AUTHORS
Pradeep Padmanabhan, MD, MSc, Associate Professor of Pediatrics, Wright State University; Associate Program Director, Pediatric Emergency Medicine Fellowship, Dayton Children’s Hospital, Dayton, OH
Jonathan Elliott, MD, Fellow, Pediatric Emergency Medicine, Dayton Children’s Hospital, Dayton, OH
PEER REVIEWER
Catherine A. Marco, MD, FACEP, Professor, Department of Emergency Medicine, Penn State Health, Hershey Medical Center, Hershey, PA
EXECUTIVE SUMMARY
- Children younger than 3 years of age rarely get streptococcal pharyngitis.
- Both the Centor and McIsaac clinical decision tools have low positive predictive value, even for those with a high score.
- Real-time polymerase chain reaction (PCR) is almost 100% sensitive and 100% specific for streptococcal pharyngitis.
- When the diagnosis of peritonsillar abscess is obvious, a contrasted computed tomography scan typically does not add additional information and preferably could be avoided.
- Erysipelas has intense erythema with distinct borders that are raised from the surrounding skin, which is different than simple cellulitis.
- Streptococcal and staphylococcal toxic shock are clinically indistinguishable and should be treated with a beta-lactamase resistant antimicrobial.
- Clindamycin is used in addition for the treatment of toxic shock syndrome to inhibit the production of cytokines and toxins.
- Streptococcal pneumonia dramatically increased during the COVID-19 pandemic.
- The incidence of both noninvasive and invasive group A streptococcal infections has increased after the COVID-19 pandemic.
- Group A streptococcal necrotizing fasciitis is not gas-forming, so free air is not to be detected in imaging studies.
Epidemiology
Group A Streptococcus (GAS) infections range from the common pharyngitis and skin infections to the invasive disease with complications and post-infectious sequelae. Streptococcal infections are common among older children, particularly between 5 and 15 years of age. In the United States, there is both a seasonality and geographic pattern of pharyngeal streptococcal infections, with infections occurring more frequently during winter and spring in the northern part of the country.1 While infectious pharyngitis is mostly viral in nature, GAS is the primary source of bacterial pharyngitis infecting 800 million people annually, resulting in an estimated 639,000 deaths globally per year.2 Infections and deaths disproportionately affect populations with lower incomes and limited resources.3
Acute infections caused by Streptococcus pyogenes may present in the form of pharyngitis, scarlet fever, impetigo, cellulitis, or erysipelas. Importantly, streptococcal infections can be invasive, resulting in necrotizing fasciitis, myositis, and streptococcal toxic shock syndrome. Immune-mediated complications include acute rheumatic fever and acute glomerulonephritis. Streptococcus agalactiae may cause meningitis, neonatal sepsis, and pneumonia in neonates. While most physicians are familiar with the common presentations of streptococcal infections (e.g., pharyngitis, impetigo), it is important to recognize the carrier state, learn management of common complications (e.g., peritonsillar abscess), and identify the potentially serious, and perhaps deadly, complications and invasive infections.
Etiology
Scarlet fever and invasive streptococcal infections are caused by GAS, which also is referred to as Streptococcus pyogenes. This strain of bacteria is characterized as a gram-positive coccus, which grows in chains. The strain of M protein within the bacteria generally correlates with the type of infection and post-infectious sequelae. In general, strains that cause pharyngitis are more associated with acute rheumatic fever, while those that cause skin infections are implicated with glomerulonephritis.1 In addition to GAS, there are many other groups of beta-hemolytic streptococci. A few of these will be discussed briefly.
Pathophysiology
There are more than 220 different subtypes of GAS, which are classified based on a surface protein known as the M protein. This protein triggers immune-modulatory effects by binding to various cell components. The M protein also contributes to the ability for Streptococcus to colonize a host. The vast degree of variation in this protein is responsible in part for the geographic patterns of infection, as well as the varying degrees of invasiveness that are seen.4
GAS can produce exotoxins and enzymes that are responsible for some of the unique conditions associated with Streptococcus infections. There still is much to be learned about these exotoxins, since many seemingly induce an antibody response but do not seem to produce or convey immunity. Assessment of these antibodies (antistreptolysin O [ASO], DNase B) may be useful in helping to establish a recent Streptococcus infection when there is concern for a post-infectious complication.1
The primary mode of transmission for group A streptococci is through respiratory droplets. In streptococcal impetigo, the organism is directly transmitted from the skin. The patients with impetigo are colonized by GAS prior to infection. Close contact is required for transmission. Crowded places, such as daycares and schools, are common locations for outbreaks to occur.5 Given their lack of acquired immunity, along with the amount of time spent in crowded settings, children are particularly at risk for streptococcal infections.5
Clinical Features of Streptococcal Pharyngitis
The classic features of GAS pharyngitis include inflammation of the tonsils, sore throat, palatal petechiae, tender anterior cervical lymphadenopathy, and strawberry tongue. See Figure 1 for a depiction of pharyngeal erythema, edema, and palatal petechiae, and Figure 2 for strawberry tongue.
Figure 1. Streptococcal Pharyngitis |
 |
Patient exhibiting redness and edema of the oropharynx, and petechiae on the soft palate Source: Centers for Disease Control and Prevention/Heinz F. Eichenwald, MD |
Figure 2. Strawberry Tongue |
 |
Image used with permission from Dr. Janani Sankar, Kanchi Kamakoti CHILDS Trust Hospital, Chennai, India. |
Scarlet fever is characterized by a “sandpaper” type rash, also known as a scarlatiniform rash: fine erythematous papules that blanch. The onset of the rash is classically 24-28 hours after the onset of pharyngitis. It typically is more pronounced in the groin, antecubital fossae, and axillae. The skin then will begin to desquamate approximately three to four days after the appearance of the rash.1 Figure 3 shows the typical “sandpaper” appearance of a scarlatiniform rash, pronounced in the antecubital fossa.
