Tachycardia in the Emergency Department: Part I
October 15, 2023
Related Articles
AUTHOR
Rahul Rege, MD, Assistant Professor of Emergency Medicine, Penn State Health Milton S. Hershey Medical Center, Hershey, PA
PEER REVIEWER
Frank LoVecchio, DO, FACEP, Vice-Chair for Research, Medical Director, Samaritan Regional Poison Control Center, Emergency Medicine Department, Maricopa Medical Center, Phoenix, AZ
EXECUTIVE SUMMARY
- Tachycardia is a common finding in the emergency department, seen in up to 55% of patients.
- Tachycardia is closely tied to the interconnection between the heart and the sympathetic nervous system.
- While pain can increase the heart rate, there is a poor correlation between the patient’s self-reported severity of pain and the heart rate.
- Decompensated valvular heart disease produces a compensatory tachycardia in an attempt to restore cardiac output.
- Concomitant beta-blocker use may result in the absence of tachycardia expected in acute exacerbations of chronic heart failure.
- Postural orthostatic tachycardia syndrome is characterized by an increase in heart rate of greater than 30 beats per minute upon standing associated with lightheadedness or fainting without orthostatic hypotension.
- Acute atrial fibrillation is defined by an onset within the past 48 hours.
- Atrial flutter typically has an atrial rate of 300 beats per minute, with the most common ventricular rate of around 150 beats per minute as a result of a 2:1 atrioventricular block.
- Atrioventricular reciprocating tachycardia usually presents with orthodromic conduction and a narrow QRS complex during the arrhythmia.
- Wide QRS complex tachycardias can originate either from the ventricle (ventricular tachycardia) or above the atrioventricular node (supraventricular tachycardia with aberrant conduction).
- With a wide complex tachycardia, very wide QRS complexes (> 160 msec) and negative QRS deflection in all the precordial leads (“negative concordance”) suggest the rhythm is ventricular tachycardia as opposed to supraventricular tachycardia with aberrancy.
- Torsades de pointes is a form of polymorphic ventricular tachycardia caused by the long QT syndrome.
- Ventricular fibrillation (VF) can be a primary event (sudden change from sinus rhythm to VF) or be the result of sustained ventricular tachycardia that deteriorates into VF.
This issue is the first of a two-part discussion of tachycardia, the most common rhythm abnormality seen in the emergency department. Part I will discuss the epidemiology, etiology, and characteristics of the different tachycardic arrhythmias. Part II will discuss conditions affecting other organ systems that can produce tachycardia, then finish by reviewing the assessment and management of these patients. We hope these two issues will be useful to your clinical practice.
— J. Stephan Stapczynski, MD, Editor
Introduction
Emergency providers evaluate and treat a wide variety of clinical presentations, from minor concerns to life-threatening emergencies. When a patient first presents to an emergency department (ED), the initial step in the triage process involves obtaining vital signs as well as a chief complaint. In adult patients, tachycardia is defined as a heart rate greater than 100 beats per minute and, in conjunction with the other vital signs, can provide clinically significant information about the severity of a patient’s illness.1 The presence of tachycardia is associated with increased morbidity and mortality in a wide variety of patient populations with varying clinical presentations.2-4
Diagnostically, the tachycardic patient presents several challenges to the emergency provider given the sheer diversity in clinical presentation and severity of illness. The purpose of this article is to discuss best practice strategies when evaluating the tachycardic patient in the ED, with special attention to diagnostic and therapeutic approaches. This article also will emphasize the importance of rhythm analysis in patients with tachydysrhythmias as well as clinical red flags and their importance when risk-stratifying the tachycardic patient to determine the severity of illness and disposition.
Epidemiology
Tachycardia is one of the most common vital sign abnormalities in patients who present to the ED, with studies reporting an incidence as high as 54.8%.5 Tachycardia can present as a manifestation of many potential diagnoses with a variety of chief complaints. In general, tachycardia is associated with increased morbidity and mortality in patients of all ages.6,7
Etiology
When evaluating patients with tachycardia, it is important to consider the interconnection between the heart and the sympathetic nervous system. Any physiologic or pathologic state that leads to increased catecholamine secretion can cause tachycardia. The challenge for the emergency provider lies in identifying a cause based on evaluation, determining the severity of illness, and deciding on appropriate therapeutic interventions. Given the innumerable causes of tachycardia that have been reported, this article will attempt to focus on those most pertinent to the emergency provider, ranging from the benign to the life-threatening.
Anxiety/Heightened Emotional State
Anxiety-related conditions account for more than 1 million ED visits annually in the United States, but alone, infrequently require hospitalization.8 When considering the tachycardic anxious patient, it is imperative for the emergency provider to first consider alternative causes and to be wary of patients who present to the ED with this isolated complaint. Often, anxiety or a heightened emotional state can be a side effect of a systemic medical condition, and alternative diagnoses must be considered before arriving at this conclusion.9,10
It is hypothesized that heightened emotional states have a neuro-modulative effect on visceral body systems, and while several theories have been proposed, further research is needed to understand the exact biochemical pathways implicated in these phenomena.10 In the emergent setting, anxiety as a cause of a patient’s tachycardia should be considered a diagnosis of exclusion after a thorough medical workup has been conducted.
Pain
Acute pain causes a stress response within the body, which can lead to increased heart rate.11 Studies have shown an increase in heart rate of healthy persons when exposed to noxious stimuli; however, the relationship between pain and heart rate appears to vary across individuals. While pain can have a powerful effect on heart rate, studies in the ED show that self-reported pain scores as well as changes in self-reported pain intensity do not directly correlate with a patient’s heart rate.12,13
The diagnostic and therapeutic approach in the ED should be catered to each individual, and it is important to determine the cause of pain. If a life-threatening cause of pain is not identified, treatment of the pain with adequate analgesia may lead to resolution of the tachycardia.
Substance Use/Withdrawal
Routine use of legal as well as illicit substances has been known to cause tachycardia. Alcohol has been known to cause tachycardia through increased sympathetic activity and by precipitating cardiac conduction delays.14,15 Patients with alcohol use disorder who develop a physiologic dependence also can develop tachycardia in withdrawal through glutamate neurotoxicity and down regulation of GABA-A receptors.16
Nicotine also can cause tachycardia through its effect on the sympathetic nervous system and on oxidative stress and inflammation.17 Caffeine, another commonly used substance, can cause tachycardia through its effect on phosphodiesterase inhibition.15 Cannabis and use of exogenous cannabinoids also have been implicated in causing tachycardia through adrenergic activity and increase in ectopy.15
Illicit substance use is at an all-time high, with the United States having one of the highest rates of stimulant and opiate use worldwide.18 Cocaine and amphetamine use can lead to direct sympathomimetic stimulation through release of neurotransmitters leading to tachycardia.15 With the opioid epidemic, patients who present to the ED with withdrawal also can manifest tachycardia.15
Medications
Even with appropriate therapeutic use, several medications have been implicated in eliciting tachycardia as an unwanted side effect. Medications from a wide variety of classes have been found to cause tachycardia, including anti-cancer agents, anticonvulsants, anti-inflammatory medications, bronchodilators, antiarrhythmics, and antipsychotics.15 (See Table 1.)
Table 1. Classes of Medications Known to Cause Tachycardia15 |
|
Some of the mechanisms causing tachycardia include direct effects on cardiac conduction, sympathetic stimulation, parasympathetic inhibition, receptor modulation, and cytotoxic effects.15 In extreme cases, patients can present with classic toxidromes due to sympathomimetics or anticholinergics, as well as life-threatening conditions such as neuroleptic malignant syndrome or serotonin syndrome.
