Managing the Difficult Airway in the Emergency Department
November 15, 2022
Related Articles
-
Infectious Disease Updates
-
Noninferiority of Seven vs. 14 Days of Antibiotic Therapy for Bloodstream Infections
-
Parvovirus and Increasing Danger in Pregnancy and Sickle Cell Disease
-
Oseltamivir for Adults Hospitalized with Influenza: Earlier Is Better
-
Usefulness of Pyuria to Diagnose UTI in Children
AUTHORS
Creagh Boulger, MD, FACEP, FAIUM, Professor, Associate Director of Ultrasound, AEMUS Fellowship Director, Ohio State University, Columbus
Samantha Lawson, MD, Ohio State University, Columbus
Matthew Barraza, MD, Ohio State University, Columbus
PEER REVIEWER
Frank LoVecchio, DO, FACEP, Vice-Chair for Research, Medical Director, Samaritan Regional Poison Control Center, Emergency Medicine Department, Maricopa Medical Center, Phoenix, AZ
EXECUTIVE SUMMARY
- Tools to predict the difficult airway have modest sensitivity but higher specificity, so always have a backup plan if your first approach is unsuccessful.
- Preoxygenation is important to prolong apneic oxygenation.
- Pre-intubation shock and hypoxia are associated with post-intubation cardiac arrest.
- Consider delayed sequence to enable stabilization of the agitated patient prior to paralytic administration.
- The emergency physician should be skilled in using either direct or video laryngoscopy since each has its advantages and disadvantages.
- Consider using the bougie when only a portion of the vocal cord opening can be visualized.
- Fiberoptic assisted intubation is used for intubation of angioedema and burn patients.
Introduction
Securing an airway is a vital skill for an emergency medicine provider. Endotracheal intubations often are high-risk and high-stress procedures, especially in the emergency department (ED) where prandial status, hemodynamics, and past history often are beyond the control of the provider. This paper will look to provide an updated review of airway management, specifically focusing on the difficult airway.
The authors will review various scoring systems for predicting difficult airways. In addition, the article will review various options for sedation and paralysis. A variety of techniques for approaching the difficult airway will be reviewed, such as awake and upright intubations, and less commonly used tools. Lastly, the article will discuss some situation-specific considerations, such as burns, trauma, and altered anatomy.
Case
A 50-year-old male presents to triage with a chief complaint of tongue swelling. His initial vital signs are blood pressure 180/100 mmHg, heart rate 105 beats/minute, SPO2 94%, and temperature 97.9°F. The patient states he was in his normal state of health until 30 minutes ago when he felt his tongue begin to swell. He tried diphenhydramine without any improvement. He denies any new food exposure. He denies any new medications. The only past medical history is hypertension, for which he is taking an angiotensin converting enzyme (ACE) inhibitor. He has been on the same medication for years. Given this presentation, what are you worried about? What should you consider when approaching this patient’s airway?
Anticipating a Difficult Airway
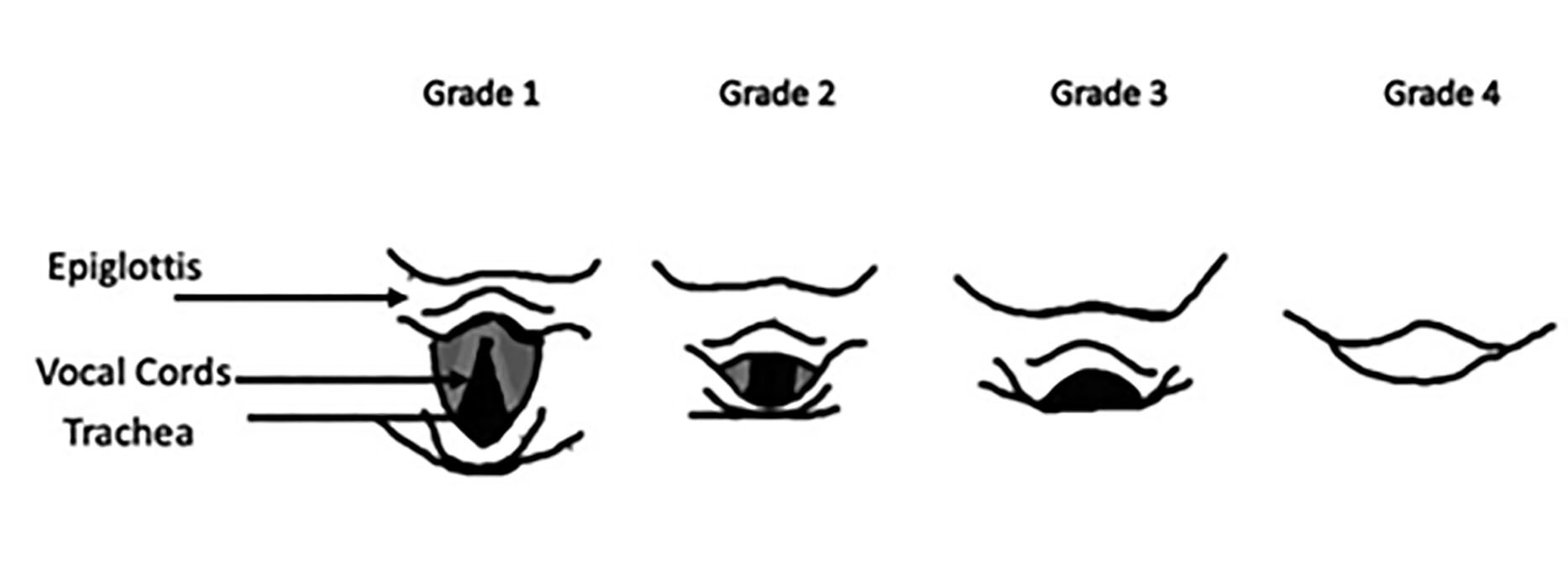
When a provider hears the words “difficult airway,” many visuals likely come to mind. Experienced emergency physicians can describe many scenarios where they expect the airway to be more challenging and thus approach the procedure of airway control with a modified algorithm. Most of the existing literature defines the difficult airway using the Cormack-Lehane grading scale, with grade 1 indicating full view to grade 4 indicating that the provider cannot see the epiglottis, cords, or trachea, or by a combination score that includes the Cormack-Lehane grading scale with the number of attempts to intubate called the Intubation Difficulty Scale. Figure 1 depicts the view available with each Cormack-Lehane grade.
