AUTHORS
Christian Bergman, MD,
Whitney Briggs, DO,
Austin Cottam, MD,
Michelle Lee, MD,
Marianna Oppenheimer-Velez, MD,
Emir Udovcic, MD,
Emergency Medicine Residents, The Ohio State University Wexner Medical Center, Columbus;
Andrew Grozenski, MD, CAQSM, Assistant Professor of Emergency Medicine and Sports Medicine, The Ohio State University Wexner Medical Center, Columbus
PEER REVIEWER
Brian L. Springer, MD, FACEP, Professor, Vice Chair, Director, Division of Tactical Emergency Medicine, Wright State University Department of Emergency Medicine, Dayton, OH
EXECUTIVE SUMMARY
- Crush injuries and other high mechanism trauma are most commonly associated with compartment syndrome. However, any time vascular damage, prolonged immobilization, or penetrating trauma is present, providers should maintain a high index of suspicion for compartment syndrome, which is key for early diagnosis and intervention. Normal compartment pressure is less than 10 mmHg. If the compartment pressure reaches 30 mmHg or greater, it is considered diagnostic for acute compartment syndrome.
- Sternoclavicular joint (SCJ) dislocations are uncommon because of the strong ligamentous support of the joint. They commonly occur as a result of motor vehicle collisions (MVCs) or collision sports, such as ice hockey or football. If present, there should be a high index of suspicion for other associated traumatic injuries. In a suspected or radiograph-confirmed SCJ dislocation, computed tomography scan is the imaging of choice, since this allows visualization of mediastinal structures and potential co-occurring injuries. Posterior dislocations can result in injury to the trachea, esophagus, brachial plexus, or great vessels in up to one-third of cases.
- The neurovascular status of the affected lower extremity with a potential distal femur should be assessed thoroughly. If weak pulses are found, further assessment for possible arterial injury should be done using a Doppler probe and obtaining ankle brachial index (ABI). An ABI < 0.9 or obvious signs of vascular injury would necessitate obtaining angiography.
- Initial assessment of acute knee dislocation should involve thorough skin assessment and neurovascular examination. In 5% to 17% of cases, the injury is reported as open. The proximity of the popliteal artery makes vascular injury a concern, with recent literature suggesting a 7.5% to 14% incidence of vascular lesions. Emergent surgical intervention is required in the presence of obvious vascular injury causing acute limb ischemia.
Major orthopedic trauma is a common issue for the emergency medicine provider. Being able to make a timely diagnosis and optimize care improves patient outcomes.
— Ann M. Dietrich, MD, Editor
Introduction
From 2013 to 2014, there were 7,214,915 patients who sustained an orthopedic injury. Of these, 1,167,656 required surgical procedures.1 One meta-analysis looking at the socioeconomic impact of orthopedic trauma showed that on average one-third of patients had not returned to work one year after their injury, patients had missed nearly 100 days of work, and roughly 13% of patients had lost employment as a result of their injuries.2 Therefore, it is incumbent on those caring for patients with major orthopedic trauma to understand the impact these injuries have on patients and optimize care for the best outcome possible.
This article starts with an overview of general orthopedic principles so that the reader understands how to describe fractures using proper nomenclature, how to approach an orthopedic physical exam and diagnostic imaging, and how to evaluate orthopedic injuries during a trauma resuscitation.
General Orthopedic Principles
Fracture Nomenclature
Understanding the descriptors and nomenclature surrounding orthopedic fractures allows for a common language to be spoken among providers.
Bones can be divided into four categories based on appearance: long, short, flat, and irregular. Long bones provide support and facilitate movement (i.e., femur, humerus, tibia, radius), short bones likewise provide support while also facilitating motion (i.e., cuboid, navicular, scaphoid), flat bones often are attachment anchors for muscle and can provide internal organ protection (i.e., scapula, sternum, cranial bones), and irregular bones often serve specialized functions for movement and protection (i.e., vertebrae, facial bones). Fracture location is described by using terms such as proximal, distal, lateral, and medial to indicate the fracture’s position on the bone.
Complete bone fractures occur when a fracture separates bone into at least two pieces going through two cortical surfaces. Complete bone fractures are divided into transverse fractures (the fracture line that goes straight across the bone), oblique fractures (an oblique fracture line separates the bone), spiral fractures (the fracture corkscrews through the bone), and comminuted fractures (the fracture separates the bone into more than two parts). Conversely, incomplete fractures involve a single cortical surface without extension through the bone. Typically, adults are more likely to sustain complete fractures, whereas pediatric patients have more incomplete fractures because of increased malleability of bones at younger ages. Examples of incomplete fractures are a torus/buckle fracture (a compression fracture with bulging of the bone’s cortex), bowing fracture (the bone bends, although cortices remain intact), and greenstick fractures (a single cortex fractures while the other side bends). Complete fractures are inherently less stable than incomplete fractures and more commonly require surgical intervention for successful reduction and healing.
For mature bones, the fracture location can be described based on the fracture location relative to the physis (i.e., the growth plate). Fractures can occur at the epiphysis, diaphysis, or metaphysis. Epiphyses are located distal to the physis and closest to the articular surface; the diaphysis is the central shaft of the long bone; the metaphysis is the wide, connecting segment between diaphysis and physis.
The Salter-Harris classification system is used to describe whether pediatric long bone fractures involve the physis, metaphysis, or epiphysis. The Salter-Harris classification system categorizes fractures around the physis into five types of fractures: Type 1 is a fracture through the physis alone; type 2 is a fracture through the metaphysis and physis; type 3 is a fracture through the physis and epiphysis; type 4 is a fracture through the metaphysis, physis, and epiphysis; and type 5 is a crush injury of the growth plate. The Salter-Harris system is useful in guiding treatment where type 1-3 fractures often can be reduced and splinted with outpatient orthopedic follow-up, while types 4 and 5 fractures are more likely to need emergent orthopedic consultation for further intervention because of an increased concern for growth arrest of the pediatric bone.3
There are many different ways to describe orthopedic bony injuries. To avoid confusion, using anatomical language is preferred.
Orthopedic Physical Exam and Imaging
A thorough yet directed physical exam is needed to guide appropriate imaging and treatment decisions. One way to think of the physical exam for orthopedic injuries is to use the IPPASS method: inspection, palpation, passive range of motion, active range of motion, strength testing, and special tests. Additionally, it is important to consider that bones transmit forces along their length and potentially into neighboring bony structures. Therefore, there should be consideration of examining both joints above and below an injury along with performing a distal neurovascular examination of the affected extremity to rule out vascular and nerve injury.
Physical examination of orthopedic injuries often is supported with diagnostic imaging, including plain radiographs, computed tomography (CT) scans, and magnetic resonance imaging (MRI). The imaging indicated for each orthopedic injury is discussed throughout the remainder of this article.
General Orthopedic Trauma Management
During a trauma evaluation, musculoskeletal injuries are evaluated and intervened upon during the secondary survey. However, there are some exceptions. When assessing for circulation during the primary survey, it is possible that a traumatic fracture or dislocation is compromising distal perfusion. Reducing an obviously dislocated extremity into better anatomic alignment often can recover distal perfusion. Additionally, in cases of massive hemorrhage, especially in the setting of open fractures and crush injuries, early control is crucial. While not definitive management, early tourniquet placement has been shown to save both life and limb. In a study published by Kragh et al in 2009, 2,838 injuries were evaluated. Those patients with early tourniquet placement had better chances of survival.4,5 More recent civilian prehospital data, specifically a 2019 retrospective analysis of penetrating trauma, showed that patients with early tourniquet placement had increased survival, decreased need for blood products, and decreased rate of limb complications.6 The American College of Surgeons Committee on Trauma (ACS-COT) and the American College of Emergency Physicians (ACEP) recommend tourniquets in life-threatening extremity hemorrhage.7,8
Fracture Complications
Open Fractures. Open fractures involve concurrent soft tissue injury that exposes bone to the outside environment, increasing the risk for bone infection. The severity of the open fracture injury has been further characterized using the Gustilo-Anderson (G-A) classification system.9 In brief, type I is defined as a minimal energy injury with relatively minimal soft tissue injury of less than 1 cm in length and minimal fracture comminution. Type II is defined as moderate-energy injury with moderate levels of soft tissue injury greater than
1 cm in length and moderate fracture comminution. Type III is the most severe, defined as high-energy injury resulting in severe tissue and/or vascular injury greater than 10 cm in length. Severe fracture comminution is seen with type III injuries. Type III is further subdivided by the majority type of soft tissue injury, including crush, significant soft tissue loss, and vascular injury.
While the G-A classification system has been adopted by both orthopedic and trauma specialty bodies to inform treatment guidelines, studies have demonstrated moderate variability among specialty surgeons in determining the specific type of G-A open fracture. For the initial provider, it is of greater importance to give early antibiotics and to allow further characterization of injury severity to be performed in the operating room where more specific antibiotic coverage can be decided as well.10
Open fractures are, by definition, infected, and early antibiotic therapy is of utmost importance. Studies have shown a marked increase in infection rates if they are not treated in a timely manner. One retrospective study indicated that antibiotics not applied to the most severe open fractures (G-A type III) within 66 minutes significantly increased the risk of infection.11 The increasing grade of open fracture injury dictates the type of antibiotics used per current guidelines; types I and II can be provided cephalosporin-based antibiotics, such as cefazolin or cefuroxime, for gram-positive skin flora.12 Type III injuries require expanded gram-negative coverage, primarily using an aminoglycoside such as gentamicin.9 Further, if there is evidence or concern for contamination of the wound with fecal matter or possible clostridial infection, such as with farm-associated injuries, high-dose penicillin is recommended.9 Patients allergic to cephalosporins may require alternative antibiotics, such as clindamycin.
All open fractures require adequate saline irrigation with or without Betadine, followed by coverage with Betadine- or saline-soaked bandages and limb immobilization. As with all traumatic soft tissue injuries, tetanus status should be assessed and appropriate coverage with vaccination and/or immunoglobulin therapy should be provided.