Tachycardia in Cardiovascular Disease
Pericarditis/Myocarditis
Pericarditis is defined as inflammation of the pericardial sac. By definition, the cardiac myocytes remain undamaged; however, pain caused by this condition may contribute to tachycardia. If tachycardia is present and pericarditis is suspected, it is important to consider a concomitant myocarditis.19
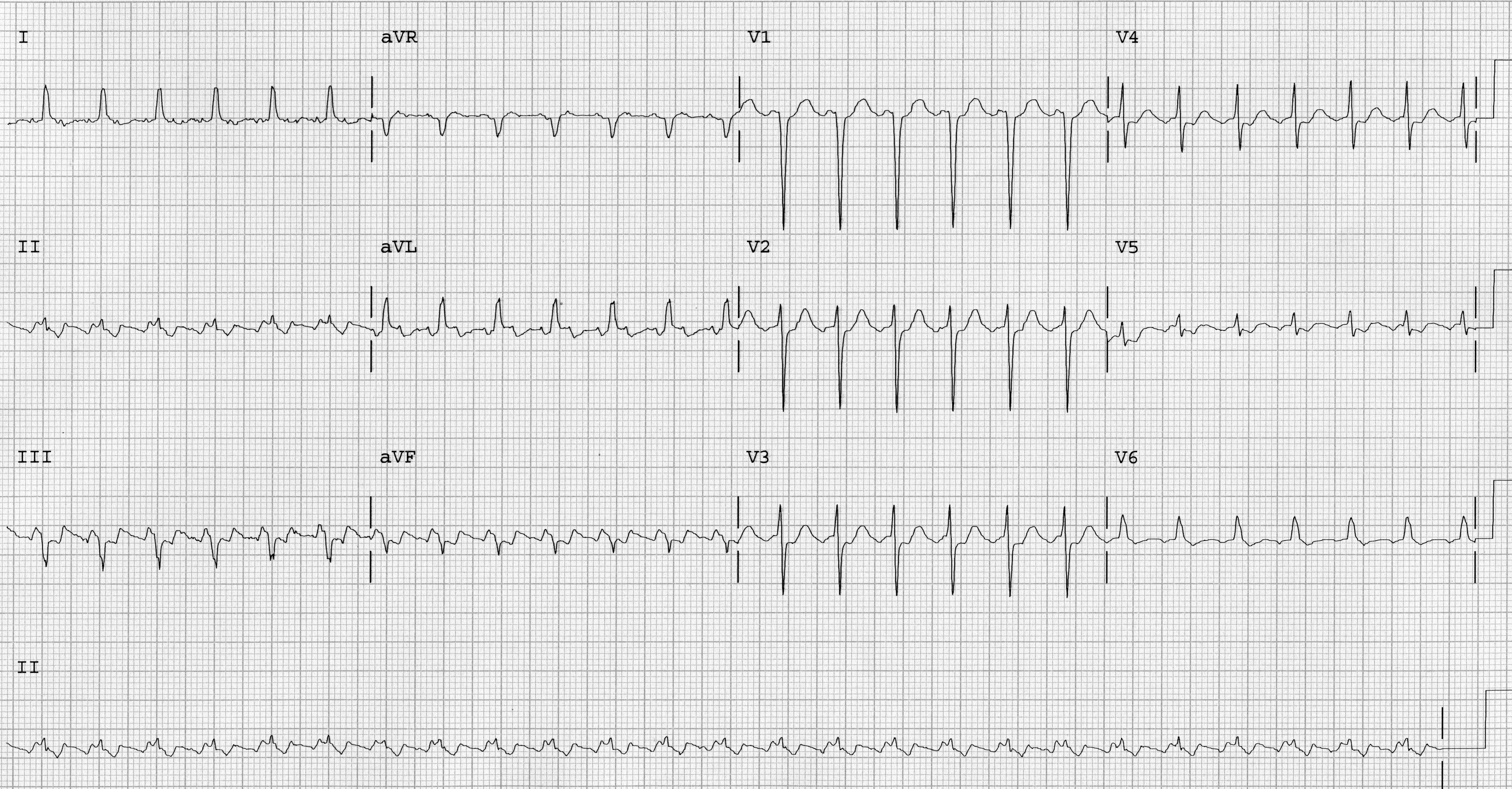
Myocarditis is characterized by inflammatory changes within the myocardium that produce myocyte degeneration and necrosis without concomitant ischemia.20 Myocarditis usually is caused by an infectious process, but it also may be caused by medication, such as doxorubicin and cocaine use. With no pathognomonic presentation, this illness represents a diagnostic challenge to the emergency provider and requires a high index of clinical suspicion.20 Classic electrocardiogram (ECG) changes in early pericarditis are PR depression noted in leads I, II, III, and avF with diffuse ST elevations.20 (See Figure 1.)
Figure 1. Electrocardiogram of Early Pericarditis |
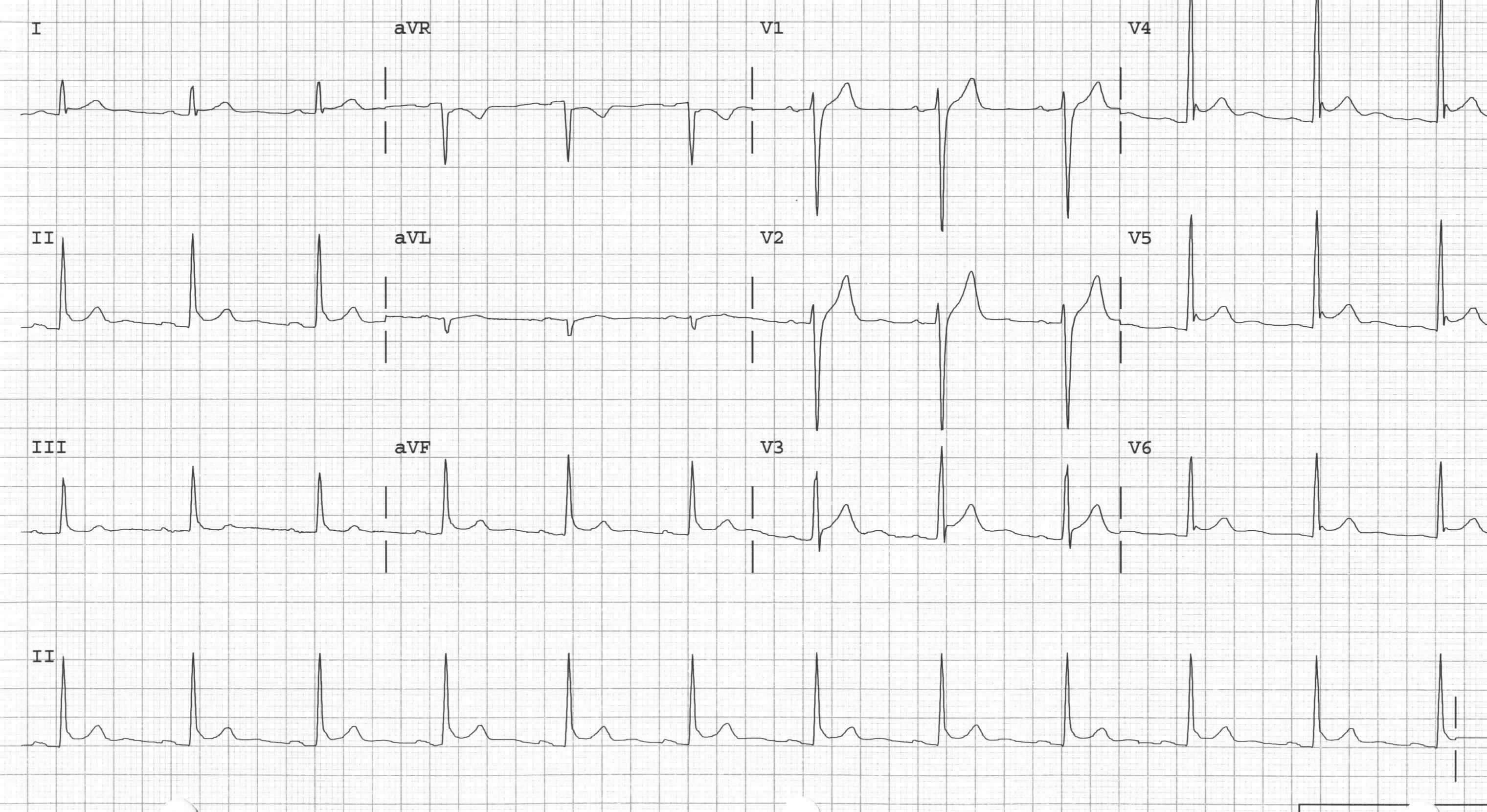 |
12-lead electrocardiogram of early pericarditis showing PR depression in leads II, III, and avF and diffuse precordial ST elevations Image courtesy of J. Stephan Stapczynski, MD |
Valvular Pathology
Aortic Stenosis
Aortic stenosis produces significant narrowing of the aortic valve resulting in impairment of left ventricular output. The major causes of aortic stenosis include calcification, rheumatic disease, and congenital abnormalities.21 Critical aortic stenosis can cause tachycardia in patients by decreasing left ventricular preload and increasing afterload.21 The body attempts to compensate by increasing the heart rate to maintain cardiac output.21
Aortic Regurgitation
Aortic regurgitation is defined by retrograde flow of blood from the aorta back into the left ventricle.22 Acute aortic regurgitation may occur in the setting of blunt chest trauma, endocarditis, or aortic dissection. Acute aortic regurgitation results in severe volume overload of the left ventricle, and the myocardium is unable to adapt to the change in volume, leading to an increase in pressure during diastole. As cardiac output declines, a compensatory tachycardia develops, leading to a shorter period of diastole in an attempt to restore cardiac output.23
Mitral Stenosis
Mitral stenosis refers to narrowing of the mitral valve causing decreased blood flow from the left atrium to the left ventricle. Rheumatic fever accounts for 80% of all cases globally.24 Prolonged mitral stenosis causes left atrial dilation as well as right heart and pulmonary circulatory dysfunction.25 Left atrial remodeling due to the stenotic valve subsequently can lead to atrial fibrillation, a notable tachydysrhythmia.