Figure 1. Grade 1-4 Cormack-Lehane Views |
 |
A key question is how to make providers more accurate with recognition of a difficult airway. Many tools have been proposed to help providers predict potential difficult airways. Some of these tools will be discussed in the subsequent sections. The ability to predict a challenging intubation has the obvious benefits of better preparation and resource optimization.
About 10% of all emergency department airways will be considered difficult, and of those, up to 90% were unexpected, making it important that physicians responsible for airway management be familiar with multiple tools for evaluating a patient’s airway prior to intubation and be able to prepare the team with a plan to overcome these challenges.1,2 Some of these tools, such as the LEMON scoring tool (see Table 1), cervical neck mobility, incisor gap, thyromental and hyomental distances, and the upper lip bite test (ULBT), among others, may be familiar to most providers. None of the tools that have been developed to date have particularly high specificity, sensitivity, or positive predictive values.3-5
Table 1. LEMON and Wilson Scoring Systems |
||
LEMON Score |
Points |
|
L = Look, assess anatomy: Facial trauma, large incisors, facial hair, and large tongue |
Each gets a point |
|
E = Evaluate the 3-3-2 rule: Incisor distance (can they fit the breadth of three fingers in their open mouth), hyoid to mental distance (three finger breadths), and the thyroid to mouth distance (two finger breadths) |
Each measurement less than the ideal finger breadth gets 1 point |
|
M = Mallampati score > 3 |
1 point if greater than 3 |
|
O = Obstruction, such as emesis, soot, abscess, or trauma present? |
1 point if obstruction present |
|
N = Neck mobility, especially extension |
1 point if patient has restricted movement of their neck |
|
Wilson Score |
Points |
|
Weight |
< 90 kg – 0 points 90 kg to 100 kg – 1 point > 110 kg – 2 points |
|
Head and neck movement |
> 90 degrees – 0 points About 90 degrees – 1 point < 80 degrees – 2 points |
|
Jaw movement Interincisor gap (IG) or subluxation (SLux) |
IG > 5 cm or SLux > 0 – 0 points IG = 5 cm or SLux = 0 – 1 point IG < 5 cm or SLux < 0 – 2 points |
|
Receding mandible |
Normal – 0 points Moderate – 1 point Severe – 2 points |
|
Buck teeth |
Normal – 0 points Moderate – 1 point Severe – 2 points |
|
Interpretation |
LEMON Score |
Wilson Score |
Anticipate easy intubation |
0-2 points |
0-2 points |
Anticipate moderately difficult intubation |
3-4 points |
3-7 points |
Anticipate difficult intubation |
≥ 5 points |
≥ 8 points |
Increased LEMON score correlated with increased difficulty of intubation |
||
The initial evaluation of a patient’s airway begins with the basics of their physical exam — including habitus and facial anatomy — and ability to bag and preoxygenate.1 If time permits, review the patient’s history, probing for a history of neck surgeries and/or radiation or any other procedures that may alter the anatomy of the airway or oropharynx. Review of their medical record for past procedure notes from ED or operating room visits about prior intubations can be extremely helpful. The most predictive risk factor for a difficult intubation is a previously difficult one.1
One of the most effective tools for predicting a difficult airway is failure of a patient to be able to bite their upper lip covering their vermillion border.1,3 However, it is a test that still requires patient participation, which may not be possible in an emergency setting. Table 1 depicts the components of the LEMON evaluation as well as the Wilson scoring system. The LEMON score has been validated in the ED setting, but the Wilson score has only been validated in the perioperative environment.6,7 An increased LEMON or Wilson score correlates with increased difficulty of intubation.8
The limitation of the LEMON airway assessment in the ED is the need for patient cooperation to access the interincisor distance and the Mallampati component. The decompensating patient with a compromised airway often does not afford the time or capacity to perform these assessments. This leads to inaccuracies in evaluation.9 As seen in Detsky’s review article, the highest performing exam was part of the 3-3-2 rule, the hyomental distance, which had a sensitivity of 69%.1
The Wilson score considers the patient’s weight (greater or less than 90 kg), jaw mobility (interincisor gap greater or less than 5 cm), cervical spinal mobility (greater than, equal to, or less than 90 degrees), ability to protrude lower teeth past upper teeth, presence of retrognathia (normal, moderate, severe), and presence of large incisors (normal, moderate, severe).1 This scoring system is faster and requires less patient participation, which makes it a more feasible tool in the ED. It accounts for a variety of factors associated with more challenging airways, such as habitus, impaired jaw and neck mobility, and challenging maxillofacial anatomy. A Wilson score of 2-3 or greater has low sensitivity but high specificity of 95% and a positive likelihood ratio of 9.1.1
These various studies demonstrate that the emergency medicine provider has a limited ability to objectively predict when an airway will be difficult.4 Although none of these tools stand well by themselves, they still may aid in preparation and decision making. A multimodal approach considering habitus, past medical and surgical history, physical exam, and the etiology of airway failure is necessary to best prepare for a difficult airway.