Figure 3. Scarlatiniform Rash |
 |
Source: Centers for Disease Control and Prevention/Dr. Sellers |
Historically, scarlet fever was thought to be caused primarily through the release of toxins. However, newer information suggests that a delayed-type hypersensitivity reaction to superantigens plays a role. This is supported by the fact that individuals who have not had a prior streptococcal infection do not seem to develop scarlet fever.6
Children younger than 3 years of age rarely get Streptococcus infections and do not seem to develop acute rheumatic fever. Instead they develop fever, rhinitis, and irritability, described as streptococcosis.7
Diagnostic Studies
Among the clinical prediction rules for streptococcal pharyngitis, the Centor score and the McIsaac score are commonly used. The Centor score (see Table 1) incorporates the following four findings, which are the primary features of streptococcal pharyngitis: tonsillar exudates, tender anterior cervical adenopathy, absence of cough, and history of fever. However, even with all four criteria present (Centor score of 4), the prediction tool only identifies a 55% probability of GAS pharyngitis.8
Table 1. The Centor Score |
|||
Symptoms |
Points |
Score |
Post-Test Probability |
Tonsillar exudates |
1 |
0 |
2.5% |
Tender anterior cervical adenopathy |
1 |
1 |
6.5% |
Absence of cough |
1 |
2 |
15.4% |
History of fever (> 38.0°C) |
1 |
3 |
31.6% |
4 |
55.7% |
||
Source: Aalbers J, O’Brien KK, Chan WS, et al. Predicting streptococcal pharyngitis in adults in primary care: A systematic review of the diagnostic accuracy of symptoms and signs and validation of the Centor score. BMC Med 2011;9:67. https://creativecommons.org/licenses/by/2.0/ |
|||
The McIsaac score is a modified form of the Centor score, which also includes a point if the patient is between the ages of 3 and 14 years. A point is taken away if the patient is older than age 45 years. Both tests have been shown to be weak, with a low positive predictive value even for those with a high score.9 Lack of a cough and the presence of tonsillar exudates both are independently associated with GAS pharyngitis. However, these features also may be present with viral pharyngitis and, consequently, should not be relied on alone.10
For GAS pharyngitis, clinical features are insufficient to reliably distinguish from viral pharyngitis. Hence, laboratory testing is required for diagnosis. Throat culture is one such method for detection. However, given the time required for culture results, other, faster methods often are used. A rapid antigen detection test (RADT) allows for results within a matter of minutes. With this test, the patient sample is exposed to antibodies that bind to a GAS antigen and produce a visible result. While these tests have a high specificity, there is a lower sensitivity compared to culture. Thus, culture should be performed when there is a negative rapid antigen test result and diagnostic confirmation is desired.1
Antibiotics often are inappropriately prescribed for pharyngitis, as indicated by studies that show the rate of antibiotic prescription is higher than the rate of streptococcal pharyngitis.11 Avoiding unnecessary prescription of antibiotics is vital to preventing the development of antibiotic resistance. More recently, real-time polymerase chain reaction (PCR) has been employed to overcome some of the negative aspects of previously mentioned tests, allowing for more accurate diagnosis and improved antibiotic prescribing techniques.
With advances in technology, real-time PCR is now inexpensive and fast, with both high sensitivity and high specificity. RADT swabs have an estimated sensitivity of 86% and specificity of 96%. This is compared to an estimated 100% sensitivity and 100% specificity of a real-time PCR test. RADT takes two to nine minutes to result, while real-time PCR takes an estimated 22-26 minutes.11
For establishing the presence of a recent GAS infection, ASO and anti-DNAse B are the two serum tests that primarily are used. There are newer tests in development, including a slide agglutination test and a latex agglutination test. However, the results and interpretation of these tests do not yet have standards that are well established.1
Household contacts need not be swabbed for strep throat unless they are at high risk of complications. Due to the low incidence of GAS infection, children younger than 3 years of age should not be tested.
Treatment of Streptococcal Pharyngitis
Antibiotics are primarily given for GAS pharyngitis to reduce the symptoms, prevent both the suppurative and nonsuppurative complications, and prevent spread to contacts. However, antibiotics have not been proven to prevent acute glomerulonephritis.6
When a patient is prescribed an antibiotic for treatment of streptococcal pharyngitis, a clinical response is usually achieved within 24-48 hours of therapy.13 More importantly, the antibiotic therapy reduces duration of illness and toxicity as well as infectivity. Penicillin is the drug of choice, and there has been no proven case of resistance. Broader spectrum antibiotics have not been shown to be more effective. Therefore, penicillin is recommended to promote antibiotic stewardship.12 Treatment options include oral penicillin or amoxicillin for 10 days, or a one-time dose of intramuscular benzathine penicillin. It is important to note that benzathine penicillin injections are painful, which can be lessened somewhat when given with the medicine at room temperature.
For those with a penicillin allergy, cephalexin or clindamycin may be considered. It should be noted that resistance to azithromycin exists with some strains of GAS.13 Cephalosporins generally are the preferred second-line agents. Resistance patterns vary regionally, and treatment recommendations differ by country. Consequently, treatment of streptococcal pharyngitis must be tailored to the specific patient population.14
Invasive Streptococcal Infections
Epidemiology
Invasive streptococcal infections have a wide variety of presentations, including bacteremia, cellulitis, necrotizing fasciitis, myositis, meningitis, and toxic shock syndrome. The pattern of these invasive infections has changed over recent years, decreasing during the initial years of the COVID-19 pandemic and subsequently increasing in incidence.15 In particular, abscesses, mastoiditis, and sinus vein thrombosis increased in incidence dramatically in the winter of 2022-2023, the first post-pandemic year.16 It is important that healthcare providers are aware of these rare but potentially deadly presentations.
Clinical Features
Invasive streptococcal infection is present when a normally sterile site (blood, brain, etc.) is infected by Streptococcus. While cellulitis and bacteremia are the most common, infections can include pneumonia/empyema, erysipelas, necrotizing fasciitis, and central nervous system (CNS) infections. Septic shock or toxic shock syndrome subsequently may develop.15 Given the wide variety of types of infections, the presenting features also will vary based on the specific infection. The clinical features, diagnosis, and management of each condition will be discussed.
Erysipelas
Erysipelas is an infection of the skin that is limited to just the dermis. It is characterized by an area of intense erythema that is raised from the surrounding skin. The infection has distinct borders. It typically spreads rapidly, and systemic symptoms such as fever or chills are common.17 Figure 4 shows the typical appearance of erysipelas. Note the intense edema of the skin. This contrasts with the typical flat nature of simple cellulitis. Diagnosis of erysipelas is clinical, and the preferred treatment is a penicillin. Clindamycin may be considered, but there is a higher rate of resistance compared to penicillins.17
Figure 4. Erysipelas |
 |
Source: Centers for Disease Control and Prevention/ Dr. Thomas F. Sellers, Emory University |
Cellulitis
Streptococcal cellulitis classically develops as a secondary infection from trauma, burns, or a surgical site. A painful area of erythema, swelling, and warmth is typical. The lesion typically is flat. The demarcation may be less distinct than with erysipelas. Like erysipelas, progression may be rapid, and systemic symptoms are common. The diagnosis is made clinically. Given that GAS cellulitis is indistinguishable from cellulitis caused by other etiologies, antibiotics should include staphylococcal coverage. A first-generation cephalosporin, such as cephalexin, is the recommended first-line treatment.17
Guttate Psoriasis
A skin manifestation associated with a recent streptococcal infection (both pharyngitis and skin infections) is guttate psoriasis. (See Figure 5.) The onset is acute, usually one to two weeks after GAS, and is characterized by raindrop-like, scaly, small lesions throughout the body.18 Koebner phenomenon — the development of new lesions over areas of trauma similar to underlying lesions — is characteristic of psoriasis. Guttate psoriasis is self-limited and clears in approximately three to four months. Emollients and ultraviolet (UV) phototherapy may help.