Compartment Syndrome. Compartment syndrome occurs when pressure within a fascial compartment exceeds the perfusion pressure, resulting in decreased blood flow and subsequent tissue ischemia and necrosis.13 The pathophysiology of compartment syndrome begins when the microcirculation is compromised, followed by cessation of venous and arterial blood flow.14 This is caused by an increase in compartment contents, decreased compartment volume, or external pressure. Compartment syndrome is a surgical emergency that threatens both life and limb. Crush injuries and other high mechanism trauma are most commonly associated with compartment syndrome. However, any time vascular damage, prolonged immobilization, or penetrating trauma is present, providers should maintain a high index of suspicion for compartment syndrome.15
Traditionally, the “five Ps” have been taught when describing compartment syndrome: pain out of proportion, pulselessness, paresthesia, pallor, and paralysis.14 Not all of the “five Ps” need to be present before intervention. Pallor and loss of pulses may occur only once arterial supply has been compromised, at which point the patient already may have sustained irreversible damage.14,15
Serial physical examinations evaluating compartment syndrome are key for early diagnosis and intervention. Normal compartment pressure is less than 10 mmHg. If the compartment pressure reaches
30 mmHg or greater, it is considered diagnostic for acute compartment syndrome. The calculation of a delta pressure as defined by the difference between the patient’s diastolic blood pressure and the intra-compartmental pressure also can be used to diagnose compartment syndrome if found to be less than or equal to
30 mmHg.15 Commercially available devices can aid in the evaluation of compartment pressures, and each device’s specific operative instructions should be noted prior to performing the evaluation.
Other tools may be considered for the evaluation of compartment syndrome, such as ultrasound to evaluate for vascular occlusion or creatine phosphokinase to evaluate for muscle breakdown. More recently, studies have had promising results surrounding the use of ultrasound and near-infrared spectroscopy, which measures tissue oxygenation, for the diagnosis of compartment syndrome.16-19
Nonetheless, physical exam and compartment pressures should guide treatment, including immediate surgical consultation and fasciotomy when indicated.
Shoulder Trauma
Clavicle Fracture
Clavicle fractures account for approximately 4% of all fractures, and they most commonly occur in male adolescents and elderly adults.20,21 The mechanism of injury for clavicle fractures is a direct fall onto the shoulder. Clavicle fractures can be divided into proximal, middle, and distal segment fractures. The middle third of the clavicle is the thinnest segment without any ligamentous attachments and is the most common site of fracture, with the distal clavicle being the second most common. Patients typically present with visible or palpable deformity with well-localized pain.
A complete neurovascular examination is required to assess for complications related to the fracture, including brachial plexus or subclavian vessel injury. Any skin tenting should be noted because this can lead to potential open fracture. Shortness of breath or diminished breath sounds may indicate an injury to the lung apex, resulting in pneumothorax or hemothorax.
Orthopedic surgery should be consulted immediately for patients with neurovascular injuries, open fractures, skin tenting, or severe displacement.22 The mainstay of treatment of nondisplaced clavicle fractures is analgesia, immobilization with a sling, and orthopedic follow-up.23 The treatment of displaced clavicle fractures is more nuanced, based on the degree of displacement, and ultimately is a decision that should be made by an orthopedic surgeon. Surgical management is associated with reduced risk of nonunion, malunion, or complications. However, data comparing surgical intervention to conservative management does not convincingly show improvement in long-term function.20-22,24,25
Scapular Fracture
Although uncommon, scapular fractures are important to identify because of their association with high-energy trauma, such as motor vehicle collisions (MVCs). They are commonly associated with polytrauma and rarely are found in isolation, including an association with pulmonary and cardiac injuries.26 Fractures to the scapula can include the scapular body, scapular neck, glenoid, acromion, or coracoid.
The physical exam should take special note of the neurovascular exam. Brachial plexus injuries are associated with scapula fractures in up to 13% of patients. Similarly, the blood supply surrounding the scapula can be compromised with significant fracture displacement or thoraco-scapular dissociations.26 Radiography often can miss scapular fractures. Therefore, if suspicion remains, a CT scan can provide clarity in the evaluation.27
The blade of the scapula is encased by the fibromuscular envelope of the rotator cuff muscles. The fibromuscular envelope provides stability and an ample blood supply. Therefore, the majority of scapula fractures are minimally displaced, and the risk of nonunion is very low.28 Minimally displaced scapula fractures can be managed conservatively with analgesia, immobilization with a sling, and physical therapy. Early mobility exercise is crucial to prevent adhesive capsulitis, also known as a frozen shoulder. Unlike the blade of the scapula, bony scapular processes, such as the glenoid, coracoid, and acromion, are more vulnerable to disruption and displacement.28 Most displaced fractures should be treated operatively because of a high-risk of long-term complications, such as arthritis and chronic instability.27,29
Proximal Humerus Fracture
Proximal humerus fractures (PHFs) present in a bimodal distribution by age and energy level. Young patients typically present following high-energy traumas, such as MVCs. Conversely, elderly patients classically present after a low-energy fall with the arm outstretched. PHFs are the fourth most common fracture in the elderly population and one of the most common osteoporotic fractures.30,31
The pertinent history to obtain when evaluating a potential PHF is previous injuries or surgeries to the limb, hand dominance, and living situation in elderly patients. The patient should be assessed specifically for potential axillary nerve injury. Associated signs of axillary nerve injury include a loss of deltoid contour, decreased sensation over the lateral shoulder, or weakness with abduction. Plain films are the initial imaging of choice. Radiographic imaging should include true anteroposterior (AP), scapular Y, and axillary lateral views.30
The Neer Classification can be used to classify PHFs based on morphological aspects. More simply, PHFs can be divided into minimally displaced and displaced fractures.32 Minimally displaced fractures often can be managed with sling immobilization followed by progressive rehabilitation. Displaced fractures often are managed surgically. Other surgical indications include concomitant soft tissue injuries, pathological fractures, neurovascular injury, or conservative treatment failure.33 Patient factors, such as age, comorbidities, and occupation, play a key role in patient selection for operative intervention.
Sternoclavicular Dislocations
Sternoclavicular joint (SCJ) dislocations are uncommon because of the strong ligamentous support of the joint. They commonly occur as a result of MVCs or collision sports, such as ice hockey or football, usually from direct impact with an anterior or posterior directed force.34 If present, there should be a high index of suspicion for other associated traumatic injuries.
Patients typically present with shoulder pain and diminished range of movement. On physical exam, a bony prominence or an indentation may be present over the SCJ based on the directionality of the dislocation.
Initial imaging for the assessment of SCJ dislocations is an AP radiograph. One also can consider obtaining a “serendipity view” radiograph to help distinguish superior or inferior displacement of the clavicle, which is difficult to assess on an AP chest X-ray alone. In a serendipity view, the XR beam is oriented 40 degrees toward the head and centered on the SCJ. Signs of SCJ dislocation can be subtle on radiography, and some joint space widening may be physiologic. Assess for potential joint space widening by comparing the SCJ to the contralateral side. In a suspected or radiograph-confirmed SCJ dislocation, CT scan is the imaging of choice, since this allows visualization of mediastinal structures and potential co-occurring injuries. Posterior dislocations can result in injury to the trachea, esophagus, brachial plexus, or great vessels in up to one-third of cases.35
Posterior SCJ dislocations are a surgical emergency requiring emergent consultation with an orthopedic surgeon and other appropriate surgical subspecialties depending on mediastinal structures involved. Conversely, acute anterior SCJ dislocations can be managed with closed reduction under general anesthesia in consultation with an orthopedic surgeon. Chronic anterior dislocations can be managed non-operatively with a sling.35,36
Acromioclavicular Injuries
Acromioclavicular (AC) joint injuries are common in young adults and athletes.37 The most common mechanisms of injury are a direct trauma to the lateral aspect of the shoulder or a fall onto an outstretched hand.
Patients typically present with swelling, limited range of motion, and tenderness at the AC joint. The physical exam may show swelling, bruising, or deformity of the AC joint.