Preoxygenation
Prior to delving into the various approaches to intubation, it is important to discuss preoxygenation and preparation. A 2017 study defines the purpose of preoxygenation as: maintaining hemoglobin saturation despite ongoing oxygen consumption during apnea. This is accomplished by denitrogenation of the alveoli so the functional residual capacity can serve as a reservoir of oxygen. Regardless of the intubation approach, maximizing the preoxygenation of the patient will be beneficial.10
To optimize preoxygenation, a provider should place the patient on a non-rebreather (NRB) at 15 L per minute. There also should be a nasal cannula placed on the patient with the flow turned up to 15 L per minute or higher. When the provider attempts intubation, the nasal cannula should be left on for apneic oxygenation. This postpones the time before desaturation. Apneic oxygenation was associated with increased peri-intubation oxygen saturation, lower rates of hypoxemia, and increased first-pass intubation success.10-12 Unsurprisingly, patients who are not able to be oxygenated well prior to intubation have a higher risk of cardiac arrest.13,14
Rapid Sequence Intubation
Currently, rapid sequence intubation (RSI) is the standard of care for endotracheal intubations in the ED. Compared with non-rapid sequence intubation, RSI has been shown to be safer for patients and to improve intubation success rates. A large, prospective study in 2017 following 2,365 ED patients in Japan, where RSI is not as widely used, found that RSI compared to non-RSI had a higher first- and second-pass success without having increased complication rates.15
Similar to poorly preoxygenated patients, those who are not volume resuscitated prior to intubation attempts also have higher arrest rates.14 The choice of RSI medications in the hypotensive patient can be challenging. Recent literature shows that the shock index can be helpful as a predictor of post-intubation hypotension and cardiac arrest.16,17 The shock index is defined as heart rate (HR)/systolic blood pressure (SBP), with a normal range of 0.5-0.7. An index ≥ 0.8 can be a clue to a hypoperfusing state, and post-intubation cardiac arrest (PICA) rates are higher in patients with a shock index ≥ 0.8.16,17
To address elevated shock index, the provider should identify the patient’s specific etiology of hypotension. For example, in trauma patients with an elevated shock index, blood products should be given, and hemorrhage control should be attempted. In septic patients with an elevated shock index, the provider should give judicious fluids and consider early vasopressors. More studies still are needed to evaluate the optimal timing and degree of pretreatment for shock before intubation. The prePARE trial aimed to look at this with 500 cc boluses of intravenous isotonic fluids but was stopped early due to futility.18
Delayed Sequence Intubation
Delayed sequence intubation (DSI) is another approach to intubation that can be considered in the difficult airway. This is defined as having a separation between the timing of giving the induction agent and giving the paralytic. This approach is useful when the provider is unable to adequately preoxygenate the patient prior to intubation. An example would be a delirious hypoxemic patient who is too altered to keep the non-invasive positive pressure ventilation (NIPPV) on to preoxygenate prior to intubation. This approach will allow the physician to medicate the patient and provide anxiolysis, position them optimally for intubation, optimize their hemodynamics and oxygenation, and then push the paralytic and complete endotracheal intubation.