Figure 5. Guttate Psoriasis |
 |
Source: Bobjgalindo. https://commons.wikimedia.org/wiki/File:Guttate_psoriasis.jpg |
Streptococcal Toxic Shock Syndrome
Toxic shock syndrome commonly can result from staphylococcal or streptococcal infections. While vaginal colonization and tampon use has been heavily linked, abortion, vaginal delivery, and surgical procedures also have been implicated in the development of staphylococcal toxic shock syndrome.
GAS toxic shock syndrome (STSS) may occur due to the spread of an invasive toxin-producing GAS into a sterile area, such as blood, meninges, or pleura, from a deep-seated and/or necrotic skin infection. The toxins help stimulate the production of tumor necrosis factor (TNF), are associated with capillary leak, and result in hypotension and multiorgan damage.
GAS toxic shock syndrome is characterized by rapid progression to multiorgan involvement and shock. Hypotension plus at least two of the following characteristics are required for diagnosis: respiratory distress syndrome, renal injury, hepatic injury, coagulopathy, erythematous macular desquamating rash, or soft tissue necrosis along with isolation of the organism.19 The typical macular rash is shown in Figure 6. Note the associated edema of the skin. Progression typically is quite rapid, leading to significant mortality.
Figure 6. Erythematous Macular Rash of Toxic Shock Syndrome |
 |
Source: Centers for Disease Control and Prevention. https://phil.cdc.gov/Details.a... |
More than 50% of patients with STSS have blood cultures positive for group A streptococci. Early recognition and prompt treatment with fluid resuscitation and antibiotics is vital to improving survival.19 Since both Staphylococcus aureus and Streptococcus pyogenes can cause toxic shock and are clinically indistinguishable, treatment regimens should include both a beta-lactamase antimicrobial that is bactericidal, as well as clindamycin to prevent the production of cytokines and toxins.20
If the patient is significantly ill, has a necrotizing infection, or has organ failure, intravenous immunoglobulin (IVIG) may be helpful by neutralizing toxin-producing superantigen and affecting cytokine synthesis.21 STSS has a worse prognosis than Staphylococcus-induced toxic shock syndrome, primarily with the difficulty in accessing and clearing pus from deep-seated infections. Drainage and debridement of any deep lesions and abscesses when possible is important to achieve source control of the infection.22
Once the surgical procedures are done and the patient is hemodynamically stable and shows signs of improvement, and the cultures are negative for Staphylococcus, it is reasonable to discontinue clindamycin alone after 48-72 hours. However, the patient should continue the primary antibiotic coverage (penicillin) for at least 14 days.
Pneumonia
Pneumonia caused by GAS previously was very rare, accounting for less than 1% of all cases of community-acquired pneumonia. However, more recent data following the COVID-19 pandemic have identified pneumonia in more than half of those who are critically ill with invasive streptococcal infections. Consequently, healthcare providers must maintain a high index of suspicion for this important cause of pneumonia, especially if there have been recent viral respiratory infections. Multilobar pneumonia is common, and progression to empyema also occurs frequently. Treatment, as with community-acquired pneumonia in general, is a penicillin such as ampicillin.22
Peritonsillar Abscess
Peritonsillar abscess is a common complication from streptococcal pharyngitis. Rarely, peritonsillar abscesses can be bilateral, but most frequently they are unilateral.23 A peritonsillar abscess often is the result of extension of tonsillitis. Other etiologies include oral/dental infections, trauma, surgery, or obstruction of salivary glands.24
While Streptococcus pyogenes is the most frequently identified bacteria in peritonsillar abscesses, infections typically are polymicrobial, with other species including Fusobacterium necrophorum and Fusobacterium nucleatum also being identified frequently, along with gram-negative anaerobic rods.25
The diagnosis is made based on clinical features, but it may be supported with imaging.23 Physical exam findings alone have a 75% sensitivity for peritonsillar abscess.26 Physical exam findings include a muffled voice, palatal edema and uvular deviation, and trismus (pain with opening the mouth).23
While the diagnosis primarily is clinical, a computed tomography (CT) scan of the neck with contrast may be used to determine the size of an abscess.23 Figure 7 shows CT scan findings of a peritonsillar abscess. Ultrasound is an alternative mode of imaging that does not involve any ionizing radiation.26 Imaging is not necessary, since studies have shown no difference in outcomes for patients treated with antibiotics compared to those who received aspiration or drainage of the abscess.27 However, CT scan may be considered if the diagnosis is not clear or the patient is not responding to medical management.26 Conversely, when there is a high suspicion of a peritonsillar abscess on physical exam, a CT scan does not typically add any additional information, and preferably could be avoided.26
Figure 7. Computed Tomography Scan of Peritonsillar Abscess |
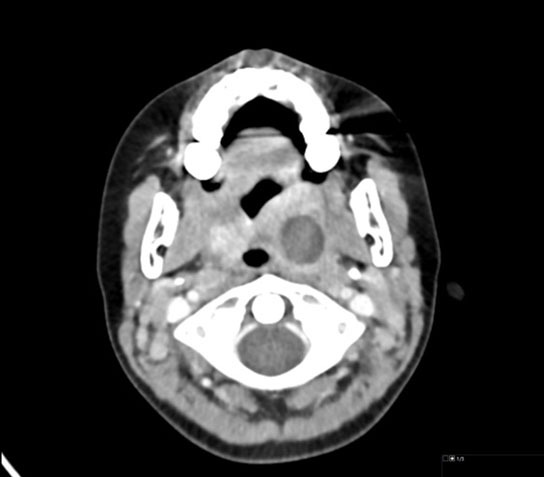 |
Axial contrast-enhanced computed tomography scan shows a 2 cm low-attenuation collection at the left tonsillar fossa, compatible with abscess (note the large but otherwise normally enhancing right palatine tonsil for comparison). Image used with permission from Mark Warren, DO, Dayton Children’s Hospital. |
An abscess that is larger than 2 cm may benefit from drainage; those of smaller size often are successfully managed with antibiotics alone.21 When ultrasound guidance is used, there is a higher rate of successful needle drainage.26
Given the polymicrobial nature of the abscess, amoxicillin-clavulanic acid is the treatment of choice. Clindamycin with ceftriaxone also may be considered, but there is a high frequency of anaerobic bacterial resistance to clindamycin. Steroids also may be used to help alleviate pain.23
The COVID-19 pandemic has somewhat altered the etiology of peritonsillar abscesses. While the incidence of peritonsillar abscess does not seem to have changed with the pandemic, there have been slight differences in the bacteria, with an increase in Fusobacterium species. Interestingly, an increase in surgical management of abscesses during COVID-19 restrictions led to longer hospital stays.27
Additional Aspects
As mentioned previously, there has been an increase in both noninvasive and invasive streptococcal infections in the post-COVID-19 pandemic era. It previously has been shown that infection with influenza virus increases the susceptibility to invasive streptococcal infections. In animal models, non-pulmonary invasive streptococcal infections are more common if there was a recent influenza infection.28 Interestingly, the increased incidence of streptococcal infections rose along with the growth in respiratory syncytial virus and influenza infections, and GAS infections continued to be detected for some time after viral respiratory infections decreased, suggesting other factors are responsible for this increase.29
Streptococcal Carrier State
It is important to discuss the carrier state and identify situations where testing is unnecessary and antibiotics unwarranted. When testing is being performed for streptococcal pharyngitis, some consideration must be given to whether the individual being tested is acutely infected with Streptococcus or simply a chronic carrier of GAS. As much as one-fourth of children with a sore throat are colonized with GAS rather than acutely infected.