Standard radiographs are the imaging of choice, including AP, lateral, and Zanca (AP view performed by tilting the beam 10-15 degrees cranial) views. (See Figure 1.) Weighted stress views also may be considered to help evaluate the degree of displacement.37
Figure 1. Left AC Separation |
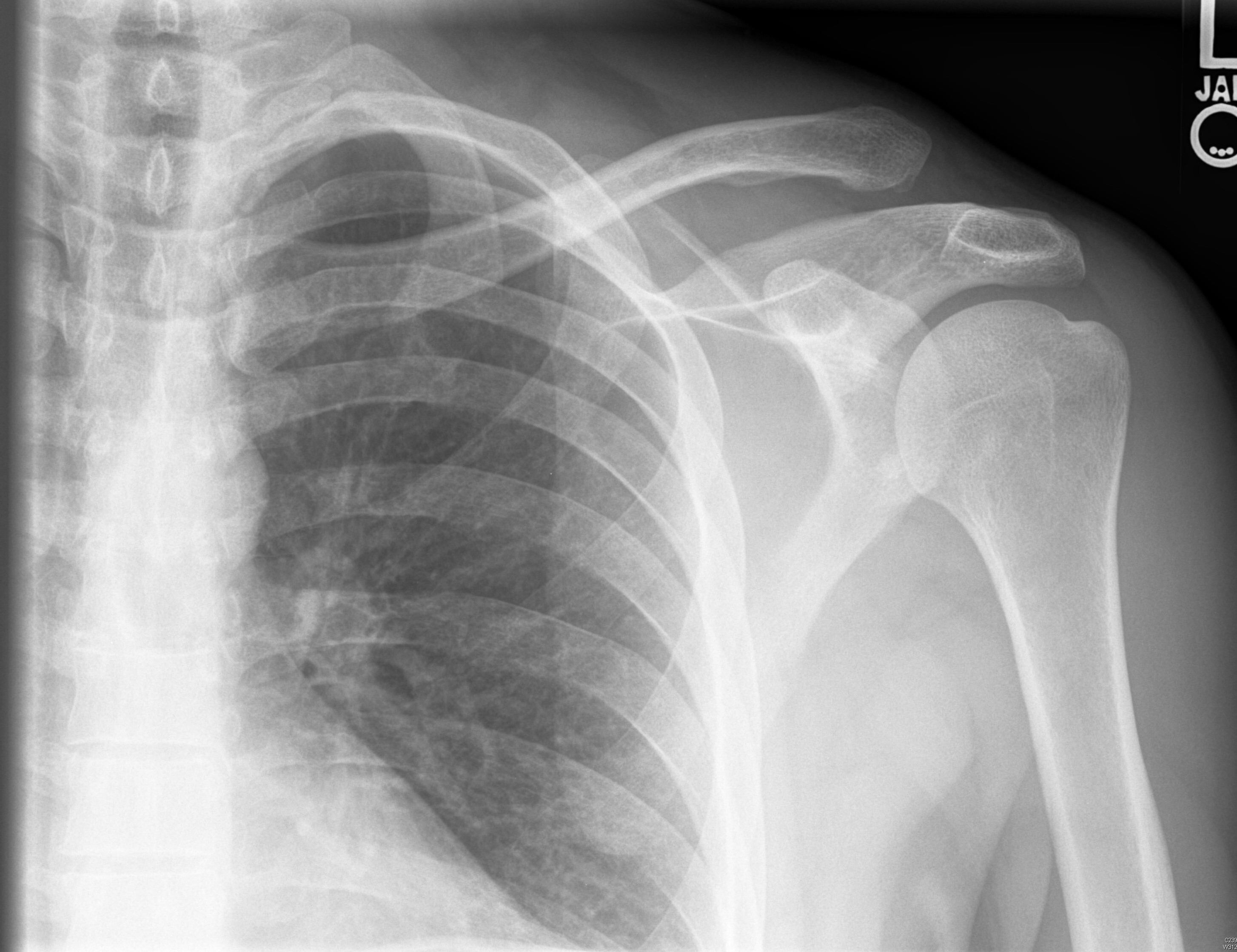 |
AC: acromioclavicular Source: Used with permission from J. Stephan Stapczynski, MD. |
The Rockwood classification is the gold standard to help guide management of AC joint injury.37-39 Type I injuries involve a sprain or partial tear to the AC ligament without clinical or radiographic evidence of coracoclavicular (CC) ligament injury or joint instability. Type II injuries include a complete tear of the AC ligament, a sprain, or partial tear to the CC ligament, with minimal joint displacement. Type III-VI injuries include completely torn AC and CC ligaments with worsening degrees of joint displacement.
Most AC joint injuries are type I or II injuries and can be managed non-operatively with a sling, analgesia, ice, and physical therapy. Type III-VI injuries may need surgical intervention, thus requiring an orthopedic surgery consultation. Of note, even for AC joints with high-grade injuries, there have been limited data to suggest that surgery improves shoulder function. Therefore, it is reasonable to start with an initial trial of conservative management.38-41
Glenohumeral Dislocation
Shoulder dislocations account for up to half of all major joint dislocations.42 The shoulder can dislocate in multiple directions because of the joint’s natural instability, with anterior dislocation being the most common. Patients with previous shoulder dislocations are more prone to repeat dislocation.42,43 Injury to the axillary nerve during shoulder dislocation is as high as 40%.42 Plain radiographs should be obtained with AP and scapular Y views to assess for glenohumeral dislocation. Associated fractures occur in up to one-quarter of dislocations.42 Tuberosity and surgical neck fractures are associated with avascular necrosis and are contraindications to closed reduction without orthopedic consultation. A Hill-Sachs deformity is a compression fracture of the posterolateral humeral head. A reverse Hill-Sachs lesion is an impact fracture of the anteromedial aspect of the humeral head and is seen in posterior dislocation. Bankart lesions refer to disruption of the glenoid labrum. (See Figure 2.)
Figure 2. Shoulder Dislocation with Bankart and Hill-Sachs Lesion |
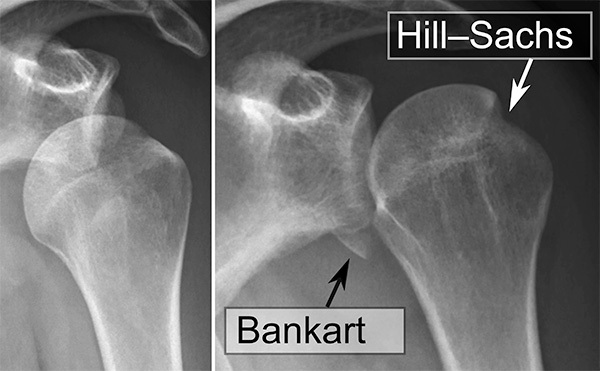 |
Source: Mikael Haggstrom, MD. https://commons.wikimedia.org/wiki/File:Shoulder_dislocation_with_Bankart_and_Hill-Sachs_lesion,_before_and_after_reduction.svg |
Several reduction techniques exist for each type of glenohumeral dislocation, and details of each maneuver go beyond the context of this article. General principles of reduction techniques include variations on traction and countertraction to restore anatomic alignment. Post reduction, the relocated extremity should have a repeat neurovascular exam to demonstrate injury did not occur during the reduction.
Anterior Glenohumeral Dislocation
Anterior shoulder dislocations are the most common type of glenohumeral dislocations and account for up to 97% of all shoulder dislocations.44 The mechanism of injury for anterior shoulder dislocation is commonly a fall onto an outstretched arm. Patients typically present with an abducted and externally rotated arm. An acutely dislocated shoulder should be reduced in a timely manner because delayed reduction increases the risk for neurovascular compromise.44-46
Posterior Glenohumeral Dislocation
Posterior dislocations account for up to 4% of shoulder dislocations.47 Usually, the injury is caused by an impact to the anterior shoulder and commonly is seen after seizures.
Posterior dislocations are easy to miss because the arm is in internal rotation and adduction. On AP radiograph, the posteriorly dislocated and internally rotated humeral head creates a “light bulb” sign, which may be noted. Nonetheless, posterior dislocation will be viewed best on the axillary view. (See Figures 3 and 4.) Posterior dislocations are at higher risk of surgical neck fracture, reverse Hill-Sachs lesions, and rotator cuff injuries.47,48
Figure 3. Posterior Dislocation Anteroposterior View |
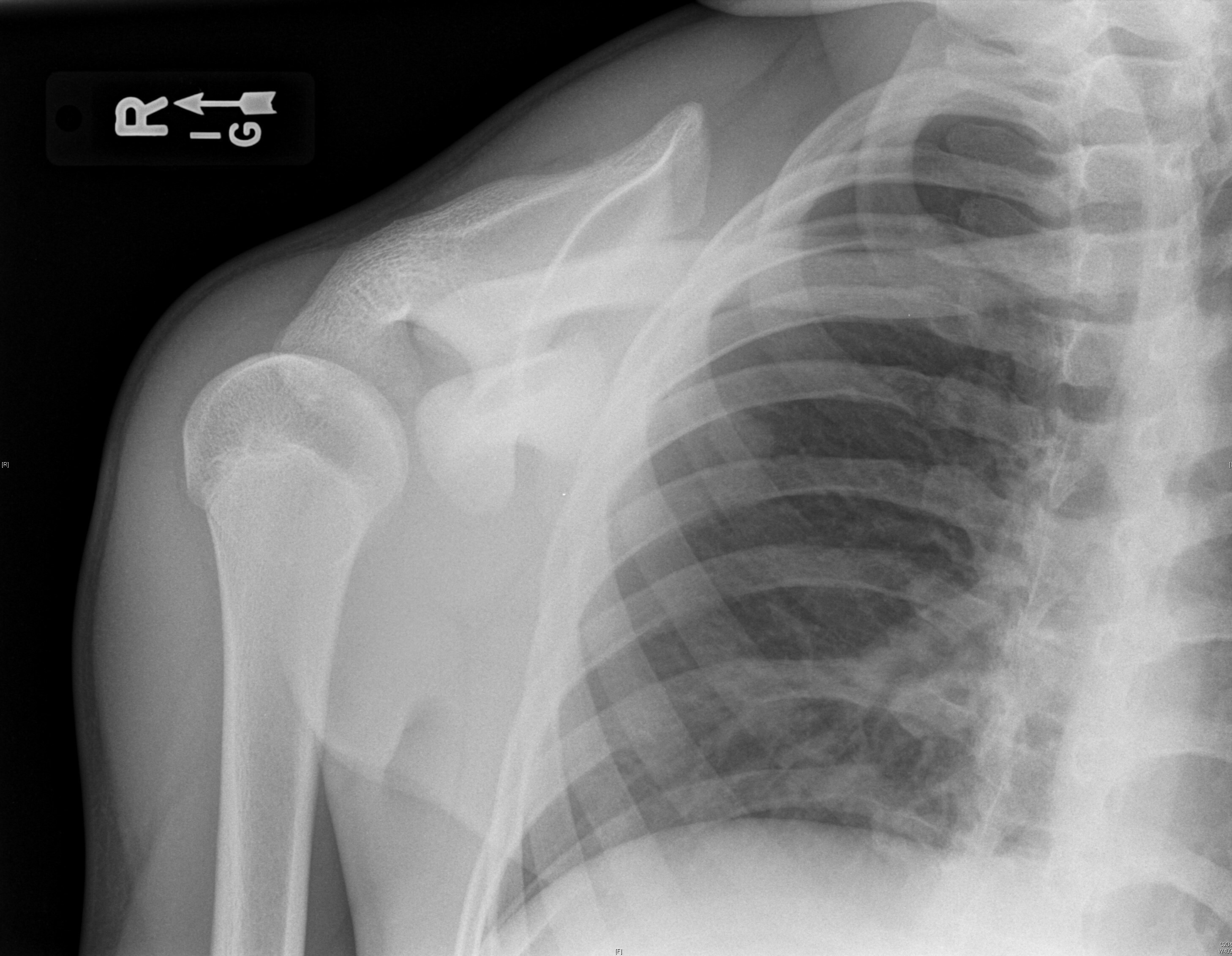 |
Source: Used with permission from J. Stephan Stapczynski, MD. |
Figure 4. Posterior Dislocation Axillary View |
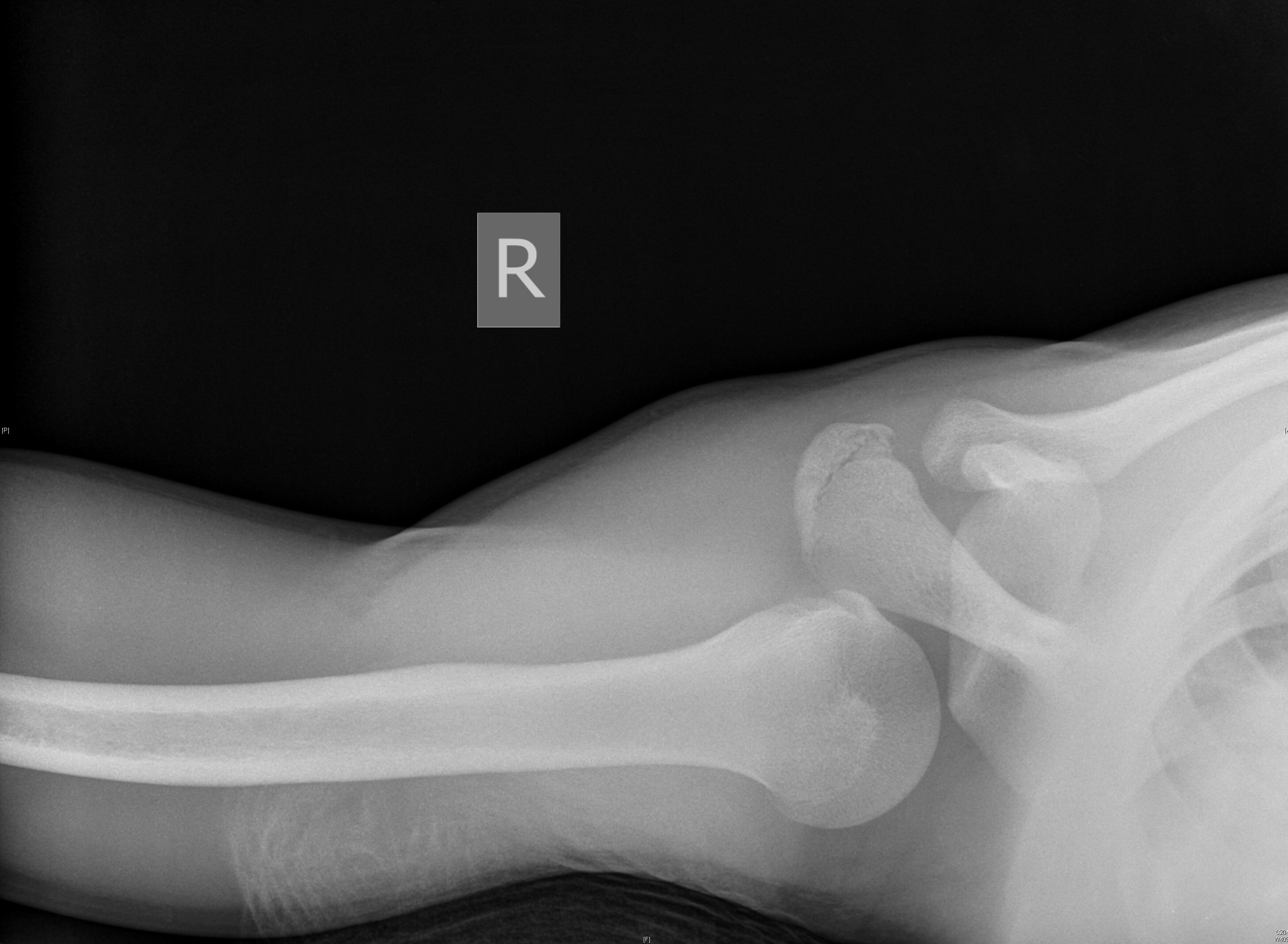 |
Source: Used with permission from J. Stephan Stapczynski, MD. |
Inferior Glenohumeral Dislocation
Inferior dislocations are the least common type of shoulder dislocation. The injury usually is caused by hyperabduction or with axial loading on the abducted arm. Patients typically present with the arm held above and behind the head, and unable to adduct the arm. Inferior dislocations have the highest incidence of axillary nerve and artery injury of all shoulder injuries.49
Pelvic Trauma
Pelvic Fractures