Mitral Regurgitation/Mitral Valve Prolapse
Mitral regurgitation refers to an incompetent mitral valve that allows blood back into the left atrium during left ventricular systole and is the most common valvular abnormality worldwide.26 While advancing age is the most common cause of this pathology, connective tissue disease and concomitant heart failure and ischemia also have been associated.26 Acute mitral regurgitation is considered a valvular emergency and is accompanied with life-threatening pulmonary edema and a precipitous drop in cardiac output leading to a compensatory tachycardia.
Mitral valve prolapse (MVP) is a condition where one or more mitral valve leaflets bellows into the atrium during ventricular systole and sometimes can progress to mitral regurgitation. A unique phenomenon known as arrhythmogenic mitral valve prolapse has been described recently in the literature finding that MVP causes changes in ventricular remodeling that can lead to ventricular tachydysrhythmias, such as ventricular tachycardia and ventricular fibrillation.27
Congestive Heart Failure Exacerbation
Heart disease is the leading cause of death in the United States, and it is estimated that more than 6 million adults in the United States currently are living with heart failure.28 While heart failure exacerbation is classically associated with dyspnea on exertion (DOE), orthopnea, and paroxysmal nocturnal dyspnea (PND), tachycardia also can be indicative of a decompensated state.28
Physiologically, decompensated heart failure represents as a mismatch between the metabolic demands of the body and the heart’s ability to supply oxygen-rich blood for function. The heart rate increases in an attempt to compensate for the reduced stroke volume to maintain cardiac output.28 It is important to note that patients who present with exacerbation of known congestive heart failure (CHF) may be chronically taking a beta-blocker medication, which impedes the neuromodulation of the sympathetic nervous system required to produce the compensatory tachycardia.
In patients with CHF, tachydysrhythmias such as ventricular tachycardia and ventricular fibrillation are a source of significant morbidity and mortality.29 It is hypothesized that the effects of heart failure on ventricular remodeling and mechanical stretch may play a role in spontaneous tachydysrhythmia generation.29
Channelopathies
In cases of sudden cardiac death in patients younger than 35 years of age who have a non-conclusive coronary disease at autopsy, it is estimated that 5% to 40% of these deaths are due to inherited channelopathies.30,31 The four that are identified most commonly on genetic testing include long QT syndrome (LQTS), Brugada syndrome, short QT syndrome (SQTS), and catecholaminergic polymorphic ventricular tachycardia (CPVT). Each has its own unique electrocardiographic signature, mode of presentation, and commonly affected genes.
Cardiomyopathies
Cardiomyopathies are characterized by remodeling that occurs of the myocardium, increasing the propensity for tachydysrhythmias. They may be genetic, acquired, or mixed in etiology and are diagnosed with the use of echocardiography or endomyocardial biopsy. (See Table 2.)
Table 2. Cardiomyopathies32 |
||
Genetic |
Mixed |
Acquired |
|
|
|
Tachydysrhythmias
One of the most important steps in the initial evaluation of the tachycardic patient is to obtain an ECG. While the initial vital signs serve to identify the tachycardic patient, the ECG serves to identify the presence of a concomitant tachydysrhythmia. ECG interpretation and rhythm analysis are essential skills of every emergency provider and can assist in diagnosis and treatment of the patient.
Sinus Tachycardia
Sinus tachycardia is the most common type of tachycardia seen in patients. In normal physiology, sinus tachycardia can be seen during and immediately after periods of exercise and stress and serves as an appropriate compensatory response.33
Sinus tachycardia is defined by the presence of a regular rate and rhythm with a ventricular rate higher than 100 beats per minute with the following ECG features: the presence of upright P waves in leads I, II, and avL; a negative P wave in avR; and each P wave is followed by a QRS complex and T wave.33 (See Figure 2.) The QRS complex typically is normal and narrow (QRS duration < 120 msec) unless there is a preexisting conduction abnormality, such as a bundle branch block.
Figure 2. Sinus Tachycardia |
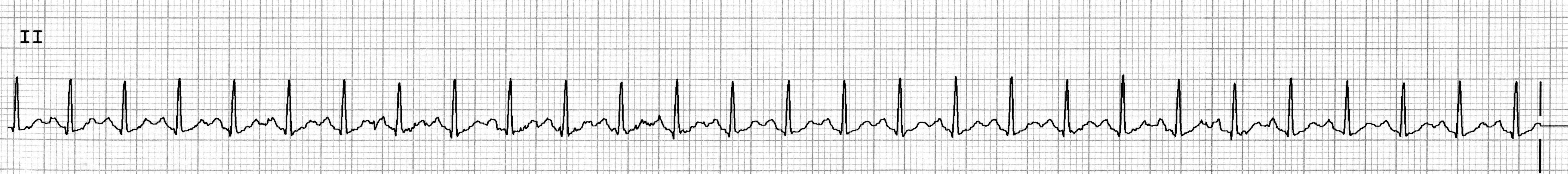 |
Image courtesy of J. Stephan Stapczynski, MD |
Postural Orthostatic Tachycardia Syndrome
Postural orthostatic tachycardia syndrome (POTS) is a multifactorial disorder defined by an increase of greater than 30 beats per minute in heart rate within 10 minutes of a change from supine to upright positioning associated with lightheadedness or fainting in the absence of orthostatic hypotension.34 While making the diagnosis requires outpatient evaluation with subspecialist assistance, this disorder is becoming more prevalent, with 1 million to 3 million people affected in the United States alone.34 It is considered a diagnosis of exclusion in the emergency setting.
Inappropriate Sinus Tachycardia
Inappropriate sinus tachycardia (IST) is defined as a resting heart rate of > 100 beats per minute with an average 24-hour heart rate > 90 beats per minute. The prevalence is reported to be as high as 1% in the middle-aged population, and diagnosis should be made in conjunction with a cardiologist and is a diagnosis of exclusion in ED patients.35
Atrial Fibrillation with Rapid Ventricular Response
Atrial fibrillation (Afib) is a common arrhythmia seen in the ED, with an estimated prevalence of 33.5 million patients in the United States and can be associated with rapid ventricular response when tachycardic.36 The rate classically is described as “irregularly irregular,” and the diagnosis requires the presence of fibrillation waves in place of discernible P waves on the ECG.37 (See Figures 3A and 3B.) This tachydysrhythmia is independently associated with increased risk of stroke, and identification is paramount to the practice of emergency medicine.