Rapid Sequence Intubation Medications
While there is no one combination of paralytic and induction agent that is consistently better than another, there are some situations where specific medication combinations may be more optimal for the patient. For example, a patient with severe bronchospasm or hypotension may benefit more from induction with ketamine rather than etomidate secondary to ketamine’s bronchodilation and hemodynamic neutrality. Tables 2 and 3 summarize the more commonly used medications and their properties.19
Table 2. Induction Agents for Intubation |
||||||
Agent |
Dosage |
Onset (seconds) |
Duration (minutes) |
Contraindications |
Side Effects |
Note |
Ketamine |
IV push |
< 60 |
5-10 |
Relative contraindication: History of psychosis |
|
|
Etomidate |
IV 0.3 mg/kg |
30-60 |
10-15 |
Adrenal crisis |
|
|
Propofol |
1 mg/kg to |
15-30 |
5-10 |
|
||
Midazolam (second line) |
0.2 mg/kg to 0.3 mg/kg |
60-180 |
30-120 |
|
||
Fentanyl (second line) |
0.5 mcg/kg to 1 mcg/kg |
30 |
30-60 |
|
|
|
IV: intravenous |
||||||
Table 3. Paralytic Agents for Intubation |
|||||||
Agent |
Dosage |
Onset (seconds) |
Duration (minutes) |
Contraindications |
Relative Contraindications |
Side Effects |
Note |
Succinylcholine |
1 mg/kg to |
30-60 |
5-10 |
Burns > 48 hours ago |
Bradycardia |
Can raise K by 0.5-1 |
Caution with neuro-muscular disease |
Rocuronium |
0.6 mg/kg to |
45-90 |
20-45 |
Slower onset of action and metabolism in liver disease |
|||
Vecuronium |
0.1 mg/kg |
120-180 |
45-65 |
||||
K: potassium |
|||||||
Awake Intubation
When a difficult airway is anticipated but the patient is oxygenating and ventilating adequately at the time on their own, the provider may want to consider an awake intubation. A review in 2016 showed that in 1,085 awake intubations, there was a high success rate, with a failure rate of 1% and complication rate of 1.6%.21-23 Awake intubations can be considered in patients who are compliant, who have a low risk of emesis, and who have a window of stability in regard to oxygenation and ventilation.
Direct, fiberoptic, or video laryngoscopy all can be used in awake intubation. There are some unique aspects of awake intubation. Mild sedation or anxiolysis may be necessary. The provider also should consider topical anesthesia, typically by means of nebulized or topical lidocaine for the airway. Finally, glycopyrrolate or other anticholinergics should be considered to reduce secretion, improve patient comfort, and reduce complications.
Tools for the Difficult Airway
The tools of intubation have advanced significantly over the years. Video laryngoscopy (VL) has become a more prominent approach in the past decade. However, direct laryngoscopy (DL) still is an important skill for providers to be facile with. This is important because there are situations where the VL camera is likely to be obscured, such as the bloody or emesis-filled airways, that may require DL skills to secure the airway appropriately. In two large reviews, DL and VL both were shown have their strengths.
Accurate comparisons between VL with DL have limitations since it is challenging to perform large, randomized studies with difficult airways. In addition, several studies mention that they were done only with experienced providers, which makes extrapolation to the broad range of providers difficult. The decision to use DL or VL should be made based on the provider’s comfort with the technique, taking into account patient characteristics. Neither approach has been shown to be consistently faster or safer than the other, making both vital skills for the emergency provider.24,25
A lower technology airway tool that has reemerged in the literature is the bougie. A recent study showed that in a grade IIb Mallampati view or worse, bougie use was associated with higher first-pass success rates.26 The rationale for use of this adjunct is that it adds tactile feedback from the bougie passing along the trachea when visual feedback is limited or not present.
In addition, more advanced adjuncts, such as flexible bronchoscopes, are becoming less expensive and more widely available. Their use as an airway adjunct can be incredibly helpful in situations where anatomy is distorted or prior to an attempt to better plan for a challenging intubation. Angioedema is one such situation where the bronchoscope-facilitated intubation may be useful. Importantly, a tube should be loaded onto the bronchoscope prior to obtaining a view, as shown in Figure 2. This allows for intubation as soon as visualization is obtained without the need for a second attempt.
Figure 2. Endotracheal Tube Loaded on Fiberoptic Scope |
 |
Often patients with difficult airways have had attempts by other providers prior to the emergency provider. Frequently, if attempts at endotracheal intubation are unsuccessful in the field, a King LT or Combitube may be placed as a temporary airway. These do not secure the airway and should be exchanged for a definitive, secured airway as soon as safely possible.27 While these devices can be left in place for up to 36 hours, as documented in literature, they ideally should be exchanged as early as possible since they promote increased trauma to the airway and surrounding tissue and not all are compatible with mechanical ventilation.28 This exchange can be done using a bougie or Cook catheter. If the airway is more tenuous, a flexible bronchoscope can be used to confirm passage into the trachea prior to exchange.
Special Airway Situations
There are certain patient populations that frequently present with difficult airways as a complication of their underlying pathology. A few commonly encountered presentations that will be discussed include patients with angioedema, trauma to the face or neck, contaminated airway (with blood or vomitus), mass or malignancy, and burns.
Angioedema
Angioedema is localized submucosal and mucosal non-pitting edema that often involves the soft tissue of the upper airway and may require intubation. About 7% of patients who present with angioedema will need intubation.29 Patients requiring intubation may present with swelling, voice change, hoarseness, dyspnea, and stridor.29-31
In a 2018 large cohort study of more than 19,000 angioedema patients, physicians secured an airway on first pass 81% of the time, with emergency medicine physicians performing 94% of these intubations.29 In this study, fiberoptic intubation or flexible endoscope was used 49% of the time. It is recommended that fiberoptic tools be used in this patient population because of the peri-intubation swelling and further distortion of the airway after a failed first pass. Video laryngoscopy was used in the other portion of intubations, with geometric and hyperangulated blades 22% and 19% of the time, respectively, with a 79% success rate.29
This study found that RSI was used most often and did not impede first-pass success, although the authors recommended awake intubations if clinicians were comfortable with it since it had slightly higher success rates. Other studies also have endorsed that fiberoptic intubation and assessment of the upper airway are beneficial in patients with angioedema.32 Cricothyrotomy should always be considered and readily available when attempting an intubation on a patient with angioedema.30
A grading system was proposed by Ishoo et al for determining airway risk and proposed dispostion based on clinical presentation.31 This system is described in Table 4. In this study, 7% of stage 3 patients and 24% of stage 4 patients were intubated.31 Tools like this can help reinforce which physical exam findings are most associated with a compromised airway and can guide the threshold for the need to secure a definitive airway in this population.