Pelvic injuries are a common presentation to the emergency department and can become life-threatening if complicated by hemorrhagic shock, injury to adjacent structures, and/or delay in care. Pelvic ring injuries account for approximately 3% to 8% of skeletal injuries.50 The most common mechanism for pelvic trauma is high-energy blunt force trauma; however, low-force trauma, such as falls, and penetrating trauma still can cause significant morbidity. Common blunt force mechanisms include: MVC (43% to 58%), pedestrian trauma (20% to 22%), falls (5% to 30%), and crush injuries and motorcycle accidents (5%).51-53 Associated internal injuries are the largest cause of fatality for those sustaining pelvic fractures. In patients 65 years of age or older, pelvic fractures have a mortality rate of up to 20%.54 Age, early physiologic derangements, and concomitant injuries to the head or trunk contribute to the high mortality rate associated with pelvic fractures in the elderly.53
Pelvic Ring Fractures
Pelvic ring fractures can be classified as non-displaced, mechanically stable fractures or displaced, mechanically unstable fractures. Stable fractures occur when one portion of the pelvic ring is disrupted, while the sacroiliac (SI) joint and symphysis pubis remain intact. These include avulsion fractures, single pubic ramus, single ischial ramus, ischial body, iliac wing, horizontal sacral, and coccygeal fractures. Of note, the most common pelvic fracture is a pubic rami fracture (70%), with predominance of the superior pubic rami compared to the inferior.51 These fractures occur near the symphysis pubis or SI joint, allowing for ring mobility reducing damage to adjacent structures.
Unstable fractures occur when two or more portions of the pelvic ring are disrupted. These account for 15% of pelvic fractures and are associated with high morbidity and mortality rates.55 Multiple studies have noted that the degree of instability is correlated with the amount of transfusion requirements if hemorrhage is present and the need for definitive intervention. Further, mortality associated with hemorrhage and shock accounts for up to 32% of patients.56
Several methods have been proposed to define pelvic ring fractures by location, severity, stability, and mechanism. The original system for classification was developed by Pennal and Southerland, and was based on the mechanism, as described by direction of force applied at the time of injury.57 Three mechanisms are described: anterior posterior compression (APC), lateral compression (LC), and vertical shear (VS). Young-Burgess and Tile adapted Pennal’s initial classification to further describe pelvic fractures, adding the combined mechanism (CM) category to describe complex trauma encompassing two or more of the original fracture patterns. Ultimately, all classifications are designed to use plain X-ray films to diagnose fractures in emergent situations.
Of note, vertical shear has been noted to produce the most unstable fracture pattern, whereas APC III have been shown to have the highest transfusion requirement, mortality, and associated neurologic injury.51
The Tile Classification exalts the importance of the posterior SI complex in maintaining pelvic stability and accounts for potential instability as a result of one of the three fracture patterns described by Pennal et al (anterior posterior compression, lateral compression, and vertical shear).51 This classification aids orthopedic surgeons and emergency physicians to predict prognosis and the need for surgical stabilization.
When discussing pelvic ring fractures, the nomenclature most commonly used to identify and classify injury is the Young-Burgess Pelvis Classification. This ensures all providers are describing the same injury, aiding in clear provider communication.
Associated Injuries
Injuries that affect the integrity of the pelvic ring are likely to affect adjacent structures within the bony pelvis.
Hemorrhage. When evaluating pelvic trauma in the emergency department, it is important to approach any trauma patient using the Advanced Trauma Life Support (ATLS) algorithm.58 The pelvis and retroperitoneum can hold up to 4 L of blood, making hemorrhagic shock the primary cause of death in pelvic trauma. Interventions focused on reducing the burden of hemorrhage, such as balanced resuscitation, use of tranexamic acid (TXA), improved access to angiography, and use of resuscitative endovascular balloon occlusion of the aorta (REBOA), have curtailed the mortality of these injuries.59
Most bleeding in pelvic trauma is venous in nature; however, true hemorrhagic shock often comes from arterial bleeding. In unstable fractures, pelvic binding can assist in hemorrhage control by attempting to anatomically approximate the pelvis to create a tamponade effect. Resuscitation can be initiated with whole blood transfusion, massive transfusion protocols, or guided transfusion based on coagulopathy markers.59-61
Definitive intervention via angiography with interventional radiology, external fixation with orthopedics, and/or exploratory laparotomy ultimately will control bleeding in these patients. Studies have shown that early angioembolization within the first 30 minutes to one hour has reduced morbidity and mortality.56,59,60,62 Consider angioembolization in clinically unstable patients where other sources of hemorrhage have been ruled out in initial ATLS evaluation. External fixators assist in reducing pelvic volume and creating a tamponade effect. Indications include unstable fracture patterns, such as APC II, APC III, LC II, LC III, and VS. Lastly, in patients with an unknown source of bleeding, damage control surgery with pelvic packing can be used to identify potential sources via direct visualization.
