
Pediatric Burn Care: Strategies for Identification and Treatment
AUTHORS
Claire Ashley Justin, MD, Department of Pediatrics, Lucile Salter Packard Children’s Hospital, Stanford School of Medicine, Palo Alto, CA
Guillermo A. De Angulo, MD, MSCR, Clinical Assistant Professor of Emergency Medicine, Stanford University School of Medicine, Palo Alto, CA
Mia L. Karamatsu, MD, Assistant Professor of Emergency Medicine and Pediatrics, Stanford University School of Medicine, Stanford, CA
PEER REVIEWER
Steven M. Winograd, MD, FACEP, Attending Emergency Physician, Trinity Health Care, Samaritan, Troy, NY
Executive Summary
- According to American Burn Association (ABA) guidelines, a patient with an electrical burn from a high-voltage source (> 1,000 V; for example, a stun gun) or lightning strike should be transferred to a burn center.
- Household electrical burns are much more common than electrical burns caused by lightning strikes. Pediatric patients have not demonstrated serious cardiac injury from household electrical burns and typically do not require initial electrocardiogram or cardiac monitoring.
- Burn depths are classified as superficial, superficial partial thickness, and deep partial thickness burns.
- Methods of estimating total body surface area (TBSA) in children are imperfect and are still an active area of study. The Lund and Browder chart is the most accurate tool for assessment.
- In any child with possible inhalational injury and concern for progressive edema of the airway or if there are breath sounds suggesting airway obstruction (e.g., stridor and wheezing), then endotracheal intubation should be performed with a cuffed tube.
- In children, the two most commonly used formulas for initial resuscitation are the Shriners-Cincinnati and Galveston formulas. The Shriners-Cincinnati formula calls for different protocols based on patient age. For older children, initial resuscitation should consist of lactated Ringer’s solution (LR) 4 mL/kg/%burn + 1,500 mL/m² TBSA. Half of the total volume should be given in the first eight hours and the rest over the next 16 hours.
- For younger children, the Shriners-Cincinnati formula calls for 4 mL/kg/%burn + 1,500 mL/m² TBSA of fluids total in the first 24 hours. LR with 50 mEq sodium bicarbonate (NaHCO3) should be used in the first eight hours, then LR for the next eight hours, and finally 5% albumin in LR for the next eight hours. The Galveston formula states that children should receive LR 5,000 mL/m2 burn + 2,000 mL/m2 total with 12.5 mg of 25% albumin per liter of crystalloid over 24 hours. The first half of the total volume should be given in the first eight hours and the second half over the next 16 hours.
- Although it is important to take the initial history in a non-judgmental fashion, child abuse should be considered in every burn evaluation. Burn injuries may represent non-accidental trauma. As with any traumatic injury, it is important to correlate the mechanism of injury with the developmental stage of the child. Certain types of burns, such as ones that spare the flexor surfaces or those that are pattern injuries, should be evaluated closely for potential child abuse.
- Undertreated pain in burn patients has been shown to lead to profound adverse psychological consequences, including post-traumatic stress disorder symptoms, anxiety, and stress.
Pediatric burn injuries, especially minor, are an essential part of caring for children. Classification of the depth of injury, recognition of nonaccidental trauma, and appropriate care are all critical aspects of management. The authors comprehensively review pediatric burn care.
— Ann M. Dietrich, MD, FAAP, FACEP, Editor
Introduction and Epidemiology
In the United States, fire and burns are still among the top 10 causes of unintentional injury deaths among people 19 years of age and younger.1 More than 1 million emergency department visits from 2011-2020 were because of pediatric burn injuries.2 Children especially are vulnerable to burns because of still-maturing motor and cognitive skills as well as dependence on adults for supervision and danger avoidance.3
Even within the pediatric population, morbidity and mortality from burn injuries are especially important for certain vulnerable subgroups. Although major advancements in burn care have reduced the fatality rate for severe burns, burn injuries and deaths continue to disproportionately affect Black children, children in low-income households, and children in rural areas.3,4
Pediatric burns are most likely to occur in the household setting. Household items, such as exposed electrical outlets, stoves, candles, and heaters, can pose a danger to children. Furthermore, hot liquids around the house, such as hot coffee, cooking oil, or bath water, also can cause burns. Children are more likely to experience minor burn injuries, although these also may require medical care. Education for families around injury prevention strategies and maintaining a safe home environment for children is important to review when the opportunity arises. Given the prevalence of burn injuries in the pediatric population, caring for pediatric burn injuries is an important skill for providers in the emergency setting.
