How Do the Rhythm and 12-Lead Go Together?
By Ken Grauer, MD
Professor Emeritus in Family Medicine, College of Medicine, University of Florida
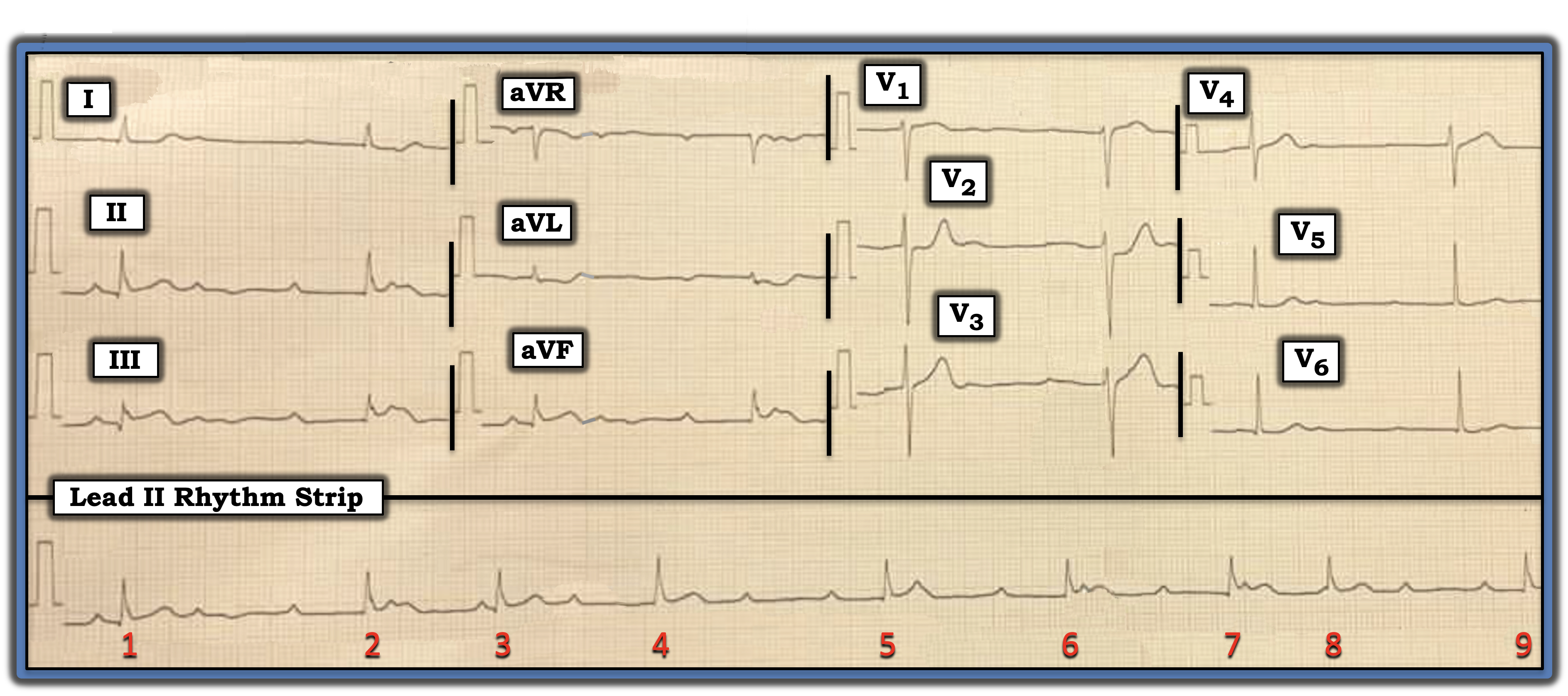
The patient whose electrocardiogram (ECG) is shown below presented for care because of chest pain. Looking at this ECG, can you determine why?
Interpretation: I favor looking first at the rhythm for a brief moment before I turn my attention to the 12-lead tracing. To emphasize that, in this initial look at the rhythm, I do not necessarily need to come up with a precise interpretation. This tip is especially helpful in today’s case because assessment of ST-T wave morphology is less reliable in leads in which the QRS complex is wide.
- The long lead II rhythm strip is remarkable for its bradycardia. The QRS complex is narrow, and it appears that there are regular upright P waves — many of which are not conducted. This suggests some significant degree of AV block.
- Despite the fact that the PR interval continually changes, this rhythm is unlikely to be complete (third-degree) AV block. This is because, most of the time, when the rhythm is third-degree AV block, the ventricular rate of the escape pacemaker will be regular.
As a result, I’m happy in my brief initial look at the rhythm to appreciate that there is some complex form of “high-grade” second-degree AV block — with marked bradycardia — and several places where consecutive sinus P waves are not conducted.
I next turn my attention to the 12-lead ECG:
- The key leads are III and aVF — both of which show subtle-but-real ST elevation with a hint of terminal T wave inversion. Given this finding in these two inferior leads, there is no doubt that, despite the tiny QRS amplitude in lead aVL, the mirror-image opposite ST-T wave shape in lead aVL compared to the ST-T wave shape in lead III constitutes enough of a reciprocal change in a patient with new chest pain to confirm acute inferior infarction until proven otherwise.
- Knowing that acute inferior myocardial infarction is so commonly associated with acute posterior involvement serves to next focus my attention on leads V2 and V3. Normally, there is slight, gently upsloping ST elevation in these two anterior leads. Therefore, the “shelf-like,” flattened ST segment accompanied by a taller-than-expected T wave in lead V2 immediately suggests associated posterior infarction until proven otherwise.
Bottom line: I favor looking first at the rhythm for a brief moment before I turn my attention to the 12-lead tracing. To emphasize that, in this initial look at the rhythm, I do not necessarily need to come up with a precise interpretation.
To emphasize, the cardiac rhythm in today’s case is complex and defies rapid interpretation. That said, “Common things are common.” Acute inferior infarction commonly is associated with some form of AV Wenckebach conduction (especially when the QRS complex is narrow, as it is in today’s case).
Therefore, my “quick initial impression” of today’s tracing is that there is acute infero-postero infarction with some form of resultant high-grade second-degree Wenckebach. This patient is in need of prompt cardiac catheterization with percutaneous coronary intervention to restore flow to the occluded “culprit” artery.
Note: For more information about this case, visit https://tinyurl.com/KG-Blog-416.
The patient whose electrocardiogram (ECG) is shown presented for care because of chest pain. Looking at this ECG, can you determine why?
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
