chronically on these oral medications to prevent both supraventricular and ventricular tachydysrhythmias through their impact on ectopic activity and re-entry.24
Class II Antiarrhythmic Medications
Class II medications block the beta-adrenergic receptors affecting the automaticity of the SA and AV nodes. Beta-blockers commonly used in the emergency department include esmolol and metoprolol, which work by inhibiting the G protein-mediated effects of cyclic-AMP specific in cardiac tissue. Beta-blockers are used in the management of a wide variety of both supraventricular and ventricular tachydysrhythmias because of their effects on automaticity, ectopy, triggered activity, and re-entry.24
Isoproterenol is a beta agonist and can be used in the emergency setting as a treatment option for the torsades de pointes variant of polymorphic ventricular tachycardia. By increasing the heart rate, this medication counteracts the later depolarizations seen with prolonged QT syndrome, preventing relapses and maintaining sinus rhythm.24
Digoxin is another class II medication and works by directly binding to the sodium-potassium channel on the myocardium. This leads to increased calcium levels within the cardiac myocyte, leading to prolongation of phase 0 and phase 4 depolarization.24 Within the AV node, this medication slows conduction through its effect on the parasympathetic nervous system.24 Digoxin can be used to treat supraventricular tachydysrhythmias in the emergency department in conditions such as decompensated heart failure where beta-blockers are contraindicated.24
Class III Antiarrhythmic Medications
Class III medications affect cardiac potassium channels and prolong phase 3 repolarization. This results in prolonged myocyte recovery, an increased refractory period, and a prolonged QT interval on the ECG.24 In emergent settings, amiodarone is a class III medication used in treating patients with ventricular tachycardia. Patients also may be on this medication to prevent paroxysmal atrial fibrillation.24 Of note, amiodarone also has class I, II, and IV activity.
Other medications in this class include ibutilide and dofetilide, which can be used in the treatment of supraventricular tachydysrhythmias.24 Sotalol, another medication in this class, may be used for the treatment of ventricular tachycardia in the emergency department.24
Class IV Antiarrhythmic Medications
Class IV medications are calcium channel blockers that inhibit L-type calcium channels, which results in inhibition of SA node pacing and AV nodal conduction. The two most common medications used in this class in the emergency department are verapamil and diltiazem, which are used to achieve ventricular rate control in supraventricular tachydysrhythmias, such as atrial fibrillation.24
Electrical Cardioversion and Defibrillation
When tachydysrhythmias fail to respond to pharmacologic treatment or the patient presents with unstable vital signs, the treatment of choice is electrical cardioversion. This can be performed as a synchronized cardioversion or electrical defibrillation. Per the American Heart Association ACLS guidelines, defibrillation is indicated in patients who present with pulseless ventricular tachycardia or ventricular fibrillation.
A defibrillatory shock can be delivered either by placing manual paddles or adhesive pads connected to the patient’s right anterior chest and lower left chest in the mid-axillary line.27 The recommended energy level is 200 J in biphasic automated external defibrillators (AEDs) with adherence to the ACLS guidelines.
Synchronized cardioversion is the first-line treatment for all tachycardic rhythms in which a patient has a pulse but is considered unstable. These patients will be considered unstable in the emergency setting because of chest pain, dyspnea, altered mental status, hypotension, pulmonary edema, or ischemic changes noted on the ECG.27
Synchronized cardioversion differs from defibrillation in two key aspects: The amount of energy needed to convert the rhythm usually is less, and the shock is delivered in a different part of the cardiac cycle. Pads are placed in a similar position, and the AED should be placed in “synchronize” mode, which will cause the monitor to track the R wave of each QRS complex. The shock will be delivered during the QRS complex (usually 40 msec after the peak of the R wave) to avoid the R-on-T phenomenon.
The recommended energy level for cardioversion ranges from 50 J to 200 J. The safest recommendation is to start at 50 J and to double the amount of energy used if unsuccessful to a maximum of 200 J.27
Additional Aspects and Challenges for the Emergency Clinician
Identifying Ventricular Tachycardia
One of the most challenging aspects that emergency clinicians face in the care of the tachycardic patient is rhythm analysis. Identification of ventricular tachycardia and differentiating it from supraventricular tachydysrhythmias with ventricular aberrancy remains one of the challenges at the forefront of emergency care. While many stepwise electrocardiographic algorithms exist to aid in differentiation, individual criteria have limitations in their sensitivity, specificity, and predictive value.28 Implementation of various algorithms and criteria still leads to misdiagnosis in the emergency department.28
Several confounding factors have been identified in the misdiagnosis of ventricular tachycardia in the emergency department, including but not limited to stability of the patient, past medical history, variety in electrocardiographic morphology, and clinical maneuvers employed by the clinician.28 While the detailed review of every stepwise algorithm is outside the scope of this review, it is important for the emergency clinician to understand how to identify atrioventricular dissociation and how to treat ventricular tachycardia.