Burn Mechanisms
Thermal
Thermal burns are the most common burn mechanism seen in the emergency department. Thermal burns are injuries to the skin caused by contact with a hot surface, liquid, or flame. Scald injuries from hot liquids are the most common cause of burns in children younger than 5 years of age.3,5 It often is underestimated how long children can be exposed to hot liquids before they become burned. Safe bathwater temperature is 100°F. Dangerously high temperatures may occur if limits are not set on the water heater.3 Another source of scald injuries is exposure to hot water or oil in the kitchen. Children should be carefully supervised when in the kitchen, especially when removing items from the microwave or around individuals boiling water or cooking with oil. In particular, scalds from hot milk have been shown to cause more extensive tissue damage than those from hot water.6,7
Children also can receive thermal burns from contact with hot objects, such as radiators, stovetops, or metal that has been in sunlight. Flame burns can occur with contact with cigarettes, candles, or house fires. It is important to elicit the mechanism of a thermal burn as part of a thorough history. These burns, in addition to being the most common in children, also are the most common type of burn seen in child abuse. For more information on burns in child abuse, refer to the subsection on this topic.
Electrical
Less common than thermal burns, electrical burns are caused by an electric current going through the body and damaging the skin and other organs. These burns often are caused by contact with voltage-containing objects or by lightning strikes. According to American Burn Association (ABA) guidelines, a patient with an electrical burn from a high-voltage source (> 1,000 V; for example, a stun gun) or lightning strike should be transferred to a burn center. Patients with injury from a low-voltage source (< 1,000 V; for example, a household outlet) should receive consultation and possible follow-up at a burn center.8
Multi-organ failure, a leading cause of mortality in pediatric burn patients, is less common with electrical burns than it is with thermal burns. This is thought to be because of early removal of non-viable tissue in electrical burn patients.9 Household electrical burns are much more common than electrical burns caused by lightning strikes. Pediatric patients have not demonstrated serious cardiac injury from household electrical burns and typically do not require initial electrocardiogram or cardiac monitoring.10
Chemical
Chemical burns are uncommon but may require transfer to a burn center.8 These have devastating consequences and may be caused by acids or alkalis making contact with the skin or eyes. Among children, this often is caused by unintentional exposure to household chemicals, particularly cleaning agents.
Irrigation with large amounts of water is of paramount importance as the first step in treating most cutaneous chemical burns.11 An exception to this rule is for elemental metals, such as sodium, lithium, and potassium, which will ignite upon contact with water.12 In this case, it is important to apply oil to the area to prevent water exposure. Phenol and certain acids and bases also should not be removed with water and require specific methods of removal.12
Pathophysiology of Burns
The skin is the body’s largest organ and serves as a protective barrier against infection, dehydration, and hypothermia. When this barrier is compromised by a burn, systemic dysfunction in these areas is more likely to occur. Children are already at greater risk of dehydration and hypothermia compared to adults because of their immature renal concentration abilities, larger body surface area to mass ratios, and thinner skin (approximately 70% the thickness of adult skin).
Locally, the vascular response to a burn is thrombosis and microvascular vasoconstriction in peripheral tissues. This is thought to partially explain the mechanism by which burns appear to deepen after the initial injury.13 Skin around the burn will necrose as a secondary response to the initial insult. Local mediators, such as prostaglandins, leukotrienes, and free radicals, will increase capillary leak resulting in tissue edema.14,15 This is especially important to consider in the pediatric population, since children have smaller airways and are more susceptible to occlusion by airway edema secondary to a burn.13
In the acute phase of a major burn injury (the first 48 hours), systemic vascular resistance increases, cardiac output decreases, organ perfusion decreases, and the patient is in a hypovolemic state.14,16 This may lead to multi-organ system dysfunction. Systemic pro-inflammatory cytokines are upregulated after a burn, resulting in the release of stress hormones and creating a hypermetabolic state three to five days after a major burn.14 Given that children have higher energy needs per kilogram than adults, particular care should be given to prevent a catabolic state. Early nutrition should be considered, although that is out of the scope of the emergency phase of care.17
Burn Depth
Superficial
Superficial burns are dry, erythematous, and blanching. They are not considered in calculations of total body surface area (TBSA) of a burn. A common superficial burn is a sunburn.