Table 4. Ishoo Classification for Monitoring Upper Airway |
||
Stage |
Clinical Findings |
Disposition |
1 |
Facial rash, facial edema, lip edema |
Home or admission |
2 |
Soft palate edema |
Home or admission |
3 |
Lingual edema |
Intensive care unit |
4 |
Laryngeal edema |
Intensive care unit |
Face or Neck Trauma
Blood and emesis are commonly encountered adversities when tackling any airway. In addition to these, trauma patients often have the added hurdle of maintaining cervical spine precautions.33-35 Although cervical spine injuries occur in only 2% of trauma patients, maintaining immobilization throughout intubation in trauma is the number one cause of a difficult airway.34
Direct laryngoscopy can be difficult while maintaining spinal precautions, but providers should be wary of video laryngoscopy as well. Video laryngoscopy can be limited by the presence of blood, emesis, and the angle of the blade. Optimize proper manual in-line stabilization with the collar open (front of collar off) and have an “earmuff” position of the hands so that the mandible is not restricted.33,34
Fractures to the face can cause disruption of the tongue insertion site, swelling, and displacement of teeth and soft tissue, thus complicating any airway procedure. Additionally, direct laryngeal/tracheal trauma can affect the ability to easily place an endotracheal tube. Cricoid pressure is not recommended in these patients, since it can distort the anatomy even more and has not been shown to prevent contamination of the airway.36 Direct, video, and surgical airways all have their place in this setting and should be part of the provider’s algorithm.
Burns
Patients with inhalation injuries and facial burns can create an airway challenge even for seasoned emergency physicians. Traditional practice with inhalation injury is to have a low threshold to intubate, especially with soot in the nares and mouth. The rationale behind early intubation in these patients is that there is risk for delayed laryngeal and tracheal edema leading to respiratory distress hours after the insult. Recent evidence in a large study series found that a low threshold for early intubation is unnecessary since 33% of burn patients were extubated within one day of intubation.37 It is possible that we should be more discerning about which burn patients need intubations and how best to manage the procedure.
No consensus exists about grading the extent of these injuries, and physical exam findings can mislead clinicians. For example, 70% of facial burn patients do not have significant pulmonary injury.37 History, what was burning, whether the patient was inside or outside, toxin exposure, explosion, physical exam, objective data, and mental status all should be used to determine the need for intubation.37 Steam, enclosed space, hoarseness, inability to swallow secretions, cough, and stridor are the strongest indicators of upper airway impairment.38
Airway burns can be divided into supraglottic and subglottic injuries. Supraglottic injuries will be identified on initial inspection evaluating for erythema or edema in the oropharynx, soot in the nose or mouth, and burns to the face and upper airway. Supraglottic injury can be diagnosed with direct visualization with laryngoscopy or a fiberoptic scope.
Subglottic injuries also can be evaluated via bronchoscopy. While very effective, it is not always readily available or comfortably used by emergency medicine physicians. Inhalational injuries are likely to be worse at the proximal airway, thus evaluation of more distal injuries often is not necessary in the emergent setting. If there is concern for distal airway injury, as evident by V/Q mismatch, this can be investigated in a subacute manner.37
When intubation is deemed necessary in patients with thermal airway injuries, awake intubation may be the safest approach.33,34 When this is not possible, management can be done with video laryngoscopy with preparation of the neck for a potential surgical airway if endotracheal intubation is unsuccessful.
Contaminated Airway
An airway can be contaminated from emesis, blood, secretions, or any object in the airway that can obstruct a clinician’s view. Contamination of the airway reduces first-pass attempts at intubation regardless of intubation method.33,34 Suction always should be at the ready when intubating; when a contaminated airway is expected, a secondary suction should be set up prior to any intubation attempts. The reason this preparation is so important is that aspiration is one of the leading causes of mortality in tracheal intubations.39 In addition to death, aspiration increases the risk of hypoxemia and hypotension, adding further insults to an already critically ill patient.40
A technique referred to as Suction Assisted Laryngoscopy and Airway Decontamination (SALAD) involves intentionally placing one suction catheter into the esophagus and using the other to continually clear the airway when using the laryngoscope. In this manner, one can more easily lift the epiglottis out of the contaminant.34
Although classic teaching is to use direct laryngoscopy in an airway contaminated by blood, studies have shown that video laryngoscopy had more success: 78% with video laryngoscopy vs. 62% with direct laryngoscopy.41 The debate between direct and video laryngoscopy has been studied mostly in simulation patients. Devices that can be used as direct if the camera becomes soiled are thought to be a logical compromise.34 Other tools to consider in a challenging and contaminated airway include using cricoid pressure, avoiding excessive positive pressure ventilation, and quickly moving to a surgical airway if a definitive airway cannot be secured in a timely fashion.34,42
Mass or Malignancy
In patients with known head and neck cancer, preparing for a difficult airway is the key to success. These patients may have challenges relating to radiation, surgery, or mass. Being aware of these situations can guide clinical decisions and best prepare for successful intubation. In these cases, acting early can be of great benefit to the patient. Signs and symptoms of impending airway collapse can include increased work of breathing, tripoding, stridor, drooling, and/or diaphoresis.