Genitourinary and Rectal. The most common visceral injuries in pelvic trauma are genitourinary. The bladder is the most affected organ, with an incidence up to 3.4% of cases, followed by the urethra in up to 1% of cases.63 Physical exam findings include blood at the urinary meatus, blood at the vaginal introitus, perineal ecchymosis, high riding prostate in males, and rectal bleeding. In patients with suspected genitourinary trauma, a CT retrograde urethrogram must be performed. A positive result will note contrast extravasation on imaging. Urology should be consulted for further management. For partial or small urethral tears, treatment includes placement of a Foley catheter, whereas in more complex tears, treatment may require more definitive intervention in the operating room. Treatment for rectal trauma includes early diverting colostomy with washout of the distal colon and presacral space drainage.64 Administer antibiotics that cover gram-negative organisms as soon as the injury is discovered.
Neurologic. Nerve root deficits associated with pelvic ring disruptions occur in 10% to 15% of pelvic trauma cases, with higher rates (up to 50%) in sacral fractures.63-64 The incidence increases with the degree of instability: 1.5% in stable fractures vs. 14.4% in unstable fractures.63 The most common sites include the L5 and S1 nerve roots and isolated peripheral nerves. Physical exam findings include decreased strength and/or sensation in the lower extremity, usually following the nerve root distribution.
Avulsion Fractures
Avulsion fractures are stable pelvic fractures. These occur in the skeletally immature pelvis, with peak age at 14 to 17 years, affecting mostly males (75%).58 The pathophysiology is due to forceful muscle contraction during high-impact activities causing a small fragment of bone to be separated from the body of the bony pelvis. Most commonly affected sites include anterior inferior iliac spine (33.2%), ischial tuberosity (29.7%), anterior superior iliac spine (27.9%), iliac crest (6.7%), lesser trochanter (1.8%), and superior corner of the pubic symphysis (1.2%).51 Avulsion fractures do not have associated injuries. They are diagnosed with AP X-ray films. Physical exam findings include tenderness at the avulsion site and painful range of motion. In adults, avulsion fractures should be considered pathologic until proven otherwise. Treatment is determined by the degree of displacement; for fractures
10 mm to 15 mm displaced, surgery is indicated. For minimally displaced fractures, conservative treatment involves being made non-weight bearing and returning to activity in three to four weeks.51 Complications can include chronic pain and bony overgrowth at the area of avulsion. In patients undergoing surgical management, return to baseline activity was shown to be higher compared to those undergoing conservative management.51
Acetabular Fractures
Acetabular fractures most commonly are caused by MVCs. The most common type of acetabular fracture involves both anterior and posterior columns, whereas isolated posterior column fractures are more common than anterior column fractures. Letournel and Judet described a classification system for acetabular fractures.50-51,58,65
Physical exam will show tenderness at the hip joint, painful range of motion, and potential limb length discrepancy depending on the degree of fracture displacement. Presentation can be associated with hip dislocations, pelvic ring disruption, femoral head fractures, pubic rami fractures, and ipsilateral limb fractures. Halverson et al described that patients with combined acetabular and pelvic ring fractures compared to those with isolated acetabular fractures usually were polytraumas, had greater transfusion requirements, and more often required operative repair. They also noted that delay in hemorrhage control, reduction, and definitive fixation affected long-term functionality.50
Acetabular fractures are evaluated with a plain film radiographic protocol known as Judet views. These include an anteroposterior film, a 45-degree iliac oblique view, and a 45-degree obturator oblique view. CT scans are more sensitive than plain films when detecting acetabular injury, providing detailed information about fracture displacement, fragmentation, and degree of comminution. For these reasons, CT scans should be obtained after identification of an acetabular fracture on plain films or when acetabular fractures are not visualized on radiographs although the clinical exam remains concerning for an acetabular fracture.61,65
Definitive management can range from nonoperative to operative. Open reduction with internal fixation (ORIF) is recommended for displaced fractures > 2 mm. Nonoperative management ranges from traction to full weight-bearing status. For fractures involving the weight-bearing dome, closed treatment with traction to prevent further displacement is required. If the weight-bearing dome is not involved, the patient can bear weight as tolerated.
Acetabular fractures are associated with significant morbidity due to complications related to time to reduction. Complications include arthritis, avascular necrosis, and sciatic nerve injury. Osteoarthritis can be seen in most fractures, and traumatic arthritis has been reported in severely displaced patterns. Avascular necrosis may occur up to a year after the injury. This is dependent on fracture type and time to reduction, with delay in reduction reported to have an incidence of 48%. Sciatic nerve injury is associated with up to 13% of acetabular injuries, delaying recovery time and causing prolonged morbidity.50-51,62
Hip Trauma
Hip Fractures
Hip fractures are a major public health issue, with significant morbidity and mortality rates. Recent studies have highlighted the increasing incidence of hip fractures, with a study published in 2021 finding the incidence of hip fractures among older adults increased by 14% from 2010 to 2018 in the United States.66 The estimated one-year mortality among elderly patients with a hip fracture is between 20% and 30%.67 There is a bimodal age distribution of hip fractures, with young males sustaining high-energy trauma and elderly patients involved in low-energy trauma.68
Hip fractures can be divided into femoral neck fractures, intertrochanteric fractures, and subtrochanteric fractures. Femoral neck fractures occur between the femoral head and trochanters. Intertrochanteric fractures occur between the greater and lesser trochanter. Lastly, subtrochanteric fractures are proximal femoral shaft fractures that occur below the intertrochanteric region and within
5 cm of the lesser trochanter.
Clinically, patients will present with hip and thigh pain, which is worse with movement. If there is displacement, the limb may be shortened, flexed, externally rotated, and abducted. Plain films serve as first-line imaging to assist in defining the type of hip trauma. However, if radiographs are negative and clinical suspicion remains, CT can be beneficial in further defining occult fractures since approximately 3% to 4% of hip fractures will not be identified by X-ray.68 Recent studies comparing the diagnostic accuracy of MRI, CT, and bone scans for the detection of occult hip fractures demonstrated MRI to have a higher sensitivity and specificity than CT or bone scans, although it was not found to make a significant difference in clinical outcomes.69
Hip fractures typically require orthopedic consultation for surgical management. Given the high morbidity and mortality, nonoperative management often is reserved for non-ambulatory patients with minimal pain and those with comorbidities putting them at high risk for surgery and anesthesia. Nerve blocks can be of great use for providing pain relief while patients await surgical intervention and at the time of surgery. The fascia iliaca and femoral nerve blocks have been found to provide better pain control than opioids, to help individuals get back to their baseline function quicker, to tend to decrease length of stay in the hospital, and to decrease 30-day readmission if the block was done while in the emergency department.70,71
Hip Dislocations
Hip dislocations can be either anterior or posterior in nature based on the positioning of the femoral head. Posterior hip dislocations occur when there is a posterior to anterior force placed on the knee while the hip is flexed and adducted (i.e., when the knee hits the dashboard in an MVC).72 Anterior hip dislocations occur when the hip is flexed and forced into abduction and external rotation.73 Posterior hip dislocations will present with a shortened, adducted, flexed, and internally rotated lower extremity. Conversely, anterior hip dislocations present with the hip flexed, abducted, and externally rotated.
Radiographs should be obtained to help with the initial diagnosis of a hip dislocation. Post reduction, radiographs should be repeated to confirm anatomic alignment, and CT imaging should be obtained to evaluate for occult fractures.74
Hip reduction is the treatment of choice and should be completed within six hours to help prevent neurovascular complications.74 There are multiple reduction techniques available for both posterior and anterior dislocations, although the details of these go beyond the scope of this article. Operative management is reserved for hip dislocations that fail reduction, have intra-articular fractures, or have been dislocated for a prolonged period of time.74
Femoral Head Fractures
Femoral head fractures occur most commonly after hip dislocation. Open reduction and internal fixation is the best treatment of choice in traumatic fractures of the femoral head. However, for some fractures there simply may be small fragments, and other options can include arthroscopy vs. percutaneous removal. Percutaneous removal has only been described in limited literature.75 However, arthroscopy has been shown to have a low complication profile in terms of complications post repair compared to open fixation.76
Knee Trauma
Distal Femur Fractures
Fractures of the distal femur are rare injuries, encompassing 3% to 6% of all femoral fractures.77 Fracture classification is done most commonly using the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association (AO/OTA) system, with fracture patterns that include type A (extra-articular), type B (partial articular/unicondylar), and type C (complete articular/bicondylar). The progressively increasing degree of comminution is used to further classify into subtypes 1, 2, and 3.78
Patients with suspected distal femur fractures typically present after trauma with knee pain or hip pain accompanied by inability to bear weight on the affected extremity, tenderness over the distal femur, swelling, and/or deformity. Such fractures usually occur because of a direct impact to the distal femur. Because of the surrounding muscular attachments, displacement of the fracture fragments is common, therefore contributing to the difficulty of achieving and maintaining adequate reduction.79 Further complicating matters is the proximity of the popliteal artery and vein to the distal femur, making these structures prone to injury with such fractures.
Five percent to 10% of supracondylar distal femur fractures are open.79 Therefore, initial evaluation should include a careful skin assessment to evaluate for open fractures or other soft tissue injuries that may complicate the treatment course.