Carriers of GAS will test positive for Streptococcus pyogenes, even in the absence of acute infection. Those colonized are at very low risk of developing post-infectious sequelae or complications. As discussed previously, the physical exam findings for streptococcal pharyngitis are nonspecific and cannot be relied upon alone to differentiate a true infection from a carrier state. Children with symptoms of an upper respiratory infection are more likely to be colonized with GAS rather than to have streptococcal pharyngitis. In an effort to promote antibiotic stewardship and avoid unnecessary treatments, caution should be used in obtaining and interpreting strep testing on children with clear viral respiratory symptoms.30 Oral clindamycin has been found to be successful to eradicate GAS carriage.
Rheumatic Fever/Rheumatic Heart Disease
Of special consideration in GAS infections is the development of rheumatic fever. Rheumatic fever is believed to be caused by an immunologic reaction to a preceding GAS infection, classically pharyngitis. In the United States, acute rheumatic fever is uncommon following a group A streptococcal skin infection.1 Interestingly, Australia reports a high frequency of rheumatic fever following a skin infection among some populations.31
The worldwide incidence of rheumatic fever/rheumatic heart disease varies significantly, with lower income/developing countries bearing the brunt of the burden. These variations likely are multifactorial. Increased crowding in developing countries allows for easier spread of GAS infections.1 Different strains of Streptococcus have varying abilities to cause rheumatic fever, so the prevalent strains of Streptococcus in a region can in part dictate the incidence of rheumatic fever. In addition, there appears to be a genetic component, as certain ethnic groups and families have an increased propensity to developing rheumatic fever.32
Rheumatic fever is thought to be mediated by an autoimmune process that is triggered by a pharyngeal GAS infection. The distinct features of rheumatic fever each are caused by a different autoimmune mechanism. Molecular mimicry, or the similarity between proteins of the bacteria and the tissue of the heart and brain, is thought to play a large role in the development of carditis and chorea. Arthritis is believed to be mediated by immune complex deposition, and the skin findings are thought to be caused by a delayed hypersensitivity reaction.31
The clinical manifestations and diagnostic criteria are summarized by the 2015 Modified Jones Criteria.33 No single feature (except for chorea) is 100% sensitive or specific for rheumatic fever, and the whole constellation of findings must be taken into account to make an accurate diagnosis.1 The United States and Canada both are considered low-risk populations and, thus, the discussion will focus on these criteria. There is a slightly different set of criteria for those living in a moderate or high-risk population.1
For the initial diagnosis of rheumatic fever, there should be laboratory evidence of a past GAS infection (elevated ASO titer or positive pharyngeal swab) except in chorea because of its long latency. The diagnosis of an initial attack of acute rheumatic fever requires the presence of two major modified Jones manifestations or one major plus two minor manifestations. For a recurrent attack, three minor manifestations can be diagnostic, in addition to the two previously described situations. Major criteria include the following: carditis, arthritis, chorea, erythema marginatum, and subcutaneous nodules. The minor criteria include polyarthralgia, fever (≥ 38.5°C), erythrocyte sedimentation rate (ESR) ≥ 60 mm in the first hour and/or C reactive protein (CRP) ≥ 3.0 mg/dL, and prolonged PR interval, after accounting for age (unless carditis is a major criterion).34 Each of these major criteria will be discussed separately.
Carditis is responsible for much of the long-term morbidity and mortality associated with the disease. Mitral valve disease is the hallmark of untreated acute rheumatic fever. Mitral and aortic regurgitation may be present. Pericarditis and myocarditis also may be seen.34
Sydenham chorea occurs in a small percentage of patients. It is characterized by involuntary movements, facial grimacing, and incoordination.1 Because of a long latency period, chorea may not be present at the time of the acute illness. It can occur up to eight months after the initial infection. Chorea may be bilateral or unilateral. The following three physical examination signs may be present: milkmaid’s grip, spooning sign, and pronator sign.34
Erythema marginatum is a serpiginous and macular rash with central pallor. It typically is most pronounced on the trunk and extremities.1 Key features include the absence of lesions on the face, rapidly moving lesions that may come and go, and a rash that is not pruritic or painful. Erythema marginatum typically is seen in conjunction with carditis.34
Arthritis is the most common, affecting approximately 75% of those with acute rheumatic fever. The arthritis typically is migratory, involving multiple joints, mainly large joints.1 Symptoms of joint swelling and pain typically improve significantly with aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs). Other causes, such as septic arthritis, are to be excluded. Aspiration of a joint typically will reveal < 100,000 white blood cells (WBC)/mm3.34
Subcutaneous nodules are the least common finding in acute rheumatic fever. Additionally, they frequently occur in conjunction with other findings, such as carditis. The nodules typically are not painful. They tend to occur over extensor surfaces of joints.34
The treatment of acute rheumatic fever first involves eradicating the GAS infection with penicillin. The remainder of treatment is focused on symptomatic relief. Acetaminophen or NSAIDs may be used to help with joint pain and fever. In the case of carditis and heart failure, fluid restriction, diuretics, and angiotensin converting enzyme (ACE) inhibitors may be used. Steroids also may be used as an adjunct to reduce inflammation.35 It is crucial to continue antibiotic prophylaxis in patients with a definitive diagnosis of acute rheumatic fever and rheumatic heart disease.