When available, review previous imaging and prior airway attempts to better anticipate the level at which airway obstruction is occurring or may be occurring. When intubation is necessary, awake, fiberoptic, and upright intubations are the most effective.43-45
Mass occupying lesions collapse the airway when in supine position, making ventilation and passing an endotracheal tube (ETT) difficult. Knowing this, providers should strongly consider upright intubation in patients with known or suspected oropharyngeal masses. Another hurdle to intubation in these patients is scar tissue. Strictures from radiation and surgical intervention, as well as masses, often make the airway much narrower than anticipated.43 Choosing a small ETT and having smaller tubes available is recommended (5.5 mm to 6.5 mm).
With impending upper airway obstruction, surgical airway may be required. Cricothyrotomy equipment should be immediately available. When available, the provider should seek out backup from other specialized airway physicians, such as otolaryngology, anesthesia, and surgery. These patients also are more likely to have a contaminated airway than the general population.43,44
In addition to the mechanical obstruction, head and neck cancers often are highly vascularized. Providers should anticipate bleeding and be prepared with suction and treatments such as nebulized epinephrine or tranexamic acid. The risk of significant bleeding increases with each subsequent attempt secondary to trauma to the soft tissue.
Mohamebhai et al have proposed a scoring system to aid providers in their airway assessment for patients with head and neck cancer.44 While this was an anesthesiology study, the researchers aimed to create a score to evaluate who was safe for primary intubation and which patient was best served with a primary tracheostomy. This scoring system is a bit more complex, but given the fact that many of these patients will present to the ED with respiratory complaints, this system could be of use to ED providers when approaching this patient population. In this single-center study, they found that patients with a score of 4 or less were safe for primary intubation, with a sensitivity and specificity around 90%.44 The components of the score are described in Table 5. While this is only a single site, it summarizes many of the historical factors to consider when approaching the airway in this challenging patient population.
Table 5. Components of the TRACHY Score43 |
|||||
T: Tumor Staging |
R: Reconstruction |
A: Anatomy |
C: Coexisting Conditions |
H: History |
Y: Laterality |
T1 = 0 |
Fasciocutaneous = 0 |
Lateral = 0 |
ASA 1 & 2 = 0 |
None = 0 |
Unilateral = 0 |
T2 = 0 |
Myocutaneous = 1 |
Central = 0 |
ASA 3 = 1 |
Operation = 1 |
Bilateral = 3 |
T3 = 1 |
Composite = 1 |
Anterior = 2 |
Radiotherapy = 3 |
||
T4 = 1 |
Two flap = 3 |
Oropharyngeal = 2 |
|||
Assessment: Score ≥ 4 points – tracheostomy indicated; score < 4 – manage with endotracheal tube ASA = American Society of Anesthesiologists |
|||||
Surgical Airway
When other methods have failed, the trauma or burns are too severe, the oropharyngeal swelling is not controlled, or the patient is deteriorating and unable to oxygenate and ventilate, it is crucial to make the decision to move to a surgical airway. This can be a difficult call to make. Surgical airways are low-frequency, high-risk situations that only occur in 0.05% to 1.7% of ED intubations.34
As discussed throughout this article, there should be preparation and consideration of a surgical airway long before it is necessary to perform one. Having this as a planned step in securing the airway, knowing when you will move to it, and communicating this to the care team are of utmost importance. Discussing your airway algorithm, including surgical airway, with your team every time an airway procedure is performed will help normalize a rarely performed procedure and reduce the hesitation to perform a surgical airway when needed.
Once the decision is made to proceed with surgical airway, the next step is to identify the cricothyroid membrane (CTM). If time allows, this should be performed prior to intubation attempts to reduce the mental load on the performing provider. Certain patient populations, most notably women and obese patients, have predictably more difficult landmarks. In these patients, visualization of the CTM only works 50% of the time.46 Palpation is a highly important skill in these patients, especially when visualization is not available. Physicians should use their non-dominant hand, palpating the cricoid cartilage on either side with the thumb and middle finger and sliding the hand caudally until the CTM is felt with the first finger.
When preparing for a surgical airway, the provider may use a commercial kit. If this is not available, a surgical airway can be achieved with as little as a scalpel, bougie, and endotracheal tube. Evidence suggests that the scalpel-bougie-tube technique has the highest first-attempt success rate.34,46 The most important thing is that the physician knows how to use the tools at their disposal. Given that this is a rarely performed, high-acuity procedure, simulation practice is paramount.