The neurovascular status of the affected lower extremity should be assessed thoroughly. If weak pulses are found, further assessment for possible arterial injury should be done using a Doppler probe and obtaining ankle brachial index (ABI). An ABI < 0.9 or obvious signs of vascular injury would necessitate obtaining angiography.80
Plain imaging begins with AP and lateral radiographs of the affected knee and ipsilateral hip to rule out concomitant injuries. CT is recommended for more comprehensive preoperative characterization of articular surfaces and degree of comminution and intra-articular extension in suspected type B and type C fractures.77
Treatment of distal femur fractures can be either nonoperative or operative. Nonsurgical treatment options comprise various methods of immobilization, including skin/skeletal traction, long leg splints, or casts. Generally, it will involve the use of an unlocked, hinged knee brace, which can allow for either protected weight or non-weight bearing while maintaining range of motion, with interval imaging done to monitor healing progress.78 Surgical reduction and fixation is indicated for displaced, intra-articular fractures of the distal femur. The primary goal of surgical intervention is the restoration of the articular unit to the shaft and anatomic alignment while maintaining stability to enable early range of motion and rehabilitation.77
Tibial Plateau Fractures
Tibial plateau fractures encompass a variety of articular injuries of the proximal tibia, often accompanied by injuries of the surrounding soft tissues. These fractures traditionally are classified using the Schatzker classification that was based on a two-dimensional representation of the fracture pattern. More recent attempts have been made to incorporate CT data into this classification to develop a three-dimensional classification. The goal of this new model is to improve perioperative planning involving patient positioning, surgical approach, and identifying areas where hardware can be applied to achieve stable fixation.81
Fractures of the tibial plateau typically have a bimodal distribution affecting young adults or the elderly and can involve both high- or low-energy trauma.82 The characteristics of the fracture and its severity are dependent on the vector upon which the load was applied, amount of energy involved, and the patient’s underlying bone quality. The direction of the rotational stress on the knee during the injury will determine whether the medial or lateral plateau is affected, with the lateral plateau being involved in most cases.82
Meniscal and ligamentous injuries commonly accompany these fractures. In one study of patients presenting with tibial plateau fractures of various Schatzker types, 77% presented with a complete anterior cruciate or lateral cruciate ligament injury, whereas 81% presented with lateral meniscal tear and 44% with a medial meniscal tear.83 The presence of such injuries can affect treatment and timing of operative interventions; therefore, initial evaluation should include careful examination for open injuries or soft tissue damage.
Other complications can include compartment syndrome and neurovascular injury, most commonly involving the peroneal nerve.
Initial radiograph imaging generally involves AP, lateral, and oblique views. With increased use of CT imaging, oblique views have become less important, although they can be helpful in determining the amount of articular depression.
Generally, tibial plateau fractures are treated operatively, but they can be managed nonoperatively with closed reduction and immobilization in certain patient populations. Consultation with orthopedic surgery is indicated to assist with decisions in management.83 Indications for nonoperative treatment involve fracture morphology that is minimally displaced or depressed, low-energy trauma resulting in a fracture that is stable on stress testing, non-ambulatory patient, and significant comorbidities preventing safe surgery. The goal of operative treatment is preservation of the tissue vascularity and restoration of joint congruity and mechanical axis of the limb. Surgical options include ORIF, external fixation and minimal osteosynthesis (EFMO), or arthroplasty. In complex articular fractures, the gold standard treatment is ORIF.83
Tibial Spine Fracture
Tibial spine fractures are rare injuries that generally were thought to be more common in the pediatric population. More recent literature suggests the incidence in adults may be higher than previously thought, with evidence suggesting accompanying injury to nearby collateral ligaments and menisci may be more common in adults.84 The injury mechanism involves an anterior or posterior force being applied to the proximal tibia while the knee is in flexion. Fractures of the anterior tibial spine are more common than of the posterior tibial spine, with the incidence of anterior fractures being approximately three per 100,000/year.84
Because the tibial spine is the attachment site for the anterior cruciate ligament (ACL), initial presentation of a tibial spine fracture may mimic an ACL tear since disruption of the tibial spine will lead to ACL deficiency. Fractures that are non-displaced can be treated nonoperatively with immobilization, whereas displaced or completely avulsed fractures necessitate orthopedic surgery consultation for surgical repair. In adults, tibial spine fractures carry a significant risk of developing knee stiffness and instability, with stiffness being a more common finding in the operatively treated group vs. the nonoperative group.84
Knee Dislocations
Knee dislocations are rare traumatic injuries representing between 0.02% and 0.2% of orthopedic injuries and occurring more often in younger patients, with a 4:1 male-to-female ratio.85 Mechanisms of injury can involve high or low energy. A knee dislocation is defined as disruption of at least two of the four major ligamentous components of the knee: ACL, popliteo-fibular ligament (PCL), and medial collateral ligament (MCL). More commonly, though, dislocations cause disruption of the ACL, PCL, plus one or more other structures. Classification traditionally is based on the direction of tibial dislocation in relation to the femur.
Anterior dislocations are the most common, occurring in 40% of cases.85 Hyperextension injuries lead to anterior dislocations, whereas posteriorly directed forces resulting in axial loading to a flexed knee (as can occur during dashboard injuries) will lead to posterior dislocations.85 Varus or valgus loads will lead to medial (4%) or lateral (18%) dislocations. Nearly 10% of knee dislocations are from simple falls, with some studies also reporting spontaneous dislocations associated with morbid obesity.85
Initial assessment of acute knee dislocation should involve thorough skin assessment and neurovascular examination. In 5% to 17% of cases, the injury is reported as open.85 The proximity of the popliteal artery makes vascular injury a concern, with recent literature suggesting a 7.5% to 14% incidence of vascular lesions.85 Emergent surgical intervention is required in the presence of obvious vascular injury causing acute limb ischemia. Rapid reduction, frequent vascular examinations, ABI, and angiography all can be used in the assessment for vascular compromise. Peripheral nerve injuries also are relatively common, with a 14% to 25% reported incidence of common peroneal nerve injuries and, less commonly, tibial nerve injury.85
Following reduction and neurovascular assessment, limb immobilization should be done to provide stability and pain control. The knee should be immobilized in 20 degrees of flexion to prevent posterior tibial subluxation.85 An external fixator can be placed during immobilization if there is vascular injury necessitating immediate surgical intervention.
Post-reduction radiographs can be used to assess for any other nearby bony injuries. To further characterize the extent of injury for proper preoperative planning, an MRI should be obtained after successful reduction and immobilization.
Management options can involve nonoperative or operative approaches. Recent literature suggests superior outcomes with early surgical intervention compared to nonoperative management.85 Indications for nonoperative management with immobilization include successful reduction without vascular injury; however, most cases tend to require some form of surgical stabilization. The most common long-term complications are stiffness and laxity/instability. Some studies have reported up to 50% of patients may develop osteoarthritis of the affected joint.85
Proximal tibiofibular dislocation or subluxation is a rare injury most seen in athletes applying strong twisting motion on a flexed knee. More recent literature has suggested injuries of the proximal tibiofibular joint may be more common than previously thought, since the differential diagnosis can be complex and the diagnosis often may be missed.86 Patterns of joint instability can be atraumatic subluxation, anterolateral dislocation (most common), posteromedial dislocation, or superior dislocation. Patients with an acute dislocation of this joint present with pain and swelling over the lateral knee accompanied by difficulty or inability to bear weight. Other concomitant symptoms may be apparent depending on the pattern of injury. Lateral collateral ligament injuries frequently are associated with anterolateral dislocations, peroneal nerve injuries often accompany posteromedial dislocations, and ankle injuries can be associated with superior dislocations since the mechanism often involves a high-energy superiorly directed force to displace the fibula superiorly.
Initial examination should involve assessment for LCL stability and integrity of the posterolateral structures of the knee because these structures are most often injured with proximal tibiofibular joint dislocations. AP and lateral radiographs should be obtained. Radiographs of the contralateral knee, if available, can be helpful comparison studies in the diagnosis of this injury. Ultimately, CT is the most sensitive imaging modality for this type of injury and should be obtained if the diagnosis is suspected despite normal plain radiographs.
Treatment involves closed reduction with application of appropriately directed force on the fibular head with the knee flexed between 80 and 110 degrees.86 Knee flexion relaxes the LCL and biceps femoris tendon. An audible pop often is reported as the fibula reduces. Reassessment of LCL and posterolateral knee structures should be performed following reduction. Immobilization is controversial without current consensus. One study reported 57% of patients with acute proximal tibiofibular dislocations required surgery in the future because of continuing symptoms after closed reduction and immobilization for three weeks.86 Indications for surgical treatment include failure of closed reduction and posteromedial dislocations since these have been associated with worse results with nonoperative treatment.
Knee Extensor Mechanism Injuries
The knee extensor mechanism is comprised of the patella, patellar tendon, and quadriceps tendon.
Fractures of the patella are traumatic knee injuries that account for 1% of all skeletal fractures.87 The mechanisms involved in such injuries include direct trauma or eccentric contraction. High-impact injuries may be associated with hip dislocations and/or fractures. An eccentric contraction of the quadriceps muscle while the knee is rapidly flexed can lead to quadriceps or patellar tendon injury resulting in the loss of extensor mechanism.