Figure 3A. Atrial Fibrillation |
 |
Lead V1, atrial fibrillatory waves at rate > 300 bpm Image courtesy of J. Stephan Stapczynski, MD |
Figure 3B. Atrial Fibrillation |
 |
Lead II, no consistent P waves and irregular ventricular response Image courtesy of J. Stephan Stapczynski, MD |
The chaotic atrial activity in atrial fibrillation typically is at rates greater than 300 beats per minute. Fortunately, the refractory period of the AV node limits the rate at which electrical signals can be transmitted to the ventricles. With a healthy AV node, the ventricular rate in untreated patients with atrial fibrillation is between 120 and 140 beats per minute. Atrial fibrillation most commonly is associated with myocardial diseases, so it is possible to also have a wide QRS complex.
In addition to making the diagnosis, it is important to clarify the duration of symptoms with a dedicated history. Acute atrial fibrillation has an onset within the past 48 hours. Paroxysmal atrial fibrillation occurs intermittently with sinus rhythm, with spontaneous recurrences and terminations. Persistent atrial fibrillation is continuous and sustained, typically greater than seven days, and can be terminated only by pharmacologic treatment or electrical conversion. Permanent atrial fibrillation is a long-term condition, typically longer than 12 months, where conversion to sinus rhythm is either not indicated or ineffective.38
Atrial Flutter
Atrial flutter is another common tachydysrhythmia of the heart and is characterized by a tachycardic atrial rate with a fixed or variable ventricular rate.39 It occurs in the presence of a re-entry mechanism within the atria, which must have the following: areas of fast and slow conduction velocities and different refractory periods of a functional circuit core.38
The typical ECG will show flutter waves with negative P wave direction in the inferior leads, with low amplitude waves in lead I and upright flutter waves in lead avL.40 (See Figures 4A and 4B.) The atrial flutter rate usually is a consistent 300 beats per minute. The ventricular rate is a ratio of the atrial rate, usually 2:1, 3:1, or 4:1, or sometimes a variable ratio.39,40 The ratio of atrial to ventricular rate is due to a functional block within the AV node.
Figure 4A. Atrial Flutter with 2:1 AV Response |
 |
12-lead electrocardiogram of atrial flutter with 2:1 AV response and ventricular rate of 152 beats/min Image courtesy of J. Stephan Stapczynski, MD |
Figure 4B. Atrial Flutter with 4:1 AV Response |
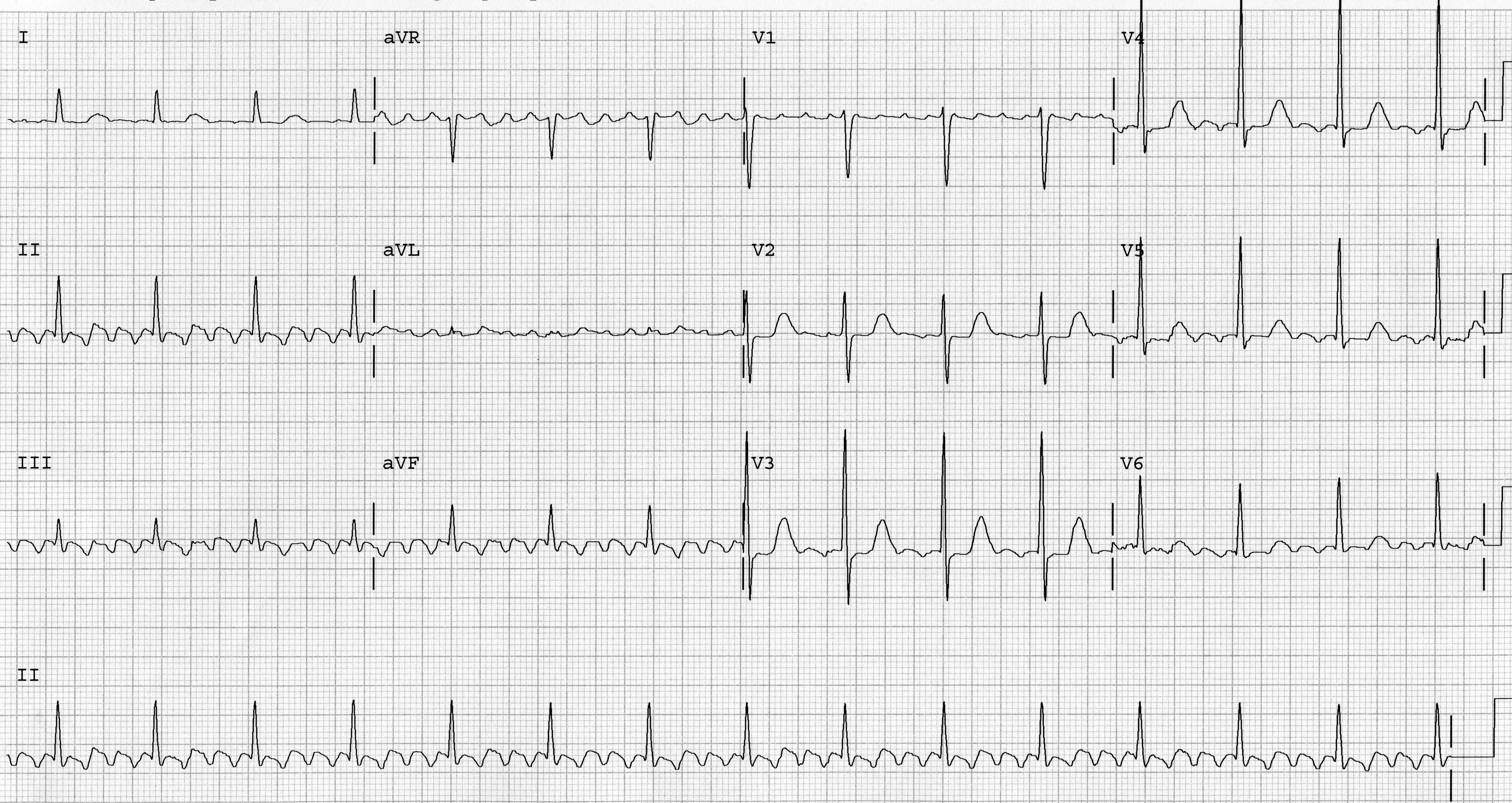 |
12-lead electrocardiogram of atrial flutter with 4:1 AV response and ventricular rate of 90 beats/min Image courtesy of J. Stephan Stapczynski, MD |
Occasionally, the flutter waves may not be discernible in the inferior leads. (See Figure 4C.) In cases of 2:1 AV block, the ventricular rate is close to 150 beats per minute and at times may be difficult to distinguish from sinus tachycardia. To make the distinction clear, vagal maneuvers can be used to transiently slow conduction through the AV node to discern the presence of flutter waves. (See Part II of this article for details.)