Summary
Airway management is an essential skill to the practicing emergency physician. We are experts in airways and should be aware of and comfortable with all the tools and methods at our disposal. This review has focused on the most recent advances in airway management. Always preoxygenate. The provider should pay attention to the shock index and resuscitate accordingly prior to intubation when feasible. In patients with angioedema, use scoring systems to aid in disposition. In patients with head and neck malignancy, gather as much information as possible about their malignancy and treatments to aid in decision making about the means of airway control.
Most importantly, make sure you have a multi-level algorithm that you employ when approaching an airway. This algorithm can include DL, VL, fiberoptics, supraglottic airways, airway adjuncts like the bougie, and finally the surgical airway. Finally, it is crucial to recall that not all airways are created equal. Optimize your medications, tools, and positioning for the patient and scenario in front of you to achieve the `highest first-past success rates. One of the most valuable tools for tackling a complicated airway is practice.47,48
Case Conclusion
In this patient, the provider should consider angioedema or anaphylaxis high on their differential. Given these diagnoses and the patient’s presentation, the provider should have a high suspicion for oropharyngeal edema and should anticipate a challenging airway. This patient currently is oxygenating and ventilating well. The provider could administer appropriate medical treatments while closely monitoring. They also could consider an awake look with DL, VL, or fiberoptic to assess the amount of edema. If the patient does not promptly respond to medical treatment, the provider should consider securing the airway. In this patient, an awake upright intubation would be ideal to avoid increasing the edema when placing the patient in a supine position and allowing the patient to continue to maintain their oxygenation and ventilation during the procedure. Prior to an airway attempt, the provider should evaluate the anterior neck and mark the midline and CTM.
REFERENCES
- Detsky ME, Jivraj N, Adhikari NK, et al. Will this patient be difficult to intubate? The rational clinical examination systematic review. JAMA 2019;321:493-503.
- Kollmeier BR, Boyette LC, Beecham GB, et al. Difficult airway. StatPearls 2022. https://www.ncbi.nlm.nih.gov/books/NBK470224/
- Faramarzi E, Soleimanpour H, Khan ZH, et al. Upper lip bite test for prediction of difficult airway: A systematic review. Pak J Med Sci 2018;34:1019-1023.
- Yentis SM. Predicting difficult intubation--worthwhile exercise or pointless ritual? Anaesthesia 2002;57:105-109.
- Vannucci A, Cavallone LF. Bedside predictors of difficult intubation: A systematic review. Minerva Anestesiologica 2015;82:69-83.
- Hagiwara Y, Watase H, Okamoto H, et al. Prospective validation of the modified LEMON criteria to predict difficult intubation in the ED. Am J Emerg Med 2015;33:1492-1496.
- Soyuncu S, Eken C, Cete Y, et al. Determination of difficult intubation in the ED. Am J Emerg Med 2009;27:905-910.
- Reed MJ, Dunn MJG, McKeown DW. Can an airway assessment score predict difficulty at intubation in the emergency department? Emerg Med J 2005;22:99-102.
- Reed MJ, Rennie LM, Dunn MJG, et al. Is the ‘LEMON’ method an easily applied emergency airway assessment tool? Eur J Emerg Med 2004;11:154-157.
- Pourmand A, Robinson C, Dorwart K, O’Connell F. Pre-oxygenation: Implications in emergency airway management. Am J Emerg Med 2017;35:1177-1183.
- Silva LOJE, Cabrera D, Barrionuevo P, et al. Effectiveness of apneic oxygenation during intubation: A systematic review and meta-analysis. Ann Emerg Med 2017;70:483-494.e11.
- Mosier JM, Hypes CD, Sakles JC. Understanding preoxygenation and apneic oxygenation during intubation in the critically ill. Intensive Care Med 2017;43:226-228.
- April MD, Arana A, Reynolds JC, et al. Peri-intubation cardiac arrest in the emergency department: A National Emergency Airway Registry (NEAR) study. Resuscitation 2021;162:403-411.
- De Jong A, Rolle A, Molinari N, et al. Cardiac arrest and mortality related to intubation procedure in critically ill adult patients: A multicenter cohort study. Crit Care Med 2018;46:532-539.
- Okubo M, Gibo K, Hagiwara Y, et al; Japanese Emergency Medicine Network Investigators. The effectiveness of rapid sequence intubation (RSI) versus non-RSI in emergency department: An analysis of multicenter prospective observational study. Int J Emerg Med 2017;10:1.
- Althunayyan SM. Shock index as a predictor of post-intubation hypotension and cardiac arrest; A review of the current evidence. Bull Emerg Trauma 2019;7:21-27.
- Zhang X, Wang Z, Wang Z, et al. The prognostic value of shock index for the outcomes of acute myocardial infarction patients. Medicine (Baltimore) 2017;96:e8014.
- Janz DR, Casey JD, Semler MW, et al. Effect of a fluid bolus on cardiovascular collapse among critically ill adults undergoing tracheal intubation (PrePARE): A randomised controlled trial. Lancet Respir Med 2019;7:1038-1047.
- Groth CM, Acquisto NM, Khadem T. Current practices and safety of medication use during rapid sequence intubation. J Crit Care 2018;45:65-70.