Superficial Partial Thickness
Superficial partial thickness burns appear moist, erythematous, vesicular/bullous, and blanching. These burns and deeper ones are considered in TBSA calculations. These burns are confined to the epidermis and often very painful because the nerve endings in the dermis have been exposed.
Deep Partial Thickness
Deep partial thickness burns, which affect the dermis, are drier, paler, and less painful than superficial partial thickness burns. The burn damages the nerve endings and vascular perfusion to the epidermis.
Full Thickness
Full thickness burns are leathery and dry. There is complete loss of sensation to sharp and light touch in full thickness burns.
Fourth-Degree Burns
A fourth-degree burn extends into the muscle and bone. The area often appears charred.
Extent of the Burn Surface
The extent of the burn surface is measured in TBSA of the affected area. Estimating the TBSA is important because it affects not only fluid resuscitation calculations but also management decisions, including transfer to a burn center. Children have proportionally larger heads and smaller limbs than adults do, so some methods of estimating burn surface area in adults have been modified to more accurately reflect pediatric body proportions.18 Methods of estimating TBSA in children are imperfect and are still an active area of study. In fact, studies have shown that burn area in children often is misestimated and has led to unnecessary burn center transfers and miscalculations of fluid needs.19,20
New technology is being developed to increase the accuracy of burn surface estimates, so advancements in technology may replace more traditional methods of estimating TBSA of burns in pediatric patients. Regardless, it is important to understand quick and readily available ways of estimating burn area. Three of the most common methods are outlined in the following sections.
Lund and Browder Chart
The Lund and Browder Chart, developed in the 1940s, assigns certain percentages to segments of the body based on children’s age ranges. (See Figure 2.)21 Although the average pediatric body mass index (BMI) has increased since the 1940s, evidence shows that the Lund and Browder chart still is adequate for estimating TBSA, even with changes to average BMI in the pediatric population.22 As a reminder, areas of simple erythema (superficial burn without blistering or skin loss) should not be included in TBSA calculations.23
Figure 2. General Rule of Nines and Lund and Browder Charts |
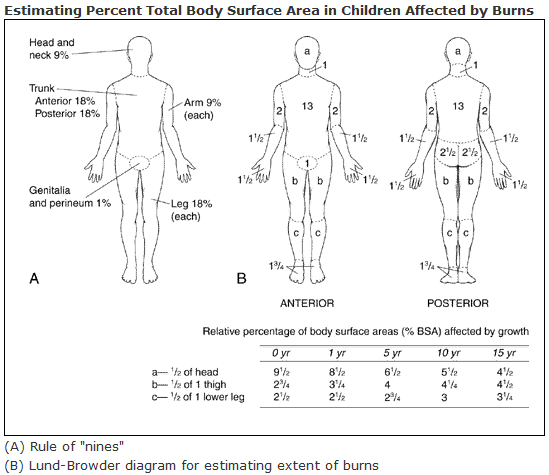 |
Source: U.S. Department of Health and Human Services. Lund and Browder chart. Published April 24, 2013. https://en.wikipedia.org/wiki/Lund_and_Browder_chart |
(Wallace’s) Rule of Nines
The Rule of Nines, or Wallace’s Rule of Nines, assigns segments of the adult body percentages in multiples of nine. (See Figures 2 and 3.)21,24,25
Figure 3. Wallace’s Rule of Nines |
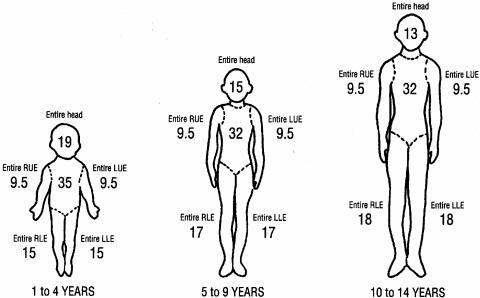 |
RUE: right upper extremity; LUE: left upper extremity; RLE: right lower extremity; LLE: left lower extremity Reprinted with permission from Church D, Elsayed S, Reid O, et al. Burn wound infections. Clin Microbiol Rev 2006;19:403-434. |
For children, the Rule of Nines assigns different percentages to account for the differences in pediatric body proportions compared to those of adults. Use the adult chart for children aged older than 14 years.
Rule of Palms
The Rule of Palms uses the size of a patient’s hand from distal wrist to distal fingers to be about 1% of TBSA. A common mistake in using the Rule of Palms is not including the length of the fingers in the estimate of TBSA.