Patellar fracture classifications can be based on fracture pattern descriptors or AO/OTA classification. Patients may present after knee trauma with palpable patellar defects, significant hemarthrosis, and inability to perform a straight leg raise. Diagnosis can be made clinically with inability to perform a straight leg raise. Plain radiographs will confirm the diagnosis and involve AP, lateral, and axial views. Bipartite patella are normal anatomic variants affecting 2% to 3% of the population that can be mistaken for patellar fractures.87
Treatment options involve nonoperative or operative approaches depending on the degree of fracture displacement and extensor mechanism integrity. Nonoperative treatment involves immobilizing the knee in extension with full weight bearing. Indications include intact extensor mechanism, nondisplaced or minimally displaced fracture, or presence of significant comorbidities. Surgery is performed with the goal to preserve the patella whenever possible. Operative options include ORIF or patellectomy if ORIF is not possible in the setting of significant comminution. Surgery indications include failure of the extensor mechanism, open fractures, and significant displacement of more than
3 mm.87
Patellar dislocations often occur in adolescents or active individuals. The usual mechanism associated with dislocation of the patella involves direct impact of the knee in extension while the foot is externally rotated, although it also can occur with a sudden lateral cut or twisting at the knee. Patients present with significant pain of the affected knee with obvious displacement of the patella. Individuals who have an acute patellar dislocation often are at increased risk of repeated dislocations resulting from recurrent patellar instability.88 Risk of future re-dislocation is determined by the degree of injury involving the major stabilizing ligament of the patella, the medial patellofemoral ligament (MPFL). Imaging generally is not required prior to reduction unless there is concern for accompanying fracture. While no clear consensus exists on the approach to treating a first patellar dislocation, treatment tends to begin with conservative options involving closed reduction, immobilization, and weight-bearing as tolerated. Indications for surgery include the presence of patellar displacement or osteochondral fractures since these can lead to increased risk of re-dislocation in the future. In cases where the MPFL has avulsed from the patella, an MPFL repair or reconstruction could be performed. Evidence has shown MPFL reconstruction to be more reliable than repair.88
Patellar and quadriceps tendon ruptures are uncommon injuries that occur with direct or indirect trauma. Isolated tears of these tendons can occur with direct trauma and have less pronounced effect on the extensor mechanism since medial and lateral retinacula typically remain intact. In contrast, indirect trauma can result in complete transection of the extensor mechanism.89 Normal tendons in healthy patients usually do not rupture under stress and are able to tolerate 17.5 times the normal body weight.89 Chronic illnesses, including chronic renal failure, diabetes, connective tissue disorders, hyperparathyroidism, systemic steroid use, and fluoroquinolone use, can accelerate tendon decline and predispose individuals to tendinous injuries.90
Quadriceps tendon rupture, occurring more commonly than patellar tendon rupture, involves disruption of the tendon at its insertion site on the patella. It typically occurs in adults, with male-to-female ratio of 8:1.91 The mechanism of injury involves eccentric loading occurring when the foot is planted and the knee slightly bent.92 Patients with this injury will present with pain and an accompanying palpable defect approximately 2 cm proximal to the superior pole of the patella. The patient will be unable to perform a straight leg raise because of extensor mechanism disruption. Diagnosis can be made clinically and confirmed radiographically with AP and lateral views of the knee.89 MRI can be indicated in certain situations where the diagnosis is unclear or differentiation between partial or complete tear is needed. Treatment can be done nonoperatively with brace and knee immobilization in patients with partial tears and intact extensor mechanisms or those in whom surgery is contraindicated. In cases where there is disruption of the extensor mechanism, surgery is indicated and involves primary repair with reattachment to the patella.
Patellar tendon rupture is a rare injury occurring in adults, with a predisposition for affecting males.93 The mechanism of injury involves abrupt quadriceps contraction while the knee is flexed (as may occur in sports involving jumping). The greatest force applied on the tendon occurs when the knee is flexed > 60 degrees.94 Patients present with pain often accompanied by hearing or feeling a popping sensation with rapid development of swelling and difficulty weight bearing. Examination involves localized tenderness, inability to perform straight leg raise, visibly elevated patellar height, and a palpable gap below the inferior pole of the patella. Plain radiographs include AP and lateral views while the knee is flexed at 30 degrees. MRI is the most sensitive imaging modality and can be obtained to differentiate partial vs. complete rupture.93 Although user-dependent, ultrasound also can be used to evaluate for tendinous disruption.
Nonoperative treatment with immobilization in full extension followed by rehabilitation can be done for partial tears with intact extensor mechanism. Surgery with primary repair is indicated for complete ruptures. If unable to approximate the tendon at the site of disruption due to a severely disrupted or degenerated tendon, a tendon reconstruction may be performed instead.
Conclusion
Traumatic orthopedic injuries represent a significant risk to both life and limb. The management of these injuries requires a large breadth of knowledge for which this article provides a foundation. Early recognition of fractures and dislocations allows for more swift definitive intervention. Reduction, stabilization, and hemorrhage control can begin as early as the prehospital setting. Frequent reassessments are crucial in recognizing complications of traumatic orthopedic injuries, such as neurovascular injury, infections, or compartment syndrome. When indicated, orthopedic surgery should be consulted to help preserve long-term function of the injured extremity.
REFERENCES
- Jarman MP, Weaver MJ, Haider AH, et al. The national burden of orthopedic injury: Cross-sectional estimates for trauma system planning and optimization. J Surg Res 2020;249:197-204.
- O’Hara NN, Isaac M, Slobogean GP, Klazinga NS. The socioeconomic impact of orthopaedic trauma: A systematic review and meta-analysis. PLoS One 2020;15:e0227907.
- Levine RH, Thomas A, Nezwek TA, Waseem M. Salter-Harris Fractures. In: StatPearls [Internet]. StatPearls Publishing; 2023 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK430688/
- Kragh JF Jr, Walters TJ, Baer DG, et al. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg 2009;249:1-7.
- Dorlac WC, DeBakey ME, Holcomb JB, et al. Mortality from isolated civilian penetrating extremity injury. J Trauma 2005;59:217-222.
- Smith AA, Ochoa JE, Wong S, et al. Prehospital tourniquet use in penetrating extremity trauma: Decreased blood transfusions and limb complications. J Trauma Acute Care Surg 2019;86:43-51.
- Bulger EM, Snyder D, Schoelles K, et al. An evidence-based prehospital guideline for external hemorrhage control: American College of Surgeons Committee on Trauma. Prehosp Emerg Care 2014;18:163-173.
- American College of Emergency Physicians. Out-of-hospital severe hemorrhage control. Policy statement. Ann Emerg Med 2015;66:693.
- Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. J Bone Joint Surg Am 1976;58:453-458.
- Kim PH, Leopold SS. In brief: Gustilo-Anderson classification. [corrected]. Clin Orthop Relat Res 2012;470:3270-3274.
- Lack WD, Karunakar MA, Angerame MR, et al. Type III open tibia fractures: Immediate antibiotic prophylaxis minimizes infection.J Orthop Trauma 2015;29:1-6.
- Hoff WS, Bonadies JA, Cachecho R, Dorlac WC. East Practice Management Guidelines Work Group: Update to practice management guidelines for prophylactic antibiotic use in open fractures. J Trauma 2011;70:751-754.
- Tillinghast CM, Gary JL, Mauffrey C, Hak DJ, Martin III MP, editors. Chapter 8: Compartment Syndrome of the Lower Extremity. In: Compartment Syndrome: A Guide to Diagnosis and Management [Internet]. Springer; 2019. https://www.ncbi.nlm.nih.gov/books/NBK553915/
- Hansen EL, Pedersen L, Lindberg-Larsen M. [Acute compartment syndrome]. [Article in Danish]. Ugeskr Laeger 2021;183:V11200817.
- Torlincasi AM, Lopez RA, Waseem M. Acute Compartment Syndrome. [Updated 2022 Aug 7]. In: StatPearls [Internet]. StatPearls Publishing; 2022 Jan-.
- Long B, Koyfman A, Gottlieb M. Evaluation and management of acute compartment syndrome in the emergency department. J Emerg Med 2019;56:386-397.
- Marmor M, Charlu J, Knox R, et al. Use of standard musculoskeletal ultrasound to determine the need for fasciotomy in an elevated muscle compartment pressure cadaver leg model. Injury 2019;50:627-632.
- Mühlbacher J, Pauzenberger R, Asenbaum U, et al. Feasibility of ultrasound measurement in a human model of acute compartment syndrome. World J Emerg Surg 2019;14:4.
- Cole AL, Roskosky M, Shuler MS, Freedman BA. Near infrared spectroscopy and lower extremity acute compartment syndrome: A review of the literature. J Trauma Treat 2014;s2:01.
- Lenza M, Buchbinder R, Johnston RV, et al. Surgical versus conservative interventions for treating fractures of the middle third of the clavicle. Cochrane Database Syst Rev 2019;1:CD009363.
- Moverley R, Little N, Gulihar A, Singh B. Current concepts in the management of clavicle fractures. J Clin Orthop Trauma 2020;11(Suppl 1):S25-S30.
- Bentley TP, Hosseinzadeh S. Clavicle fractures. In: StatPearls [Internet]. StatPearls Publishing; 2023.
- Qin M, Zhao S, Guo W, et al. Open reduction and plate fixation compared with non-surgical treatment for displaced midshaft clavicle fracture: A meta-analysis of randomized clinical trials. Medicine 2019;98:e15638.
- Asadollahi S, Bucknill A. Acute medial clavicle fracture in adults: A systematic review of demographics, clinical features and treatment outcomes in 220 patients. J Orthop Traumatol 2019;20:24.
- Shi F, Hu H, Tian M, et al. Comparison of 3 treatment methods for midshaft clavicle fractures: A systematic review and network meta-analysis of randomized clinical trials. Injury 2022;53:1765-1776.
- Libby C, Frane N, Bentley TP. Scapula Fracture. In: StatPearls [Internet]. StatPearls Publishing; 2023.
- Pires RE, Giordano V, de Souza FSM, Labronici PJ. Current challenges and controversies in the management of scapular fractures: A review. Patient Saf Surg 2021;15:6.
- Limb D. Scapula fractures: A review. EFORT Open Rev 2021;6:518-525.
- Ström P. Glenoid fractures of the shoulder. EFORT Open Rev 2020;5:620-623.
- Pencle FJ, Varacallo M. Proximal Humerus Fracture. In: StatPearls [Internet]. StatPearls Publishing; 2023.
- Soler-Peiro M, García-Martínez L, Aguilella L, Perez-Bermejo M. Conservative treatment of 3-part and 4-part proximal humeral fractures: A systematic review. J Orthop Surg Res 2020;15:347.
- Brorson S, Palm H. Chapter 10: Proximal humeral fractures: The choice of treatment. In: Falaschi P, Marsh D, eds. Orthogeriatrics: The Management of Older Patients with Fragility Fractures [Internet], 2nd ed. Springer; 2021.
- Gallusser N, Barimani B, Vauclair F. Humeral shaft fractures. EFORT Open Rev 2021;6:24-34.