Figure 4C. Atrial Flutter with Minimal Flutter Waves |
 |
The flutter waves are difficult to see and this rhythm may be mistaken for sinus tachycardia at a rate of 150 beats/min Image courtesy of J. Stephan Stapczynski, MD |
Multifocal Atrial Tachycardia
Multifocal atrial tachycardia (MAT) is a rare tachydysrhythmia, seen in only 0.05% to 0.32% of ECGs in hospital admissions, and is characterized by multiple ectopic foci within the atria.41 This arrhythmia represents a poor prognostic sign in acute illness and is associated with chronic obstructive pulmonary disease, chronic heart failure, and chronic renal failure.41
The diagnosis is made by obtaining a 12-lead ECG, which shows an irregular tachycardia with at least three distinct, identifiable P wave morphologies.42 (See Figure 5.) In addition to this, there should be irregular PP intervals with the presence of an isoelectric baseline in between P waves, which differentiates this rhythm from atrial fibrillation.41,42 This tachydysrhythmia generally resolves with treatment of the underlying condition or removal of an offending agent.41,42
Figure 5. Multifocal Atrial Tachycardia |
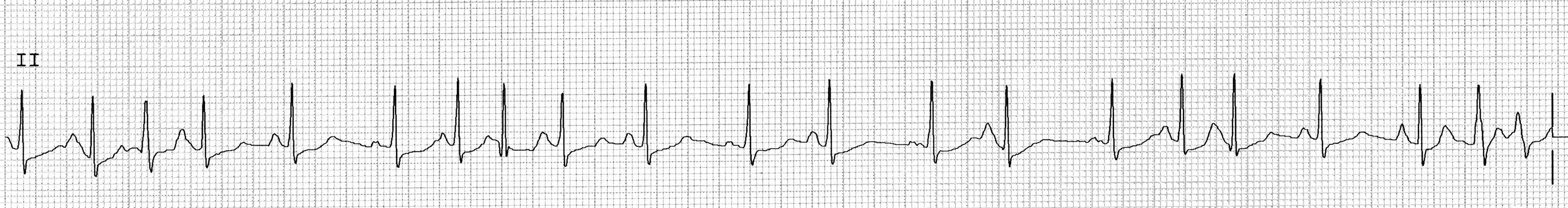 |
Image courtesy of J. Stephan Stapczynski, MD |
Paroxysmal Supraventricular Tachycardia
Paroxysmal supraventricular tachycardia (PSVT) refers to a group of tachydysrhythmias that originate in cardiac tissue above the bundle of His. For the purposes of this review, we will discuss the two most encountered PSVT rhythms in the ED: atrioventricular nodal re-entrant tachycardia (AVNRT) and atrioventricular reciprocating tachycardia (AVRT).43
Atrioventricular Nodal Re-Entrant Tachycardia
AVNRT is defined as a regular, narrow complex tachycardia with a ventricular rate between 160 and 220 beats per minute. (See Figure 6.) It is the most common cause of palpitations in patients with structurally normal hearts and often occurs without the presence of systemic illness. P waves are not visible before the narrow QRS complex, but on close inspection may be seen buried within the QRS complex or retrograde afterward. Treatment centers on disrupting the cycle of pathways that maintain the re-entry circuit within the AV node.44
Figure 6. Atrioventricular Nodal Re-Entrant Tachycardia (AVNRT) |
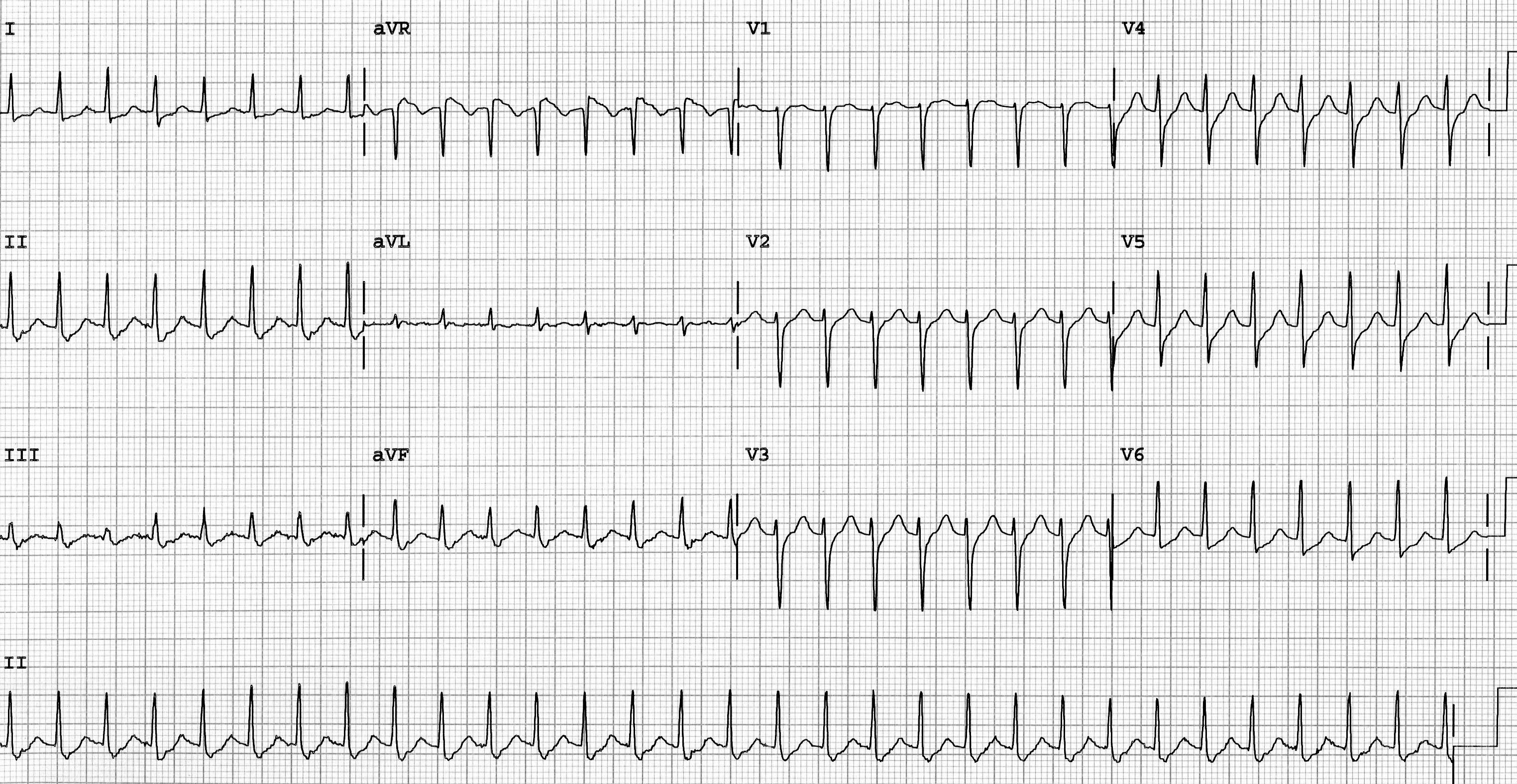 |
Image courtesy of J. Stephan Stapczynski, MD |
Atrioventricular Reciprocating Tachycardia
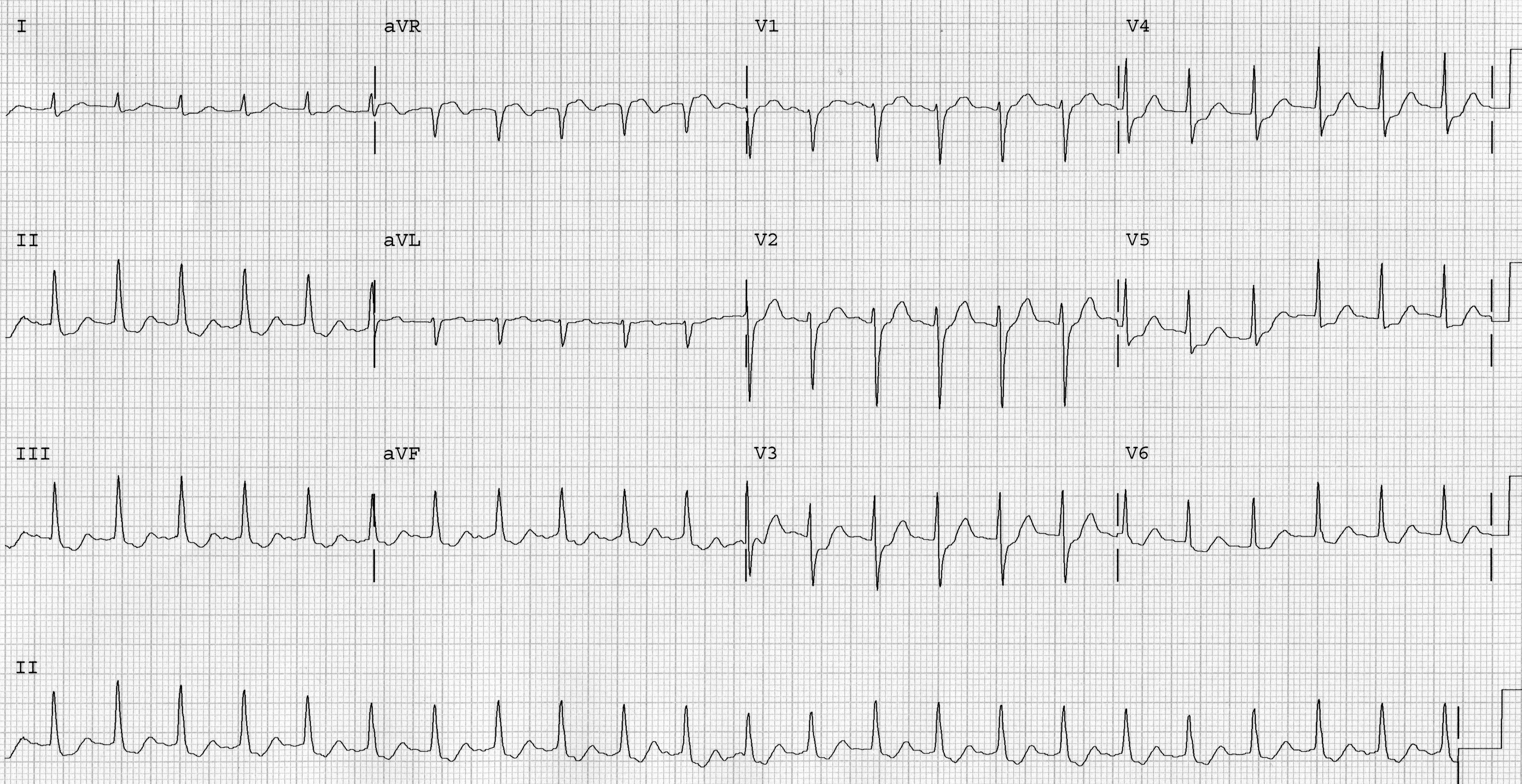
AVRT is a type of SVT that requires the presence of an accessory pathway separate from the AV node. This pathway has electrophysiologic properties different from the AV node that serve to initiate and maintain the arrhythmia.45 Depending on the direction of electrical conduction, AVRT may be orthodromic or antidromic.