One might also notice that the Lund and Browder chart directly contradicts the palmar method by estimating that the anterior hand is 1.5% of TBSA. Use of the Rule of Nines or the Lund and Browder chart is usually preferred over the Rule of Palms.20,26 However, the Rule of Palms still can be useful in the estimation of TBSA for scattered or smaller burns.27
Burn Patient Initial Care
No matter how severe the burn initially appears or what the mechanism of the burn is, children presenting with burn injuries to the emergency department should be evaluated using a methodical approach that includes a primary and secondary survey, as recommended by advanced trauma life support.
Primary Survey
Airway and Breathing: Inhalational Injuries and Carbon Monoxide Poisoning. Evaluation of the airway is of paramount importance in burn patients. As outlined previously, burns can cause airway edema and, therefore, obstruction of the airway. If there is concern for progressive edema or if there are breath sounds suggesting airway obstruction (e.g., stridor and wheezing), then endotracheal intubation should be performed with a cuffed tube.13 This is an especially important consideration with smaller children, given their smaller airways. If a child with burn injury is intubated, it is important to maintain the security of the endotracheal tube via tie harnesses or other methods.13
Smoke inhalation also can lead to carbon monoxide toxicity. Recall that a pulse oximeter will not accurately reflect the patient’s oxygenation status. Patients who were trapped in enclosed spaces and have altered neurologic status should be tested for carbon monoxide and should have 100% oxygen administered to them for at least four hours.28
Circulation: Initial Fluid Resuscitation. Children with major burn injuries who may be transported to a burn center should have secure vascular access. If the burns cover a large body surface area, it is acceptable to insert a short-term intravenous or intraosseous line through a burn wound. The ABA recommends initial formal fluid resuscitation for patients with burns covering more than 20% of TBSA, preferably through the intravenous route.16
In children, the two most commonly used formulas for initial resuscitation are the Shriners-Cincinnati and Galveston formulas. The Shriners-Cincinnati formula calls for different protocols based on patient age.
For older children, initial resuscitation should consist of lactated Ringer’s solution (LR) 4 mL/kg/%burn + 1,500 mL/m² TBSA. Half of the total volume should be given in the first eight hours and the rest over the next 16 hours.
For younger children, the Shriners-Cincinnati formula calls for 4 mL/kg/%burn + 1,500 mL/m² TBSA of fluids total in the first 24 hours. LR with 50 mEq sodium bicarbonate (NaHCO3) should be used in the first eight hours, then LR for the next eight hours, and finally 5% albumin in LR for the next eight hours.
The Galveston formula states that children should receive LR 5,000 mL/m2 burn + 2,000 mL/m2 total with 12.5 mg of 25% albumin per liter of crystalloid over 24 hours. The first half of the total volume should be given in the first eight hours and the second half over the next 16 hours. These formulas are summarized in Table 1.29
Since children have lower hepatic glycogen stores than adults that are depleted after 12-14 hours of fasting, the ABA also recommends adding dextrose fluids in the first 24 hours or introducing early enteral nutrition.16,30 Inhalational injuries also increase the initial fluid resuscitation requirements to about 5.7 mL/kg/%burn.31
Table 1. Formulas for Fluid Resuscitation in Pediatric Burns29 |
|||
| Formula | Time | ||
| Hours 0-8 | Hours 8-16 | Hours 16-24 | |
Galveston |
Fluid: LR Quantity: 2,500 mL/m2 TBSA burn + 1,000 mL/m2 TBSA AND 12.5 g of 25% albumin per 1 liter of LR |
Fluid: LR Quantity: 2500 mL/m2 TBSA burn + 1,000 mL/m2 TBSA AND 12.5 g of 25% albumin per 1 liter of LR |
|
Shriners-Cincinnati (younger children) |
Fluid: LR + NaHCO3 Quantity: 2 mL/kg/% TBSA burn + 750 mL/m2 TBSA AND 50 mEq NaHCO3 |
Fluid: LR Quantity: 1 mL/kg/% TBSA burn + 375 mL/m2 TBSA |
Fluid: LR + 25% albumin Quantity: 1 mL/kg/% TBSA burn + 375 mL/m2 TBSA AND 12.5 g of 25% albumin per 1 liter of LR |
Shriners-Cincinnati (older children) |
Fluid: LR Quantity: 2 mL/kg/% TBSA burn + 750 mL/m2 TBSA |
Fluid: LR Quantity: 2 mL/kg/% TBSA burn + 750 mL/m2 TBSA |
|
LR: lactated Ringer's solution; TBSA: total body surface area |
|||
Disability and Exposure. As outlined previously, altered mental status should increase suspicion for carbon monoxide poisoning. During the primary survey, a patient’s clothing should be removed to assess for and prevent further injury (from thermal or chemical burns). Given that the skin is integral to the body’s ability to maintain thermal homeostasis, patients with severe burns are at increased risk for hypothermia. It is important to monitor core temperature and take measures to prevent hypothermia during initial resuscitation.