- Shi HJ, Yuan RX, Zhang JZ, et al. Effect of midazolam on delirium in critically ill patients: A propensity score analysis. J Int Med Res 2022;50:1-10.
- Joseph TT, Gal JS, DeMaria S, et al. A retrospective study of success, failure, and time needed to perform awake intubation. Anesthesiology 2016;125:105-114.
- Leslie D, Stacey M. Awake intubation. Continuing Education in Anaesthesia, Critical Care & Pain 2015;15:64-67.
- Leslie D, Stacey M. Awake intubation Continuing Education in Anaesthesia, Critical Care & Pain 2015;15:64-67.
- Griesdale DEG, Liu D, McKinney J, Choi PT. Glidescope® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: A systematic review and meta-analysis. Canadian Journal of Anesthesia 2012;59:41-52.
- De Jong A, Molinari N, Conseil M, et al. Video laryngoscopy versus direct laryngoscopy for orotracheal intubation in the intensive care unit: A systematic review and meta-analysis. Intensive Care Med 2014;40:629-639.
- Driver B, Dodd K, Klein LR, et al. The bougie and first-pass success in the emergency department. Ann Emerg Med 2017;70:473-478.
- Subramanian A, Garcia-Marcinkiewwicz AG, Brown DR, et al. Definitive airway management of patients presenting with a pre-hospital inserted King LT(S)-DTM laryngeal tube airway: A historical cohort study. Canadian Journal of Anesthesia 2016;63:275-282.
- Mort TC. The role of the LMA as a ventilating and intubation conduit during emergency airway management: Utilization, success rates and trends. Anesthesiology News Sept. 3, 2019.
- Sandefur BJ, Liu XW, Kaji AH, et al. Emergency department intubations in patients with angioedema: A report from the National Emergency Airway Registry. J Emerg Med 2021;61:481-488.
- Long BJ, Koyfman A, Gottlieb M. Evaluation and management of angioedema in the emergency department. West J Emerg Med 2019;20:587-600.
- Ishoo E, Shah UK, Grillone GA, et al. Predicting airway risk in angioedema: Staging system based on presentation. Otolaryngol Head Neck Surg 1999;121:263-268.
- Pandian V, Zhen G, Stanley S, et al. Management of difficult airway among patients with oropharyngeal angioedema. Laryngoscope 2018;129:1360-1367.
- Walrath BD, Harper S, Barnard E, et al. Airway management for trauma patients. Mil Med 2018;183(Suppl 2):29-31.
- Kovacs G, Sowers N. Airway management in trauma. Emerg Med Clin North Am 2018;36:61-84.
- Li T, Jafari D, Meyer C, et al. Video laryngoscopy is associated with improved first‐pass intubation success compared with direct laryngoscopy in emergency department trauma patients. J Am Coll Emerg Physicians Open 2021;2:1-9.
- Choi J, Lorenz PH, Spain DA. Review of facial trauma management. J Trauma Acute Care Surg 2020;88:e124-e130.
- Foncerrada G, Culnan DM, Capek KD, et al. Inhalation injury in the burned patient. Ann Plast Surg 2018;80(3Suppl2):S98-S105.
- Gigengack RK, Cleffken BI, Loer SA. Advances in airway management and mechanical ventilation in inhalation injury. Curr Opin Anesthesiol 2020;33:774-780.
- Cook TM, Woodall N, Frerk C; Fourth National Audit Project. Major complications of airway management in the UK: Results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: Anaesthesia. Br J Anaesth 2011;106:617-631.
- Sakles JC, Chiu S, Mosier J, et al. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med 2013;20:71-78.
- Corn GJ, Hollinger P, Patanwala AE, Sackles JC. The use of a GlideScope video laryngoscope is associated with a higher first pass success than a direct laryngoscope in the presence of a bloody airway. Ann Emerg Med 2015;66:S5.
- Salem MR, Khorsani A, Zeidan A, Crystal GJ. Cricoid pressure controversies: Narrative review. Anesthesiology 2017;126:738-752.
- Chen K, Varon J, Wenker OC. Malignant airway obstruction: Recognition and management. J Emerg Med 1998;16:83-92.
- Mohamedbhai H, Ali S, Dimasi I, Kalavrezos N. TRACHY score: A simple and effective guide to management of the airway in head and neck cancer. Br J Oral Maxillofac Surg 2018;56:709-714.
- Wong J, Lee JSE, Wong TGL, et al. Fibreoptic intubation in airway management: A review article. Singapore Med J 2019;60:110-118.
- Price TM, McCoy EP. Emergency front of neck access in airway management. BJA Educ 2019;19:246-253.
- Amalric M, Larcher R, Brunot V, et al. Impact of videolaryngoscopy expertise on first-attempt intubation success in critically ill patients. Crit Care Med 2020;48:e889-e896.
- Singhal SK, Kaur K, Yadav P. A study to evaluate the role of experience in acquisition of the skill of orotracheal intubation in adults. J Anaesthesiol Clin Pharmacol 2021;37:469.
Securing an airway is a vital skill for an emergency medicine provider. The authors will review various scoring systems for predicting difficult airways, as well as a variety of techniques for approaching the difficult airway.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