Orthodromic AVRT comprises the majority of AVRTs and can be initiated by either atrial or ventricular premature beats.45 (See Figure 7.) The premature impulse is conducted down the His-Purkinje system in an antegrade fashion and retrograde up through the accessory pathway. In orthodromic AVRT, the ECG is notable for a ventricular rate between 150 and 250 beats per minute with the presence of a narrow QRS complex and retrograde P waves following the QRS complex. The duration of the RP interval will be less than half of the RR interval.
Figure 7. Orthodromic Atrioventricular Reciprocating Tachycardia (AVRT) Initiated by a Premature Atrial Contraction (PAC) |
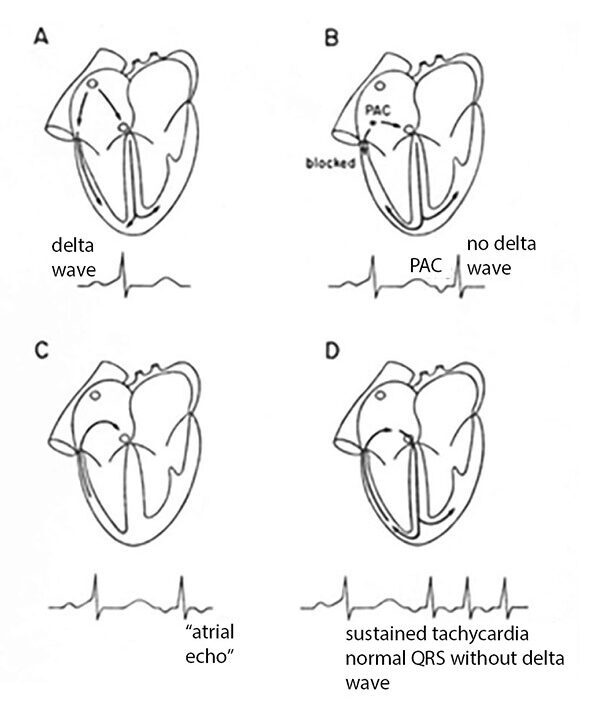 |
During sinus rhythm, pre-excitation of the ventricle creates the delta wave on the electrocardiogram. During AVRT, the ventricles are only activated via the His-Purkinje system and there is no delta wave. Image courtesy of J. Stephan Stapczynski, MD |
Antidromic AVRT represents around 5% to 10% of all AVRTs.45 In this arrhythmia, the impulse is conducted in an antegrade fashion down the accessory pathway and in a retrograde fashion through the His-Purkinje system. As a result, the ECG is notable for a wide QRS complex since the ventricles are activated solely by the accessory pathway. Retrograde P waves sometimes can be seen, and the overall ventricular rate is between 150 to 250 beats per minute. The RP interval also will be prolonged and generally is longer than half of the RR interval.
Ventricular Tachycardia
Ventricular tachycardia (VT) is indicative of serious myocardial disease and portends a high risk for clinical decompensation.46 The diagnosis of VT requires at least three ventricular contractions at a rate greater than 100 beats per minute. VT can be episodic, with recurrent runs of tachycardia that self-terminate. Sustained VT is with a duration of at least 30 seconds or there is hemodynamic instability.47 VT can originate from either the ventricular myocytes or from the His-Purkinje tissues.
The clinical challenge is to differentiate VT from SVT with ventricular conduction aberrancy. Several algorithms have been developed to differentiate VT from SVT with aberrancy, the details of which are beyond the scope of this article. Traditional teaching emphasizes five ECG features to differentiate VT from SVT with aberrancy: irregularity, AV dissociation, fusion and capture beats, QRS duration, and QRS complex concordance.
Ventricular tachycardia is usually very regular; marked irregularity is more suggestive of atrial fibrillation with ventricular aberrance. AV dissociation is strongly suggestive of VT but is noted in only about 10% of such cases. Capture and fusion beats suggest ventricular tachycardia.
VT usually has wider QRS complexes than SVT with aberrancy, so an extreme QRS duration > 160 msec favors VT. Negative concordance, where all QRS complexes across the precordial leads have a negative or downward deflection, suggests ventricular tachycardia. Additionally, the presence of an extreme axis and delay in the initial phase of the QRS complex can be used to diagnose VT; however, these diagnostic criteria can be difficult to discern.48
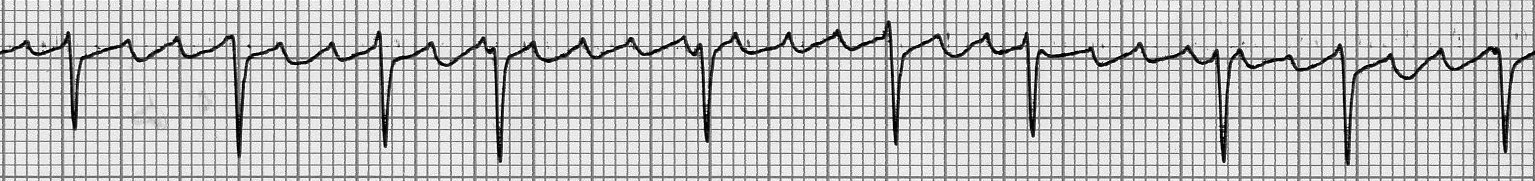
VT can be categorized further into two subtypes: monomorphic and polymorphic. Monomorphic VT has a single consistent QRS morphology (see Figure 8), while polymorphic VT can have multiple QRS morphologies.48 (See Figure 9.)