Secondary Survey
A secondary survey should be conducted that includes a comprehensive head-to-toe physical examination, history, and appropriate imaging.
Initial History. The initial history should include the mechanism of the burn and burn diagram. Clinicians should obtain tetanus vaccination history because prophylaxis may be necessary.32 Wound photography may be helpful for documentation.33 It is important to obtain information from collateral sources about the events leading up to the burn.
Burns in Child Abuse. Although it is important to take the initial history in a non-judgmental fashion, child abuse should be considered in every burn evaluation.13 Burn injuries may represent nonaccidental trauma.
As with any traumatic injury, it is important to correlate the mechanism of injury with the developmental stage of the child. Certain types of burns, such as ones that spare the flexor surfaces or those that are pattern injuries, should be evaluated closely for potential child abuse.35 (See Figure 4.) Other injuries on the body may indicate a history of nonaccidental trauma.35 If there is suspicion for child abuse, the patient should be admitted for further management regardless of burn severity.13
Figure 4. Burns and Injuries Indicating Child Abuse Rule34 |
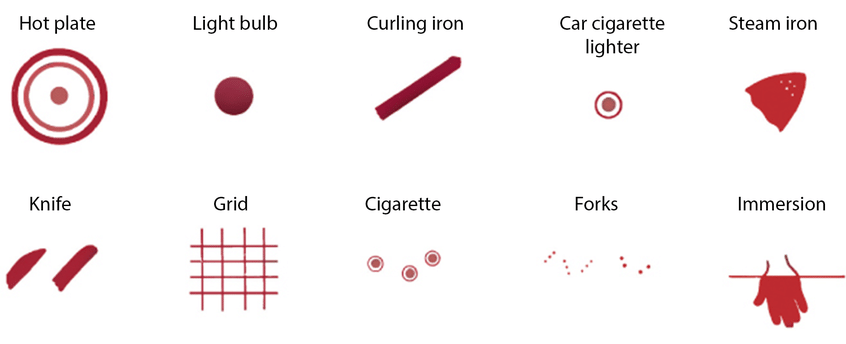 |
Reprinted with permission from Dubowitz H, Lane WG. Abused and neglected children. In: Kliegman RM, Stanton BF, St. Geme JW 3rd, Schor NF, eds. Nelson's Textbook of Pediatrics. 20th ed. Elsevier;236-244. |
Fluid Management. After initial fluid resuscitation, fluids should be titrated to achieve urine output of > 1 mL/kg/hour for children weighing less than 30 kg and > 0.5 mL/kg/hour for children weighing more than 30 kg.36 Other findings, such as capillary refill time, mental status, and vital signs, also are important for monitoring fluid status.
Circumferential Burns. When conducting the secondary survey, it is important to note burns that are circumferential or near circumferential around the torso or any limb. Circumferential burns can lead to an eschar that causes compartment syndrome of the areas distal to it.13 For circumferential wounds around the torso, this can cause poor ventilation and poor renal perfusion. Compartment syndrome in a limb can lead to peripheral nerve ischemia and muscle necrosis. If there is a circumferential burn, the affected area should be monitored frequently for signs of compartment syndrome. If the concern for compartment syndrome arises, then timely decompression is critical.