Recognizing and treating acute rheumatic fever is critical because, if unrecognized, it can lead to longstanding rheumatic heart disease, ultimately culminating in heart failure and death in the most severe cases. Given that there is an excess of disease burden in lower income countries, which often lack a comprehensive disease monitoring system, the true worldwide morbidity and mortality from rheumatic fever are unknown.32
Post-Streptococcal Glomerulonephritis
Post-infectious glomerulonephritis can occur after any infection, but classically occurs after a GAS infection. It is thought to be caused by an immune-mediated process. It can occur after either pharyngitis or impetigo. It typically will occur several weeks following the antecedent infection. As a result, patients may not recall the inciting infection.36
The clinical features of post-
streptococcal glomerulonephritis, in order from most common to least common, are edema, hypertension, and gross hematuria. Given that the Streptococcus infection typically precedes glomerulonephritis, tests such as ASO titers and anti-DNase B may be used to establish the presence of a recent streptococcal infection. A C3 complement level typically is low.37
The disease usually is self-limited, with symptoms resolving within a few weeks in the vast majority of patients. However, it should be noted that microscopic hematuria may continue to be present for up to several years in the absence of other symptoms.37 In a small subset of patients, the disease can be severe, including progression to rapidly progressive glomerulonephritis. Characteristics that place patients at high risk for rapidly progressive glomerulonephritis include estimated glomerular filtration rate (eGFR) < 18, C3 level < 0.03, age > 10 years, presence of nephrotic range proteinuria, and illness duration greater than two weeks.38
Treatment of post-streptococcal glomerulonephritis is mainly supportive. In patients with edema or fluid overload, loop diuretics can be helpful.39 Hypertension often is treated with a calcium channel blocker. Caution should be used regarding ACE inhibitors because they can further reduce glomerular filtration, which already is affected by the disease itself.36 In the most extreme cases, dialysis or renal transplant may be required.39
Unless there is an active infection, antibiotics typically are not a part of treatment. Unfortunately, treatment of Streptococcus infections with antibiotics does not seem to reduce the risk of subsequently developing glomerulonephritis.36
Henoch-Schonlein Purpura
Henoch-Schonlein purpura (HSP) is a unique post-infectious process that commonly affects children. HSP is an immunoglobulin A (IgA) mediated vasculitis. While it is not specific to GAS and may be triggered by any illness, a preceding streptococcal infection is the most identified trigger.
HSP is characterized by purpura or petechiae on the lower extremities. (See Figure 8.) In addition to the classic rash, abdominal pain and joint pain are other common symptoms. Like post-streptococcal glomerulonephritis, it is a self-limited process and typically only requires supportive care. A small percentage of those affected go on to have chronic renal disease or require renal transplant.
Figure 8. Henoch- Schonlein Purpura |
 |
Image used with permission from Dr. Janani Sankar, Kanchi Kamakoti CHILDS Trust Hospital, Chennai, India. |
It should be noted that there is an increased risk of intussusception with HSP, so children presenting with abdominal pain and other features concerning for HSP should be evaluated carefully for intussusception.40
Because of the possibility of chronic renal disease, close follow-up is essential, including referral to a nephrologist if renal involvement is evident.
Tonsillectomy
Tonsillectomies typically are performed for sleep apnea disorders and recurrent tonsillar infection. A tonsillectomy may be considered for those patients with frequent, recurrent tonsillitis. While there are several sets of criteria and guidelines available, the Paradise criteria frequently are used for children.41 Seven or more episodes in one year, five or more each year for two years, or three or more each year for three years are indications for tonsillectomy. Additionally, the criteria stipulate that each episode of tonsillitis should have been evaluated by a physician and adequately treated.
Guidelines for tonsillectomy in adults are not as well established, but most are based on the Paradise criteria.42 Tonsillectomy in adults has been shown to be effective at reducing the rate of subsequent tonsillitis.43
Intracranial Complications of Streptococcal Infections
It is of paramount importance to recognize some of the most serious complications from GAS infection involve the CNS. There has been renewed focus because of the increase in invasive streptococcal infections worldwide, including brain empyema.
Group A streptococci can cause brain abscesses and serious intracranial infections. Similar to what has been discussed with other invasive streptococcal infections, the incidence of pediatric intracranial infections has increased following the lifting of COVID-19 restrictions.44 Intracranial infections include brain abscess and epidural or subdural empyema.
Brain abscesses are most commonly caused by streptococci and Staphylococcus.45,46 However, rather than GAS, the predominant species is Streptococcus anginosus. While Streptococcus anginosus is the most common bacteria, the infections are polymicrobial, particularly when there is associated sinusitis. Preceding sinusitis can lead to a frontal lobe abscess. Untreated mastoiditis and otitis media can lead to temporal lobe or cerebellar abscesses.
Symptoms typically have an indolent onset, starting with low fevers and headache, and progressing to vomiting and neurologic changes. A head CT or magnetic resonance imaging (MRI) of the brain allows for an accurate diagnosis. See Figures 9 A-B for a brain MRI that depicts the typical findings of abscesses secondary to Streptococcus. Figures 10 A-C show a classic epidural abscess. Given the possibility of elevated intracranial pressure, lumbar puncture should be avoided because of the risk of herniation.