Figure 8. Ventricular Tachycardia |
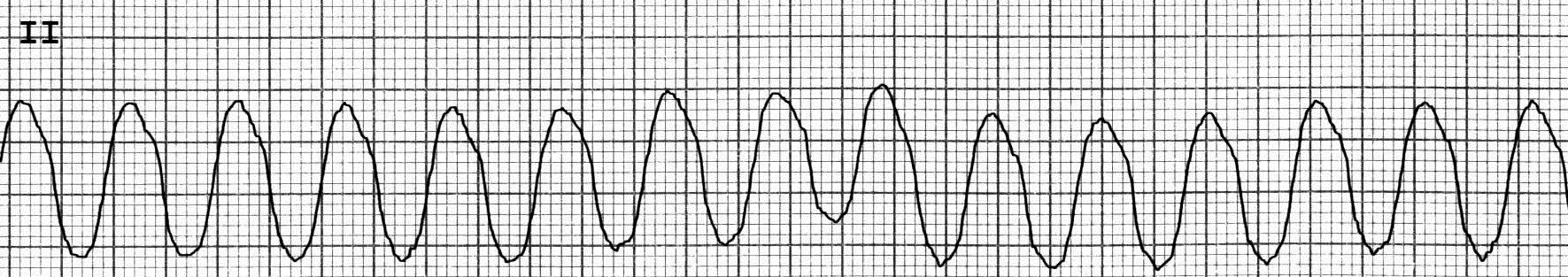 |
Lead II, monomorphic ventricular tachycardia at a rate of 142 beats/min Image courtesy of J. Stephan Stapczynski, MD |
Figure 9. Torsades de Pointes |
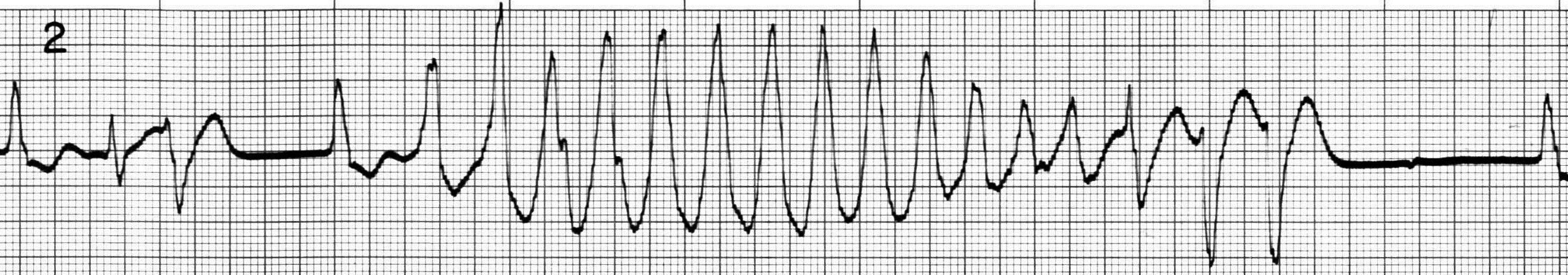 |
Lead II, 16-beat run of torsades with sinusoidal variation in QRS amplitude and direction triggered by PVC Image courtesy of J. Stephan Stapczynski, MD |
The differential diagnosis of polymorphic VT includes two potential mimics: an atrial tachyarrhythmia with ventricular preexcitation and an ECG artifact caused by patient movement or electrical interference. There are several forms of polymorphic VT, but a specific form termed torsades de pointes is worthy of discussion.
Torsades de pointes is an arrhythmia caused by genetic or acquired long QT syndrome. Malfunction of ion channels in the myocardial cell membrane delays repolarization and postpones inactivation of the calcium channel. The excessive inflow of calcium then creates early after-depolarizations that may trigger reentrant arrhythmias. The torsades rhythm is characterized by progressive changes in morphology, polarity, and amplitude of the QRS complex appearing to twist around the isoelectric baseline. Torsades can be episodic, with self-termination, but is prone to recurrence. Sustained torsades can deteriorate into ventricular fibrillation.
VT usually is due to ischemic heart disease, cardiomyopathies, and electrolyte derangements such as hypokalemia and hypomagnesemia. In younger individuals presenting with VT, it is important to inquire about family and personal history to assess for the role of substance use and the presence of channelopathies. Brugada syndrome, long or short QT syndrome, and malignant early repolarization all are indicative of inherited channelopathies and should be considered in the patient’s evaluation.
VT is designated as idiopathic when a cause is unable to be identified and is a diagnosis of exclusion, since full assessment of the patient requires a detailed evaluation outside of the scope of the emergency clinician.
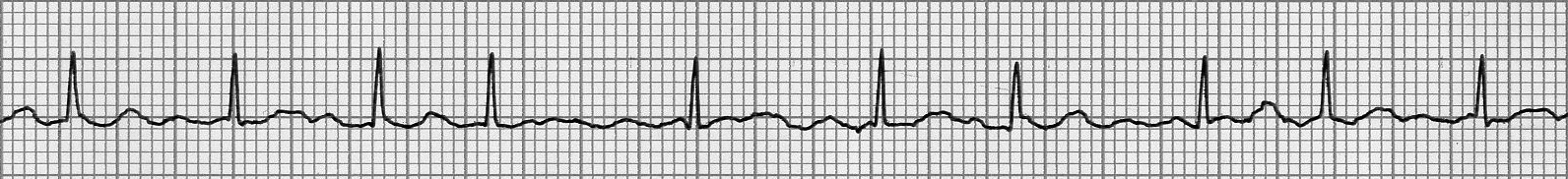
Ventricular Fibrillation
Ventricular fibrillation is a fatal tachydysrhythmia due to uncoordinated chaotic electrical activity within the ventricles that results in cardiac arrest. Ventricular fibrillation can have many causes but most commonly is associated with myocardial infarction, electrolyte abnormalities, and cardiomyopathy.
Ventricular fibrillation is diagnosed on cardiac monitoring by the presence of fibrillation waves with varying amplitude with no identifiable P waves, QRS complexes, or T waves, with a rate of 150 to 500 beats per minute.49 (See Figure 10.)
Figure 10. Ventricular Fibrillation |
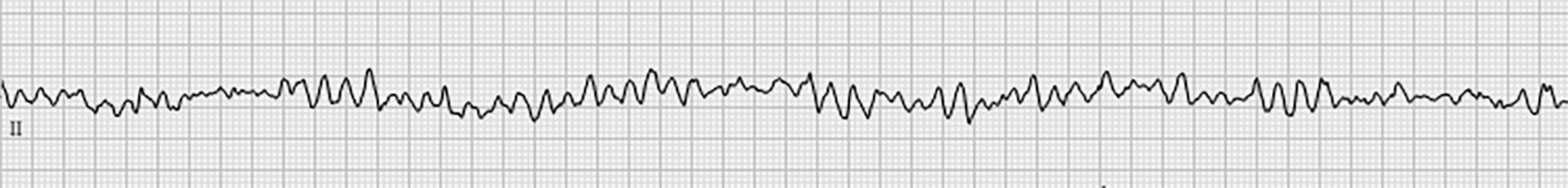 |
Image courtesy of J. Stephan Stapczynski, MD |
Ventricular fibrillation can be a primary event where an electrical discharge during ventricular repolarization can trigger chaotic reentry, producing ventricular fibrillation. Commotio cordis is an example of this where blunt impact to the mid or low chest wall triggers ventricular fibrillation.
Ventricular fibrillation also can result from deterioration of sustained VT. This process usually occurs in patients with coronary artery disease or cardiomyopathies. Sustained VT usually has diminished cardiac output that, over time, reduces coronary artery perfusion leading to increasing myocardial ischemia. The ischemic myocardium no longer can maintain organized depolarization and deteriorates into the electrical and mechanical chaos of ventricular fibrillation.
REFERENCES
- Song Y, Chen J, Zhang R. Heart rate estimation from incomplete electrocardiography signals. Sensors (Basel) 2023;23:59.
- Hasegawa D, Sato R, Prasitlumkum N, et al. Effect of ultrashort-acting β-blockers on mortality in patients with sepsis with persistent tachycardia despite initial resuscitation: A systematic review and meta-analysis of randomized controlled trials. Chest 2021;159:2289-2300.
- Krieger P, Zhao A, Croll L, et al. Tachycardia is associated with mortality and functional outcome after thrombectomy for acute ischemic stroke. J Stroke Cerebrovasc Dis 2022;31:106450.
- Hemu M, Chiang CJ, Bhatt PK, et al. Associations between sinus tachycardia and adverse cardiovascular outcomes and mortality in cancer patients. J Thorac Dis 2021;13:4845-4852.