Analgesia. Only about 13% to 20% of pediatric burn patients treated with prehospital first aid are given analgesia.37 Undertreated pain in burn patients has been shown to lead to profound adverse psychological consequences, including post-traumatic stress disorder symptoms, anxiety, and stress.38 Acetaminophen commonly is used and has been shown to reduce pain scores in the days post-admission.39 Furthermore, acetaminophen is a safe choice in patients with burns.40
Nonsteroidal anti-inflammatory drugs (NSAIDs) are less favorable, given that the safety of NSAIDs has not been studied in pediatric burn patients, and their side effect profiles include renal toxicity and bleeding risk, for which patients with burns are already at higher risk.40
Opioids also commonly are used for analgesia in the pediatric population, although no studies have clearly found a specific opioid or standardized dosing parameters that are most effective for pediatric burn patients.40,41
Burn Patient Triage
The ABA has released criteria for referral to a large burn center. A study of pediatric emergency department visits for burn injuries in 2012 showed that more than 78% of children who meet criteria for referral to a burn center were seen in hospitals that have fewer than 20 burn admissions a year. However, only 8.2% of these patients were transferred.42 These data suggest that children often are under-referred to burn centers, even when they meet the criteria for transfer.
Burn Center Referral
The ABA’s guidelines for transfer and consultation to a burn center are summarized in Table 2. The guidelines are not meant to be strict parameters for referral but rather a group of characteristics that can be used as an aid to triaging.
Table 2. American Burn Association Burn Center Consultation Guidelines8 |
||
| Type of Injury | Immediate Consultation and Consideration for Transfer | Consider Consultation |
Thermal burns |
|
|
Inhalation injuries |
|
|
Electrical burns |
|
|
Chemical burns |
|
|
TBSA: total body surface area |
||
There is a special guideline addressing pediatric patients specifically (defined as patients younger or equal to 14 years of age or younger or weighing less than 30 kg). The guideline states that all pediatric patients may benefit from burn center referral. Burn size, mechanism, severity, and the patients’ families social, emotional, and psychological needs should be taken into account prior to making the decision to transfer, admit, or treat as an outpatient.
Outpatient Management
Most pediatric burns can be managed as an outpatient. Patients who are appropriate for outpatient management should have small burns without inhalational injury and should have a feasible follow-up plan in place.43 Follow-up plans should be suitable for the family’s available resources and comfort. Burns should be small enough to not require fluid resuscitation.43 There should not be concern for abuse or neglect.
Remember that close consultation with an inpatient burn unit is appropriate for any pediatric patient and can help emergency clinicians triage and develop appropriate follow-up. If a child has a circumferential wound or if they require surgical management, such as skin grafting, then they should be admitted to decrease delay in surgery and/or for close monitoring.43
Topical Agents and Dressing. Minor burns should be run under cool water for 20 minutes to decrease the spread of the injury.44 Wounds heal best in moist environments, so topical agents are important for treatment. For superficial burns, such as sunburns, topical agents, such as hypoallergenic lotion, aloe vera, honey, or antibiotic ointment, are sufficient to prevent drying as the skin heals.
Partial thickness burns should be treated with silver sulfadiazine or absorptive occlusive dressings.45 Absorptive dressing options include Aquacel Ag and hydrocolloid dressings, such as Duoderm and Urgotul. Notably, silver sulfadiazine is contraindicated in newborns and patients with sulfa allergies. Also, a randomized control trial has shown silver sulfadiazine is inferior in both pain metrics and time to healing compared to an absorptive dressing.46 Another randomized controlled trial in the pediatric population showed that use of Mepilex Ag leads to shorter re-epithelialization times (compared to Acticoat with Mepitel) and decreased pain during dressing changes (compared to Acticoat).47 The most optimal dressing to use for partial thickness burns is still an active area of research. However, it is generally appropriate to use a moist occlusive dressing, such as Aquacel Ag, Mepilex Ag, or Acticoat.
Most small burns can be managed with daily dressing changes and wound care.43 Families should feel comfortable with dressing changes and wound care prior to being discharged from the acute care setting. Burn wounds are only appropriate for outpatient treatment if there is low concern for future development of ischemia. Pain management is an important consideration, especially around dressing changes. Often, children being treated as an outpatient have pain adequately managed via oral narcotic given 30 minutes prior to dressing change.43
Follow-Up. The timing of follow-up appointments depends on the wound and the family’s comfort with the outpatient care plan. Most children should be seen at least twice weekly initially, and some may need to be seen daily.43 Follow-up visits should include evaluation of the wound, cleansing, and re-dressing. The burn care plan and return precautions should be discussed at every follow-up. Return precautions include delayed wound healing, signs of infection, escalating pain or anxiety with dressing changes, difficulty enacting follow-up plan, and inability to maintain adequate oral hydration.