Supraventricular Tachycardia
In patients who present to the emergency department with documented AVNRT or AVRT, the utility of testing has come under scrutiny in recent years. Unnecessary investigation can be burdensome and lead to an increase in invasive testing and adverse outcomes without a change in clinical management.29 In the case of AVNRT or AVRT, studies have shown that troponin studies, thyroid studies, blood counts, and chest X-ray seldom led to a change in management or to the identification of an underlying cause of the patient’s tachydysrhythmias.29
Atrial Fibrillation/Flutter
Another area of research in recent years has been the emergency management of patients who present in atrial fibrillation. An increasing number of studies have been conducted to identify patients who do not require inpatient management. Meta-analysis has shown that clinical decision tools, such as the RED-AF and AFFORD tools, allow the clinician to identify patients at risk for adverse outcomes if discharged, with a heavy emphasis placed on the ability to obtain close follow-up.30
Studies also show that if the arrhythmia is present for 48 hours or less, electrical cardioversion has a greater success rate than chemical cardioversion.30 When comparing chemical cardioversion, electrical cardioversion, and rate control strategies, each group represented a similarly low rate of adverse events and can serve as a viable treatment option. While conversion to normal sinus rhythm may seem desirable, these studies show that if the patient is adequately rate controlled and asymptomatic, discharge from the emergency department still is a reasonable option.30
Anticoagulation of the Patient with Atrial Fibrillation/Flutter
An additional consideration in the treatment of atrial fibrillation/flutter for the emergency clinician is the initiation of oral anticoagulation. Stroke remains one of the most devastating complications of these tachydysrhythmias, leading to a greater propensity for disability, increased healthcare costs, and long-term rehabilitation.31,32 Multiple studies have shown that initiation of oral anticoagulation is underused in the emergency department and represents a potential area of improvement for the emergency management of atrial fibrillation/flutter.
Current guidelines advocate for the use of both the CHA2DS2-VASc and HAS-BLED risk stratification scores to determine which patients would benefit from initiation of oral anticoagulation.31-33 Many factors, such as polypharmacy, perceived risk of falls, and difficulty arranging follow-up, have been shown to be barriers in emergency department initiation of anticoagulation. To mitigate this, increased research is being conducted in developing protocols to assist with optimization of rhythm management and initiation of anticoagulation in the emergency department.32,33
Electrical Storm
Electrical storm is a life-threatening situation defined as three or more episodes of sustained ventricular tachycardia, ventricular fibrillation, or shocks from an implanted cardioverter defibrillator within 24 hours.34 It is associated with significant morbidity and mortality and often is refractory to standard ACLS treatment.34
Initial treatment centers on the use of beta-blockade to reduce sympathetic tone. In this situation, repeat doses of epinephrine are not recommended, since this can cause an increase in sympathetic stimulation. Additional treatment centers on identifying underlying causes, such as correction of electrolyte abnormalities and use of isoproterenol in patients with Brugada syndrome.34 Amiodarone remains the rhythm control agent of choice and shows decreased rates of ventricular arrhythmias and shocks when used in conjunction with beta-blockade.30
The use of double sequence defibrillation (DSD) has shown success in case reports, with some studies reporting improved outcomes when used early in resuscitation.34 With the increasing presence of ultrasound in emergency departments around the world, one potential option for the emergency clinician in cases of refractory ventricular tachydysrhythmias is the stellate ganglion block.34,35 When performed correctly, it has been shown to successfully block sympathetic stimulation to the heart and abate refractory ventricular tachydysrhythmias. Increased research is needed to understand the role of operator dependence on success and the rate of adverse outcomes.35
Summary
Patients who present to the emergency department with tachycardia have a wide variety of potential problems. The differential diagnosis can be broad, ranging from the relatively benign to fulminant shock requiring medication and admission to the intensive care unit. Identifying patients with systemic illness and conducting a thorough evaluation remain at the forefront of importance for the emergency clinician.
For primary tachydysrhythmias, it is important for the emergency clinician to appropriately use information obtained from the ECG to guide evaluation and management strategies. By understanding the mechanism of tachycardia and how to use diagnostic testing to our advantage, managing these patients becomes more straightforward.
REFERENCES
- Finsterer J, Wahbi K. CNS-disease affecting the heart: Brain–heart disorders. J Neurol Sci 2014;345:8-14.
- Benarroch EE. Physiology and pathophysiology of the autonomic nervous system. Continuum (Minneap Minn) 2020;26:12-24.
- Doubleday AR, Sippel RS. Hyper-thyroidism. Gland Surg 2020;9:124-135.
- Ertek S, Cicero AF. Hyperthyroidism and cardiovascular complications: A narrative review on the basis of pathophysiology. Arch Med Sci 2013;9:944-952.
- Lindow T, Pahlm O, Ljungström E. Pheochromocytoma – An ECG diagnosis? J Electrocardiol 2020;58:7-9.
- Zhang J, Yang J, Liu L, et al. Significant abnormal glycemic variability increased the risk for arrhythmias in elderly type 2 diabetic patients. BMC Endocr Disord 2021;21:1-8.
- Muneer M, Akbar I. Acute metabolic emergencies in diabetes: DKA, HHS and EDKA. In: Islam MS, ed. Diabetes: From Research to Clinical Practice, Volume 4. Springer International Publishing; 2021:85-114.