- Jang ES, Park CN, Levine WN, Popkin CA. A Current Concepts review of clavicle injuries in ice hockey from sternoclavicular to acromioclavicular joint. Orthop J Sports Med 2020;8:2325967120951413.
- Kiel J, Ponnarasu S, Kaiser K. Sternoclavicular joint injury. In: StatPearls [Internet]. StatPearls Publishing; 2023.
- Garcia JA, Arguello AM, Momaya AM, Ponce BA. Sternoclavicular joint instability: Symptoms, diagnosis and management. Orthop Res Rev 2020;12:75-87.
- Kiel J, Taqi M, Kaiser K. Acromioclavicular Joint Injury. In: StatPearls [Internet]. StatPearls Publishing; 2023.
- Nolte PC, Lacheta L, Dekker TJ, et al. Optimal management of acromioclavicular dislocation: Current perspectives. Orthop Res Rev 2020;12:27-44.
- Phadke A, Bakti N, Bawale R, Singh B. Current concepts in management of ACJ injuries. J Clin Orthop Trauma 2019;10:480-485.
- Tamaoki MJ, Lenza M, Matsunaga FT, et al. Surgical versus conservative interventions for treating acromioclavicular dislocation of the shoulder in adults. Cochrane Database Syst Rev 2019;10:CD007429.
- Jeong JY, Chun YM. Treatment of acute high-grade acromioclavicular joint dislocation. Clin Shoulder Elb 2020;23:159-165.
- Abrams R, Akbarnia H. Shoulder Dislocations Overview. In: StatPearls [Internet]. StatPearls Publishing; 2023.
- Hasebroock AW, Brinkman J, Foster L, Bowens JP. Management of primary anterior shoulder dislocations: A narrative review. Sports Med Open 2019;5:31.
- Pak T, Kim AM. Anterior Glenohumeral Joint Dislocation. In: StatPearls [Internet]. StatPearls Publishing; 2023.
- Braun C, McRobert CJ. Conservative management following closed reduction of traumatic anterior dislocation of the shoulder. Cochrane Database Syst Rev 2019;5:CD004962.
- Wang SI. Management of the first-time traumatic anterior shoulder dislocation. Clin Shoulder Elb 2018;21:169-175.
- Kammel KR, El Bitar Y, Leber EH. Posterior shoulder dislocations. In StatPearls [Internet]. StatPearls Publishing; 2023.
- Paparoidamis G, Iliopoulos E, Narvani AA, et al. Posterior shoulder fracture-dislocation: A systematic review of the literature and current aspects of management. Chin J Traumatol 2021;24:18-24.
- Kammel KR, Leber EH. Inferior Shoulder Dislocations. In: StatPearls [Internet]. StatPearls Publishing; 2023.
- Halvorson JJ, Lamothe J, Martin CR, et al. Combined acetabulum and pelvic ring injuries. J Am Acad Orthop Surg 2014;22:304-314.
- Atallah HY. Pelvis. In: Sherman SC, ed. Simon’s Emergency Orthopedics, 8e. McGraw-Hill Education; 2019.
- Balogh Z, King KL, Mackay P, et al. The epidemiology of pelvic ring fractures: A population-based study. J Trauma 2007;63:1066-1073; discussion 1072-1063.
- Giannoudis PV, Grotz MR, Tzioupis C, et al. Prevalence of pelvic fractures, associated injuries, and mortality: The United Kingdom perspective. J Trauma 2007;63:875-883.
- Porter SE, Schroeder AC, Dzugan SS, et al. Acetabular fracture patterns and their associated injuries. J Orthop Trauma 2008;22:165-170.
- Burgess AR, Eastridge BJ, Young JW, et al. Pelvic ring disruptions: Effective classification system and treatment protocols. J Trauma 1990;30:848-856.
- Coccolini F, Stahel PF, Montori G, et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg 2017;12:5.
- MacLeod M, Powell JN. Evaluation of pelvic fractures. Clinical and radiologic. Orthop Clin North Am 1997;28:299-319.
- Henry S. Advanced Trauma Life Support (ATLS) Student Manual. 10th ed. American College of Surgeons; 2018.
- Marchand LS, Sepehri A, Hannan ZD, et al. Pelvic ring injury mortality: Are we getting better? J Orthop Trauma 2022;36:81-86.
- Kleweno CP, Maier RV. Pelvic ring resuscitation pathways. J Orthop Trauma 2022;36:294-297.
- Walsh M, Fritz S, Hake D, et al. Targeted thromboelastographic (TEG) blood component and pharmacologic hemostatic therapy in traumatic and acquired coagulopathy. Curr Drug Targets 2016;17:954-970.
- Magee GA, Fox CJ, Moore EE. Resuscitative endovascular balloon occlusion of the aorta in pelvic ring fractures: The Denver Health protocol. Injury 2021;52:2702-2706.
- Tomberg S, Heare A. Pelvic trauma: Initial evaluation and management. UpToDate. Updated Oct. 27, 2023.
- Barclay-Buchanan CJ, Barton MA. Pelvis Injuries. In: Tintinalli JE, Ma OJ, Yealy DM, et al., eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw-Hill Education; 2020.
- Poole GV, Ward EF. Causes of mortality in patients with pelvic fractures. Orthopedics 1994;17:691-696.
- Montero-Odasso MM, Kamkar N, Pieruccini-Faria F, et al. Evaluation of clinical practice guidelines on fall prevention and management for older adults: A systematic review. JAMA Netw Open 2021;4:e2138911.
- Giversen IM. Time trends of mortality after first hip fractures. Osteoporos Int 2007;18:721-732.
- Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 2006;17:1726-1733.
- Koval KJ, Aharonoff GB, Rokito AS, et al. Patients with femoral neck and intertrochanteric fractures. Are they the same? Clin Orthop Relat Res 1996;330:166-172.
- Griffiths R, Babu S, Dixon P, et al. Guideline for the management of hip fractures 2020: Guideline by the Association of Anaesthetists. Anaesthesia 2021;76:225-237.
- Kolodychuk N, Krebs JC, Stenberg R, et al. Fascia iliaca blocks performed in the emergency department decrease opioid consumption and length of stay in patients with hip fracture. J Orthop Trauma 2022;36:142-146.
- Giza E, Mithöfer K, Matthews H, Vrahas M. Hip fracture-dislocation in football: A report of two cases and review of the literature. Br J Sports Med 2004;38:E17.
- Pallia CS, Scott RE, Chao DJ. Traumatic hip dislocation in athletes. Curr Sports Med Rep 2002;1:338-345.
- Dawson-Amoah K, Raszewski J, Duplantier N, Waddell BS. Dislocation of the hip: A review of types, causes, and treatment. Ochsner J 2018;18:242-252.
- Marecek GS, Routt ML Jr. Percutaneous manipulation of intra-articular debris after fracture-dislocation of the femoral head or acetabulum. Orthopedics 2014;37:603-606.
- Asghar FA, Karunakar MA. Femoral head fractures: Diagnosis, management, and complications. Orthop Clin North Am 2004;35:463-472.
- Gangavalli AK, Nwachuku CO. Management of distal femur fractures in adults: An overview of options. Orthop Clin North Am 2016;47:85-96.
- Gwathmey FW Jr, Jones-Quaidoo SM, Kahler D, et al. Distal femoral fractures: Current concepts. J Am Acad Orthop Surg 2010;18:597-607.
- Von Keudell A, Shoji K, Nasr M, et al. Treatment options for distal femur fractures. J Orthop Trauma 2016;30(Suppl 2):S25-S27.
- Weinberg DS, Scarcella NR, Napora JK, Vallier HA. Can vascular injury be appropriately assessed with physical examination after knee dislocation? Clin Orthop Relat Res 2016;474:1453-1458.
- Kfuri M, Schatzker J. Revisiting the Schatzker classification of tibial plateau fractures. Injury 2018;49:2252-2263.
- Raschke MJ, Kittl C, Domnick C. Partial proximal tibia fractures. EFORT Open Rev 2017;2:241-249.
- Prat-Fabregat S, Camacho-Carrasco P. Treatment strategy for tibial plateau fractures: An update. EFORT Open Rev 2017;1:225-232.
- Aderinto J, Walmsley P, Keating JF. Fractures of the tibial spine: Epidemiology and outcome. Knee 2008;15:164-167.
- Howells NR, Brunton LR, Robinson J, et al. Acute knee dislocation: An evidence based approach to the management of the multiligament injured knee. Injury 2011;42:1198-1204.
- Sekiya JK, Kuhn JE. Instability of the proximal tibiofibular joint. J Am Acad Orthop Surg 2003;11:120-128.
- Sayum Filho J, Lenza M, Tamaoki MJ, et al. Interventions for treating fractures of the patella in adults. Cochrane Database Syst Rev 2021;2:CD009651.
- Bulgheroni E, Vasso M, Losco M, et al. Management of the first patellar dislocation: A narrative review. Joints 2019;7:107-114.
- Okoye M, Wissman A, Wissman RD. Review of extensor mechanism injuries in the dislocated knee. J Knee Surg 2022;35:498-501.
- Tandogan RN, Terzi E, Gomez-Barrena E, et al. Extensor mechanism ruptures. EFORT Open Rev 2022;7:384-395.
- McKinney B, Cherney S, Penna J. Intra-articular knee injuries in patients with knee extensor mechanism ruptures. Knee Surg Sports Traumatol Arthrosc 2008;16:633-638.
- Boublik M, Schlegel TF, Koonce RC, et al. Quadriceps tendon injuries in national football league players. Am J Sports Med 2013;41:1841-1846.
- Matava MJ. Patellar tendon ruptures. J Am Acad Orthop Surg 1996;4:287-296.
- Hsu H, Siwiec RM. Patellar Tendon Rupture. In: StatPearls [Internet]. StatPearls Publishing; 2023 Jan–.
Major orthopedic trauma is a common issue for the emergency medicine provider. Being able to make a timely diagnosis and optimize care improves patient outcomes.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