Cellulitis. Families should be informed about signs of infection, such as increased swelling, redness, pain, fever, and malaise. It may be difficult to determine whether the symptoms are from the burn itself or from a superimposed infection. If a patient with a burn presents with concern for cellulitis, then they should receive broad-spectrum antibiotics that cover both gram-negative and gram-positive organisms.45 Cellulitis is an uncommon complication of burns, especially if they are adequately cleaned and dressed.45
Conclusion
Pediatric emergency departments and urgent care providers may encounter a variety of burn-related complaints that range from mild and able to be managed in the outpatient setting to severe and requiring transfer to a burn center. Providers should be prepared to initiate evaluation and management while appropriately triaging and referring to a burn center if necessary.
The initial encounter for a burn should be conducted as a trauma evaluation with primary, secondary, and tertiary surveys. Subsequent encounters should include re-assessment for the family’s capacity to adhere with necessary follow-up recommendations and evaluation of proper wound healing.
Given the prevalence of burns in the pediatric emergency department, the unique needs of the pediatric population, and the ever-evolving research in burn management, it is important for providers to be familiar with the current standard of care in managing pediatric burn injuries in the emergency setting.
References
- Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS). Last reviewed Nov. 8, 2023. https://www.cdc.gov/injury/wisqars/index.html
- Abramowicz S, Allareddy V, Lee MK, et al. Hospital-based emergency department visits with pediatric burns: Characteristics and outcomes. Pediatr Emerg Care 2020;36:393-396.
- American Burn Association. Scald Statistics and Data Resources. American Burn Association; 2018.
- West BA, Rudd RA, Sauber-Schatz EK, Ballesteros MF. Unintentional injury deaths in children and youth, 2010-2019. J Safety Res 2021;78:322-330.
- Tegtmeyer LC, Herrnstadt GR, Maier SL, et al. Retrospective analysis on thermal injuries in children—demographic, etiological and clinical data of German and Austrian pediatric hospitals 2006–2015—approaching the new German burn registry. Burns 2018;44:150-157.
- Yastı AÇ, Koç O, Şenel E, Kabalak AA. Hot milk burns in children: A crucial issue among 764 scaldings. Ulus Travma Acil Cerrahi Derg 2011;17:419-422.
- Tarim A, Nursal TZ, Basaran O, et al. Scalding in Turkish children: Comparison of burns caused by hot water and hot milk. Burns 2006;32:473-476.
- American Burn Association. Guidelines for burn patient referral. Published 2022. https://ameriburn.org/resources/burnreferral/
- Hundeshagen G, Wurzer P, Forbes A, et al. The occurrence of single and multiple organ dysfunction in pediatric electrical vs. other thermal burns. J Trauma Acute Care Surg 2017;82:946-951.
- Bailey B, Gaudreault P, Thivierge RL, Turgeon JP. Cardiac monitoring of children with household electrical injuries. Ann Emerg Med 1995;25:612-617.
- Williams FN, Lee JO. 40 - Chemical burns. In: Herndon DN, ed. Total Burn Care. 5th ed. Elsevier;408-413.e1.
- Nguyen ATM, Chamberlain K, Holland AJA. Paediatric chemical burns: A clinical review. Eur J Pediatr 2021;180:1359-1369.
- Sheridan RL. Burn care for children. Pediatr Rev 2018;39:273-286.
- Fuzaylov G, Fidkowski CW. Anesthetic considerations for major burn injury in pediatric patients. Pediatr Anesth 2009;19:202-211.
- Jeschke MG, van Baar ME, Choudhry MA, et al. Burn injury. Nat Rev Dis Primers 2020;6:11.
- Pham TN, Cancio LC, Gibran NS; American Burn Association. American Burn Association practice guidelines burn shock resuscitation. J Burn Care Res 2008;29:257-266.
- Venter M, Rode H, Sive A, Visser M. Enteral resuscitation and early enteral feeding in children with major burns—effect on McFarlane response to stress. Burns 2007;33:464-471.
- Sofia J, Ambardekar A. Pediatric burn resuscitation, management, and recovery for the pediatric anesthesiologist. Curr Opin Anaesthesiol 2020;33:360-367.
- Goverman J, Bittner EA, Friedstat JS, et al. Discrepancy in initial pediatric burn estimates and its impact on fluid resuscitation. J Burn Care Res 2015;36:574-579.
- Chan QE, Barzi F, Cheney L, et al. Burn size estimation in children: Still a problem. Emerg Med Australas 2012;24:181-186.