- Hobohm L, Becattini C, Ebner M, et al. Definition of tachycardia for risk stratification of pulmonary embolism. Eur J Intern Med 2020;82:76-82.
- Goedemans L, Abou R, Montero-Cabezas JM, et al. Chronic obstructive pulmonary disease and risk of atrial arrhythmias after ST-segment elevation myocardial infarction. J Atr Fibrillation 2020;13:2360.
- Vincent JL. Understanding cardiac output. Crit Care 2008;12:174.
- Kislitsina ON, Rich JD, Wilcox JE, et al. Shock - Classification and pathophysiological principles of therapeutics. Curr Cardiol Rev 2019;15:102-113.
- Rhodes CE, Denault D, Varacallo M. Physiology, oxygen transport. In: StatPearls [Internet]. Updated Nov. 14, 2022. StatPearls Publishing; 2022.
- Goyal A, Basit H, Bhyan P, Zeltser R. Reentry arrhythmia. In: StatPearls. Updated July 4, 2023. StatPearls Publishing; 2023.
- Stahmer SA, Cowan R. Tachy-dysrhythmias. Emerg Med Clin North Am 2006;24:11-40, v-vi.
- Riggins J Jr, Douglas T, deSouza IS. Ventricular tachycardia as a consequence of triggered activity. Am J Emerg Med 2021;44:480.e5-480.e7.
- Kardalas E, Paschou SA, Anagnostis P, et al. Hypokalemia: A clinical update. Endocr Connect 2018;7:R135-R146.
- Negru AG, Pastorcici A, Crisan S, et al. The role of hypomagnesemia in cardiac arrhythmias: A clinical perspective. Biomedicines 2022;10:2356.
- Bhatt DL, Lopes RD, Harrington RA. Diagnosis and treatment of acute coronary syndromes: A review. JAMA 2022;327:662-675.
- Go MT, George AM, Tahsin B, Fogelfeld L. Tachycardia in hyperthyroidism: Not so common. PLoS One 2022;17:e0273724.
- Riley LK, Rupert J. Evaluation of patients with leukocytosis. Am Fam Physician 2015; 92:1004-1011.
- Niehues LJ, Klovenski V. Vagal maneuver. In: StatPearls [Internet]. Updated July 3, 2023. StatPearls Publishing; 2023.
- Mahtani AU, Nair DG. Supraventricular tachycardia. Med Clin North Am 2019;103:863-879.
- Appelboam A, Reuben A, Mann C, et al. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): A randomised controlled trial. Lancet 2015;386:1747-1753.
- Lei M, Wu L, Terrar DA, Huang CLH. Modernized classification of cardiac antiarrhythmic drugs. Circulation 2018;138:1879-1896.
- Singh S, McKintosh R. Adenosine. In: StatPearls [Internet]. Updated Sept. 10, 2022. StatPearls Publishing; 2023.
- Beach C, Follansbee CW, Beerman L, et al. Adenosine-sensitive Wolff-Parkinson-White: Longer time across the atrioventricular groove. Pacing Clin Electrophysiol 2018;41:35-41.
- Goyal A, Sciammarella JC, Chhabra L, Singhal M. Synchronized electrical cardioversion. In: StatPearls [Internet]. Updated March 27, 2023. StatPearls Publishing; 2023.
- Farré J, Rubio JM, Sternick EB. Confounding factors leading to misdiagnosing ventricular tachycardia as supraventricular in the emergency room. Indian Pacing Electrophysiol J 2023;23:1-13.
- Fernando H, Adams N, Mitra B. Investigations for the assessment of adult patients presenting to the emergency department with supraventricular tachycardia. World J Emerg Med 2020;11:54-59.
- Vandermolen JL, Sadaf MI, Gehi AK. Management and disposition of atrial fibrillation in the emergency department: A systematic review. J Atr Fibrillation 2018;11:1810.
- Rangnekar G, Gallagher C, Wong GR, et al. Oral anticoagulation therapy in atrial fibrillation patients managed in the emergency department compared to cardiology outpatient: Opportunities for improved outcomes. Heart Lung Circ 2019;28:e43-e46.
- Do DH, Bernardes-Souza B, Merjanian M, et al. Development of a care pathway for atrial fibrillation patients in the emergency department. Crit Pathw Cardiol 2022;21:105-113.
- Miller RJH, Chew DS, Rezazadeh S, et al. Factors influencing oral anticoagulation prescription for patients presenting to emergency departments with atrial fibrillation and flutter. Can J Cardiol 2018;34:804-807.
- Dyer S, Mogni B, Gottlieb M. Electrical storm: A focused review for the emergency physician. Am J Emerg Med 2020;38:1481-1487.
- Savastano S, Schwartz PJ. Blocking nerves and saving lives: Left stellate ganglion block for electrical storms. Heart Rhythm 2023;20:1039-1047.
This issue completes the two-part series on tachycardia. This issue will finish the discussion of additional causes of tachycardia, address management, and conclude by covering some challenging issues with this arrhythmia.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