- Linton JJ, Eagles C, Green MS, et al. Diagnosis and management of patients who present with narrow complex tachycardia in the emergency department. Can J Emerg Med 2023;25:303-313.
- Tverdal A, Hjellvik V, Selmer R. Heart rate and mortality from cardiovascular causes: A 12 year follow-up study of 379 843 men and women aged 40-45 years. Eur Heart J 2008;29:2772-2781.
- Palatini P, Julius S. Association of tachycardia with morbidity and mortality: Pathophysiological considerations. J Hum Hypertens 1997;11 Suppl 1:S19-S27.
- Dark T, Flynn HA, Rust G, et al. Epidemiology of emergency department visits for anxiety in the United States: 2009-2011. Psychiatr Serv 2017;68:238-244.
- Guerri G, Bressan S, Sartori M, et al. Hypothyroidism and hyperthyroidism. Acta Biomed 2019;90(Suppl 10):83-86.
- Hsueh B, Chen R, Jo Y, et al. Cardiogenic control of affective behavioural state. Nature 2023;615:292-299.
- Dayoub EJ, Jena AB. Does pain lead to tachycardia? Revisiting the association between self-reported pain and heart rate in a national sample of urgent emergency department visits. Mayo Clin Proc 2015;90:1165-1166.
- Bossart P, Fosnocht D, Swanson E. Changes in heart rate do not correlate with changes in pain intensity in emergency department patients. J Emerg Med 2007;32:19-22.
- Marco CA, Plewa MC, Buderer N, et al. Self-reported pain scores in the emergency department: Lack of association with vital signs. Acad Emerg Med 2006;13:974-979.
- Carvalho AF, Heilig M, Perez A, et al. Alcohol use disorders. Lancet 2019;394:781-792.
- Tisdale JE, Chung MK, Campbell KB, et al. Drug-induced arrhythmias: A scientific statement from the American Heart Association. Circulation 2020;142:e214-e233.
- Airagnes G, Ducoutumany G, Laffy-Beaufils B, et al. Alcohol withdrawal syndrome management: Is there anything new? Rev Méd Interne 2019;40:373-379.
- Moheimani RS, Bhetraratana M, Yin F, et al. Increased cardiac sympathetic activity and oxidative stress in habitual electronic cigarette users: Implications for cardiovascular risk. JAMA Cardiology 2017;2:278-284.
- Vo AT, Patton T, Peacock A, et al. Illicit substance use and the COVID-19 pandemic in the United States: A scoping review and characterization of research evidence in unprecedented times. Int J Environ Res Public Health 2022;19:8883.
- Imazio M, Gaita F, LeWinter M. Evaluation and treatment of pericarditis: A systematic review [published correction appears in JAMA 2015;314:1978] [published correction appears in JAMA 2016;315:90. Dosage error in article text]. JAMA 2015;314:1498-1506.
- Buttà C, Zappia L, Laterra G, Roberto M. Diagnostic and prognostic role of electrocardiogram in acute myocarditis: A comprehensive review. Ann Noninvasive Electrocardiol 2020;25:e12726.
- Gottlieb M, Long B, Koyfman A. Evaluation and management of aortic stenosis for the emergency clinician: An evidence-based review of the literature. J Emerg Med 2018;55:34-41.
- Di Labbio G, Ben Assa E, Kadem L. Experimental investigation of the effect of heart rate on flow in the left ventricle in health and disease—Aortic valve regurgitation. J Biomech Eng 2020;142:051005.
- Akinseye OA, Pathak A, Ibebuogu UN. Aortic valve regurgitation: A comprehensive review. Curr Probl Cardiol 2018;43:315-334.
- Wunderlich NC, Dalvi B, Ho SY, et al. Rheumatic mitral valve stenosis: Diagnosis and treatment options. Curr Cardiol Rep 2019;21:14.
- Westermann D, Schrage B. Mitral stenosis and atrial fibrillation. Heart 2020;106:713-713.
- Douedi S, Douedi H. Mitral regurgitation. In: StatPearls. StatPearls Publishing; 2023. Accessed June 11, 2023.
- Kubala M, Essayagh B, Michelena HI, et al. Arrhythmic mitral valve prolapse in 2023: Evidence-based update. Front Cardiovasc Med 2023;10.
- Chen J, Aronowitz P. Congestive heart failure. Med Clin North Am 2022;106:447-458.
- Gutierrez A, Ash J, Akdemir B, et al. Nonsustained ventricular tachycardia in heart failure with preserved ejection fraction. Pacing Clin Electrophysiol 2020;43:1126-1131.
- Skinner JR, Winbo A, Abrams D, et al. Channelopathies that lead to sudden cardiac death: Clinical and genetic aspects. Heart Lung Circ 2019;28:22-30.
- Campuzano O, Allegue C, Partemi S, et al. Negative autopsy and sudden cardiac death. Int J Legal Med 2014;128:599-606.
- McKenna WJ, Maron BJ, Thiene G. Classification, epidemiology, and global burden of cardiomyopathies. Circ Res 2017;121:722-730.
- Henning A, Krawiec C. Sinus tachycardia. In: StatPearls. StatPearls Publishing; 2023.
- Sebastian SA, Co EL, Panthangi V, et al. Postural orthostatic tachycardia syndrome (POTS): An update for clinical practice. Curr Probl Cardiol 2022;47:101384.
- Ali M, Haji AQ, Kichloo A, et al. Inappropriate sinus tachycardia: A review. RCM 2021;22:1331-1339.
- Sagris M, Vardas EP, Theofilis P, et al. Atrial fibrillation: Pathogenesis, predisposing factors, and genetics. Int J Molecular Sci 2022;23:6.
- Long B, Keim SM, Gottlieb M, Stiell IG. What is the best agent for rate control of atrial fibrillation with rapid ventricular response? J Emerg Med 2022;63:467-476.
- Brundel BJJM, Ai X, Hills MT, et al. Atrial fibrillation. Nat Rev Dis Primers 2022;8:21.
- Rodriguez Ziccardi M, Goyal A, Maani CV. Atrial flutter. In: StatPearls. StatPearls Publishing; 2023.
- Bagliani G, Leonelli FM, De Ponti R, et al. Electrocardiographic approach to atrial flutter: Classifications and differential diagnosis. Card Electrophysiol Clin 2022;14:385-399.
- Custer AM, Yelamanchili VS, Lappin SL. Multifocal atrial tachycardia. In: StatPearls. StatPearls Publishing; 2023.
- Harvey M. Challenges in diagnosing and managing multifocal atrial tachycardia. HeartRhythm Case Rep 2023;9:129-130.
- Ahmad F, Abu Sneineh M, Patel RS, et al. In the line of treatment: A systematic review of paroxysmal supraventricular tachycardia. Cureus 2021;13:e15502.
- Brubaker S, Long B, Koyfman A. Alternative treatment options for atrioventricular-nodal-reentry tachycardia: An emergency medicine review. J Emerg Med 2018;54:198-206.
- Jabbour F, Grossman SA. Atrioventricular reciprocating tachycardia. In: StatPearls. StatPearls Publishing; 2023.
- AlMahameed ST, Ziv O. Ventricular arrhythmias. Med Clin North Am 2019;103:881-895.
- Ding WY, Mahida S. Wide complex tachycardia: Differentiating ventricular tachycardia from supraventricular tachycardia. Heart 2021;107:1995-2003.
- Foth C, Gangwani MK, Ahmed I, Alvey H. Ventricular tachycardia. In: StatPearls. StatPearls Publishing; 2023.
- Ludhwani D, Goyal A, Jagtap M. Ventricular fibrillation. In: StatPearls. StatPearls Publishing; 2023.
This issue is the first of a two-part discussion of tachycardia, the most common rhythm abnormality seen in the emergency department. Part I will discuss the epidemiology, etiology, and characteristics of the different tachycardic arrhythmias. Part II will discuss conditions affecting other organ systems that can produce tachycardia, then finish by reviewing the assessment and management of these patients. We hope these two issues will be useful to your clinical practice.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