Figure 9A. Brain Magnetic Resonance Imaging Enhancement of Abscesses |
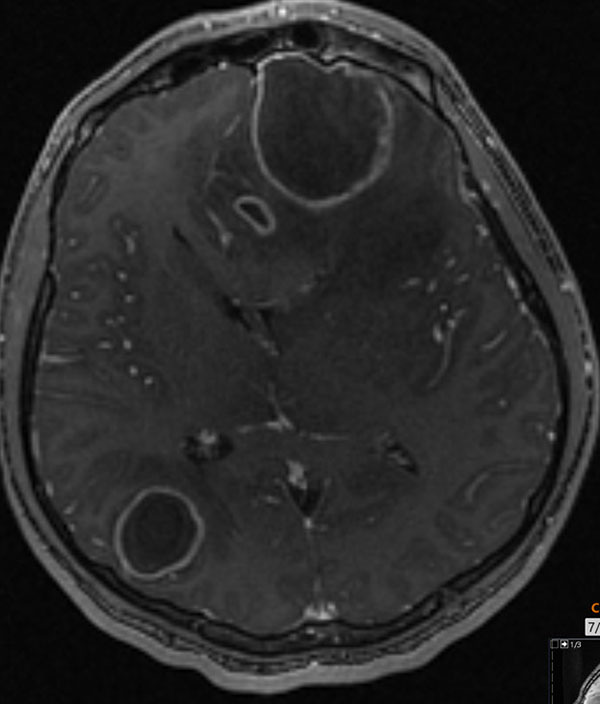 |
Brain magnetic resonance imaging post-contrast T1 depicting rim enhancement of abscesses Used with permission from Sean Kelleher, MD, Dayton Children’s Hospital. |
Figure 9B. Brain Magnetic Resonance Imaging with Fluid and Edema |
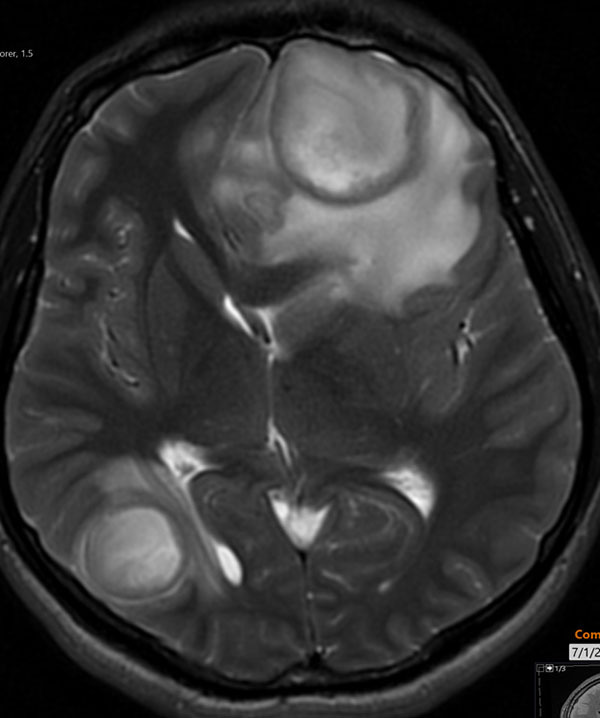 |
Brain magnetic resonance imaging T2 showing complex fluid within the lesion and extensive adjacent edemas Used with permission from Sean Kelleher, MD, Dayton Children’s Hospital. |
Figure 10A. Epidural Abscess |
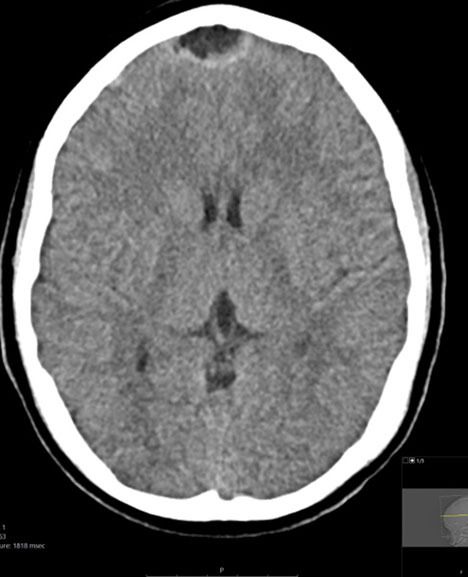 |
Axial contrast-enhanced computed tomography of a midline epidural abscess Used with permission from Mark Warren, DO, Dayton Children’s Hospital. |
Figure 10B. Epidural Abscess |
 |
Sagittal contrast-enhanced computed tomography of a midline epidural abscess Used with permission from Mark Warren, DO, Dayton Children’s Hospital. |
Figure 10C. Epidural Abscess |
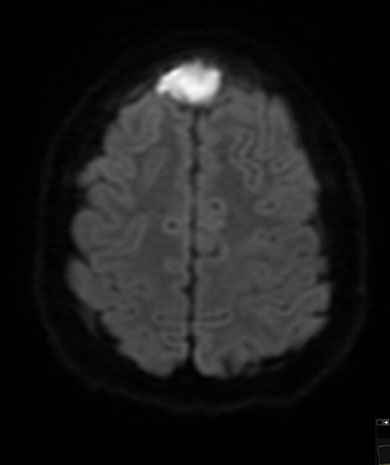 |
Diffusion-weighted magnetic resonance imaging of midline epidural abscess Used with permission from Mark Warren, DO, Dayton Children’s Hospital. |
Prompt antibiotics and neurosurgical consultation are the keys to treatment.45 Empiric broad-spectrum antibiotics covering gram-positive, gram-negative, and anaerobic infections should be started soon as possible.47 Metronidazole in combination with a third-generation cephalosporin (ceftriaxone, ceftazidime) is a common regimen. Vancomycin should be considered for methicillin-resistant Staphylococcus aureus (MRSA) coverage. Steroids are necessary to treat cerebral edema and associated vasculitis.
Most patients with brain abscess will require surgical intervention, such as drainage of abscess, and complete excision may be necessary for increased intracranial pressure. Removal of pus often is difficult because of its adherence to brain tissue. Antibiotics may be needed for six to eight weeks, and the duration is to be determined based on clinical improvement and inflammatory markers. Those with a small fluid collection (less than 2.5 cm) may improve with medical management alone, but this decision should be made in conjunction with a neurosurgeon.46
While microbial clearance may be achieved, the outcome largely is dependent on various factors, such as persistence of increased intracranial pressure, and complications, such as venous thrombosis or infarction.
Necrotizing Fasciitis
While Clostridium species have been implicated understandably for gas gangrene and fasciitis, GAS infections are most associated with this devastating and serious complication. Necrotizing fasciitis and myositis have a very high mortality of 8% to 15% and can result in loss of limbs.
The initial symptoms could be nonspecific. Muscle aches and skin changes could be minimal initially, and skin findings could be similar to erysipelas or cellulitis.48 Severe pain out of proportion to the appearance and sudden worsening should alert the provider to the possibility of necrotizing fasciitis. These symptoms may portend development of high compartment pressures and soft tissue and muscular necrosis.