- U.S. Department of Health and Human Services. Lund and Browder chart. Published April 24, 2013. https://en.wikipedia.org/wiki/Lund_and_Browder_chart
- Rumpf RW, Steward WCL, Martinez SK, et al. Comparison of the Lund and Browder table to computed tomography scan three-dimensional surface area measurement for a pediatric cohort. J Surg Res 2018;221:275-284.
- Antrum JHG, Galloway JE, Anwar MU, Hodson SL. Managing a small burn. BMJ 2022;379:e068812.
- Church D, Elsayed S, Reid O, et al. Burn wound infections. Clin Microbiol Rev 2006;19:403-434.
- Roth JJ, Hughes W. The Essential Burn Unit Handbook. CRC Press; 2015.
- Thom D. Appraising current methods for preclinical calculation of burn size — a pre-hospital perspective. Burns 2017;43:127-136.
- Sheridan RL, Petras L, Basha G, et al. Planimetry study of the percent of body surface represented by the hand and palm: Sizing irregular burns is more accurately done with the palm. J Burn Care Rehabil 1995;16:605-606.
- Gonzalez R, Shanti CM. Overview of current pediatric burn care. Semin Pediatr Surg 2015;24:47-49.
- Romanowski KS, Palmieri TL. Pediatric burn resuscitation: Past, present, and future. Burns Trauma 2017;5:26.
- Shahi N, Skillman HE, Phillips R, et al. Why delay? Early enteral nutrition in pediatric burn patients improves outcomes. J Burn Care Res 2021;42:171-176.
- Warden GD. Burn shock resuscitation. World J Surg 1992;16:16-23.
- Centers for Disease Control and Prevention. Tetanus: For clinicians. Last reviewed Aug. 29, 2022. https://www.cdc.gov/tetanus/clinicians.html
- Peck MD, Priolo-Kapel D. Child abuse by burning: A review of the literature and an algorithm for medical investigations. J Trauma Acute Care Surg 2002;53:1013-1022.
- Dubowitz H, Lane WG. Abused and neglected children. In: Kliegman RM, Stanton BF, St. Geme JW 3rd, Schor NF, eds. Nelson's Textbook of Pediatrics. 20th ed. Elsevier;236-244.
- Purdue GF, Hunt JL, Prescott PR. Child abuse by burning—an index of suspicion. J Trauma 1998;28:221-224.
- Arbuthnot MK, Garcia AV. Early resuscitation and management of severe pediatric burns. Semin Pediatr Surg 2019;28:73-78.
- Strobel AM, Fey R. Emergency care of pediatric burns. Emerg Med Clin North Am 2018;36:441-458.
- Bakker A, Maertens KJP, Van Son MJM, Van Loey NEE. Psychological consequences of pediatric burns from a child and family perspective: A review of the empirical literature. Clin Psychol Rev 2013;33:361-371.
- Meyer WJ 3rd, Nichols RJ, Cortiella J, et al. Acetaminophen in the management of background pain in children post-burn. J Pain Symptom Manage 1997;13:50-55.
- Pardesi O, Fuzaylov G. Pain management in pediatric burn patients: Review of recent literature and future directions. J Burn Care Res 2017;38:335-347.
- Gandhi M, Thomson C, Lord D, Enoch S. Management of pain in children with burns. Int J Pediatr 2010;2010:e825657.
- Johnson SA, Shi J, Groner JI, et al. Inter-facility transfer of pediatric burn patients from U.S. emergency departments. Burns 2016;42:1413-1422.
- Sheridan R. Outpatient burn care in the emergency department. Pediatr Emerg Care 2005;21:449-456.
- Griffin BR, Frear C, Babl F, et al. Cool running water first aid decreases skin grafting requirements in pediatric burns: A cohort study of two thousand four hundred ninety-five children. Ann Emerg Med 2020;75:75-85.
- Lloyd ECO, Rodgers BC, Michener M, Williams MS. Outpatient burns: Prevention and care. Am Fam Physician 2012;85:25-32.
- Muangman P, Pundee C, Opasanon S, Muangman S. A prospective, randomized trial of silver containing hydrofiber dressing versus 1% silver sulfadiazine for the treatment of partial thickness burns. Int Wound J 2010;7:271-276.
- Gee Kee EL, Kimble RM, Cuttle L, et al. Randomized controlled trial of three burns dressings for partial thickness burns in children. Burns 2015;41:946-955.