Urgent surgical management, particularly fasciotomy and debridement as appropriate, guided by CT or MRI, is of paramount importance. Group A streptococcal fasciitis is not gas-forming and, hence, free air is not to be detected in imaging studies. Clindamycin should be given along with penicillin since clindamycin can reduce toxin production.49
Group B Streptococcus
A brief discussion is warranted regarding group B Streptococcus (GBS). GBS, also known as Streptococcus agalactiae, is a significant cause of neonatal morbidity and mortality. Among infants with early onset sepsis (within the first seven days of life), GBS often is implicated and is associated with bacteremia and meningitis. Pneumonia and urinary tract infection are seen less frequently.
Maternal screening for colonization with GBS and treatment with antibiotics prior to delivery in those who are GBS-positive have reduced the incidence of serious sepsis in infants within the first seven days of life (early onset). However, pretreatment with antibiotics does not seem to make an impact on the incidence of late-onset sepsis (after seven days). Therefore, a high index of suspicion must be maintained, even for those infants whose mothers were appropriately treated for GBS. Preterm infants and those exposed to human immunodeficiency virus (HIV) are at particular risk of developing late-onset GBS infections.
GBS is susceptible to penicillin or ampicillin, although expanded coverage at the initial presentation is necessary until the bacteria is identified.50
Summary
Scarlet fever and invasive streptococcal infections represent a significant cause of morbidity and mortality, particularly in the pediatric population. Since not all of the immune-mediated complications are preventable by a complete course of antibiotics, these disease manifestations must be considered in all children with a preceding streptococcal infection irrespective of treatment. As the frequency, manifestations, and severity of invasive infections continue to evolve in the post-COVID-19 pandemic era, brain abscesses and other invasive infections are becoming a more frequent occurrence. It is imperative that healthcare workers understand these complications and maintain a high index of suspicion.
REFERENCES
- Shulman S, Reuter C. Group A Streptococcus. In: Kliegman R, Stanton B, St Geme JW, et al, eds. Nelson Textbook of Pediatrics. Edition 21. Elsevier Inc.; 2020:1440-1450.
- Lindgreen C, Fine A. Sore Throat. In: Shaw KN, Bachur RG, eds. Fleisher & Ludwig’s Textbook of Pediatric Emergency Medicine. 8th edition. Wolters Kluwer; 2021:508-511.
- Hand R, Snelling T, Carapetis J. Group A Streptococcus. In: Ryan ET, Hill DR, Solomon T, et al, eds. Hunter’s Tropical Medicine and Emerging Infectious Diseases. Tenth edition. Elsevier; 2020:429-438.
- Brouwer S, Rivera-Hernandez T, Curren BF, et al. Pathogenesis, epidemiology and control of group A Streptococcus infection. Nat Rev Microbiol 2023;21:431-447.
- Sims Sanyahumbi A, Colquhoun S, Wyber R, Carapetis JR. Global disease burden of group A Streptococcus. In: Ferretti JJ, Stevens DL, Fischetti VA, editors. Streptococcus pyogenes: Basic Biology to Clinical Manifestations. University of Oklahoma Health Sciences Center; 2016.
- Hurst JR, Brouwer S, Walker MJ, McCormick JK. Streptococcal superantigens and the return of scarlet fever. PLoS Pathog 2021;17:e1010097.
- Kimberlin DW, Barnett ED, Lynfield R, Sawyer MH, eds. Group A streptococcal infections. In: Red Book: 2021-2024 Report of the Committee on Infectious Diseases. 32nd edition. American Academy of Pediatrics; 2021:694-707.
- Aalbers J, O’Brien KK, Chan WS, et al. Predicting streptococcal pharyngitis in adults in primary care: A systematic review of the diagnostic accuracy of symptoms and signs and validation of the Centor score. BMC Med 2011;9:67.
- Kanagasabai A, Evans C, Jones HE, et al. Systematic review and meta-analysis of the accuracy of McIsaac and Centor score in patients presenting to secondary care with pharyngitis. Clin Microbiol Infect 2024;30:445-452.
- Pallon J, Rööst M, Sundqvist M, Hedin K. The aetiology of pharyngotonsillitis in primary health care: A prospective observational study. BMC Infect Dis 2021;21:971.
- Peachey MH, Kubow KE, Blyer KB, Halterman JA. Use of saliva-based qPCR diagnostics for the accurate, rapid, and inexpensive detection of strep throat. Diagnosis 2024;11:178-185.
- van Driel ML, De Sutter AI, Thorning S, Christiaens T. Different antibiotic treatments for group A streptococcal pharyngitis. Cochrane Database Syst Rev 2021;3:CD004406.
- Shulman ST, Bisno AL, Clegg HW, et al; Infectious Diseases Society of America. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis 2012;55:e86-e102.
- Pellegrino R, Timitilli E, Verga MC, et al. Acute pharyngitis in children and adults: Descriptive comparison of current recommendations from national and international guidelines and future perspectives. Eur J Pediatr 2023;182:5259-5273.
- Kliegman R, Stanton B, St Geme JW, et al, eds. Invasive Group A Streptococcus. In: Nelson Textbook of Pediatrics. Edition 21. Elsevier Inc.; 2020:xlii.
- Metz C, Schmid A, Veldhoen S. Increase in complicated upper respiratory tract infection in children during the 2022/2023 winter season — a post coronavirus disease 2019 effect? Pediatr Radiol 2023;54:49-57.
- Stevens D, Bryant A. Streptococcus pyogenes impetigo, erysipelas, and cellulitis. In: Ferretti JJ, Stevens DL, Fischetti VA, eds. Streptococcus Pyogenes: Basic Biology to Clinical Manifestations. 2nd ed. University of Oklahoma Health Sciences Center; 2022. http://www.ncbi.nlm.nih.gov/books/NBK587111/
- Leung AK, Barankin B, Lam JM, Leong KF. Childhood guttate psoriasis: An updated review. Drugs Context 2023;12:2023-8-2.
- Zhang H, Dong J, Huang J, et al. Evaluating antibiotic regimens for streptococcal toxic shock syndrome in children. PLoS One 2023;18:e0292311.
- Kimberlin DW, Barnett ED, Lynfield R, Sawyer MH, eds. Red Book: 2021-2024 Report of the Committee on Infectious Diseases. 32nd edition. American Academy of Pediatrics; 2021.
- Laho D, Blumental S, Botteaux A, Smeesters PR. Invasive group A streptococcal infections: Benefit of clindamycin, intravenous immunoglobulins and secondary prophylaxis. Front Pediatr 2021;9:697938.
- Peetermans M, Matheeussen V, Moerman C, et al. Clinical and molecular epidemiological features of critically ill patients with invasive group A Streptococcus infections: A Belgian multicenter case-series. Ann Intensive Care 2024;14:19.
- Casey J, Keidel S, Kudo M, Chan M. Management protocol for uncomplicated peritonsillar abscess: Standardizing care and improving emergency medicine resident confidence. Cureus 2024;16:e53223.
- Saar M, Vaikjärv R, Parm Ü, et al. Unveiling the etiology of peritonsillar abscess using next generation sequencing. Ann Clin Microbiol Antimicrob 2023;22:98.
- Black DL, Sears R. Peritonsillar abscess. JAAPA 2024;37:1-2.
- Long B, Gottlieb M. Managing peritonsillar abscess. Ann Emerg Med 2023;82:101-107.
- Heilig Y, Sapir A, Yafit D, et al. Impact of the COVID‐19 era on clinical presentation, management and microbiology in paediatric peritonsillar abscess: A case-control study. Clin Otolaryngol 2024;49:207-213.
- Herrera AL, Potts R, Huber VC, Chaussee MS. Influenza enhances host susceptibility to non-pulmonary invasive Streptococcus pyogenes infections. Virulence 2023;14:2265063.
- De Beir J, Lucas M, Jesus AR, et al. Postpandemic rebound in noninvasive group a streptococcal disease is not synchronous with winter RSV and influenza epidemics. Pediatr Infect Dis J 2024;43:e106-e108.
- Rick AM, Zaheer HA, Martin JM. Clinical features of group A Streptococcus in children with pharyngitis: Carriers versus acute infection. Pediatr Infect Dis J 2020;39:483-488.
- Guilherme L, Steer A, Cunningham M. Pathogenesis of acute rheumatic fever. In: Dougherty SD, Carapetis J, Zühlke L, Wilson N, eds. Acute Rheumatic Fever and Rheumatic Heart Disease. Elsevier; 2021:1-18.
- Watkins D, Baker M, Kumar R, et al. Epidemiology, risk factors, burden and cost of acute rheumatic fever and rheumatic heart disease. In: Dougherty SD, Carapetis J, Zühlke L, Wilson N, eds. Acute Rheumatic Fever and Rheumatic Heart Disease. Elsevier; 2021:19-30.
- Gewitz MH, Baltimore RS, Tani LY, et al. Revision of the Jones Criteria for the diagnosis of acute rheumatic fever in the era of Doppler echocardiography: A scientific statement from the American Heart Association. Circulation 2015;131:1806-1818.
- Dougherty S, Nascimento B, Carapetis J. Clinical evaluation and diagnosis of acute rheumatic fever. In: Dougherty SD, Carapetis J, Zühlke L, Wilson N, eds. Acute Rheumatic Fever and Rheumatic Heart Disease. Elsevier; 2021:31-54.
- Cilliers A, Sadiq M. Management of acute rheumatic fever. In: Dougherty SD, Carapetis J, Zühlke L, Wilson N, eds. Acute Rheumatic Fever and Rheumatic Heart Disease. Elsevier; 2021:44-67.
- Iyengar A, Kamath N, Radhakrishnan J, Estebanez BT. Infection-related glomerulonephritis in children and adults. Semin Nephrol 2023;43:151469.
- Dhakal AK, Shrestha D, Singh SK, Acharya S. Clinical profile of children with acute post-streptococcal glomerulonephritis. Pediatr Nephrol 2023;38:3327-3336.
- Karakaya D, Güngör T, Çakıcı EK, et al. Predictors of rapidly progressive glomerulonephritis in acute poststreptococcal glomerulonephritis. Pediatr Nephrol 2023;38:3027-3033.
- Rodriguez-Iturbe B, Haas M. Post-Streptococcus pyogenes glomerulonephritis. In: Ferretti JJ, Stevens DL, Fischetti VA, eds. Streptococcus Pyogenes: Basic Biology to Clinical Manifestations. 2nd ed. University of Oklahoma Health Sciences Center; 2022. http://www.ncbi.nlm.nih.gov/books/NBK587111/
- Fan GZ, Li RX, Jiang Q, et al. Streptococcal infection in childhood Henoch-Schönlein purpura: A 5-year retrospective study from a single tertiary medical center in China, 2015-2019. Pediatr Rheumatol Online J 2021;19:79.
- Paradise JL, Bluestone CD, Bachman RZ, et al. Efficacy of tonsillectomy for recurrent throat infection in severely affected children. Results of parallel randomized and nonrandomized clinical trials. N Engl J Med 1984;310:674-683.
- Houborg HI, Klug TE. Evaluation of guidelines for tonsillectomy in adults with recurrent acute tonsillitis. Ann Otol Rhinol Laryngol 2023;132:1573-1583.
- Tzelnick S, Hilly O, Vinker S, et al. Long-term outcomes of tonsillectomy for recurrent tonsillitis in adults. Laryngoscope 2020;130:328-331.
- Bauer S. Increased pediatric intracranial infections. In: Kliegman R, Stanton B, St Geme JW, et al, eds. Nelson Textbook of Pediatrics. Edition 21. Elsevier Inc.; 2020:xlii.
- Janowski A, Hunstad D. Brain abscess. In: Kliegman R, Stanton B, St Geme JW, et al, eds. Nelson Textbook of Pediatrics. Edition 21. Elsevier Inc.; 2020:3235-3236.
- Corsini Campioli C, Castillo Almeida NE, O’Horo JC, et al. Bacterial brain abscess: An outline for diagnosis and management. Am J Med 2021;134:1210-1217.e2.
- Smiljkovic M, Tat J, Richardson SE, et al. A 20-year study of intracranial pyogenic complications of sinusitis in children. Pediatr Infect Dis J 2024;43:91-96.
- Hourmozdi JJ, Hawley DA, Hadi CM, et al. Streptococcal necrotizing myositis: A case report and clinical review. J Emerg Med 2014;46:436-442.
- Horn DL, Roberts EA, Shen J, et al. Outcomes of β-hemolytic streptococcal necrotizing skin and soft-tissue infections and the impact of clindamycin resistance. Clin Infect Dis 2021;73:e4592-e4598.
- Coggins SA, Puopolo KM. Neonatal group B Streptococcus disease. Pediatr Rev 2024;45:63-73.
While most physicians are familiar with the common presentations of streptococcal infections (e.g., pharyngitis, impetigo), it is important to recognize the carrier state, learn management of common complications (e.g., peritonsillar abscess), and identify the potentially serious, and perhaps deadly, complications and invasive infections.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.

