Hemorrhage Control in Adult and Geriatric Trauma
March 1, 2023
Related Articles
-
Infectious Disease Updates
-
Noninferiority of Seven vs. 14 Days of Antibiotic Therapy for Bloodstream Infections
-
Parvovirus and Increasing Danger in Pregnancy and Sickle Cell Disease
-
Oseltamivir for Adults Hospitalized with Influenza: Earlier Is Better
-
Usefulness of Pyuria to Diagnose UTI in Children
AUTHORS
Creagh Boulger, MD, Professor of Emergency Medicine, Ohio State University Wexner Medical Center, Columbus
Whitney Briggs, DO, Emergency Medicine Resident, Ohio State University, College of Medicine, Columbus
PEER REVIEWER
Steven M. Winograd, MD, FACEP, Brookdale Hospital Emergency Department, Brooklyn, NY; Samaritan Hospital, Troy, NY
EXECUTIVE SUMMARY
- In the guidelines from the Eastern Association for the Surgery of Trauma (EAST), a lower threshold for trauma activation and a high level of care are recommended for geriatric trauma.
- Damage control resuscitation is a multifaceted method for hemorrhage control that includes mechanical hemostasis, limited crystalloid and artificial colloids, permissive hypotension, and balanced resuscitation.
- Tourniquets can provide simple, cost-effective, lifesaving care. While most data come from military use, newer studies also support the use of tourniquets in the civilian prehospital setting. Consideration should be given to certain rare potential complications, such as nerve palsies and ischemia.
- When placing a tourniquet, it is important to document a neurovascular exam prior to placement, as well as the time at which the tourniquet was placed.
- Some military studies suggest a limit of two hours for tourniquets, with take down of the device and assessment every two hours.
- Combat Gauze, Celox Gauze, and Chito Gauze are deemed safe and efficacious and, thus, are considered first-line recommended hemostatic agents by the Committee on Tactical Combat Casualty Care (CoTCCC). These agents should be packed into the wound, and the provider should apply three to five minutes minimum of direct pressure, followed by a pressure dressing.
- Pelvic fractures can be life-threatening, with mortality reported as ranging between 7.6% and 50% for open pelvic fractures. When an unstable pelvic fracture is suspected or diagnosed, Advanced Trauma Life Support (ATLS) guidelines advise the use of a pelvic circumferential compression device as a temporizing measure until definitive fixation can be achieved.
- Tranexamic acid (TXA) is a synthetic lysine analogue and competitive inhibitor of plasminogen. The EAST guidelines for damage control resuscitation conditionally recommend early TXA for the severely hemorrhaging trauma patient.
- The ATLS 10th edition identifies that resuscitation with greater than 1.5 L of crystalloid is associated with increased mortality and now recommends limiting crystalloid use to no more than 1 L during the initial resuscitation. Newer recommendations support earlier administration of blood products, including plasma and platelets in 1:1:1 ratios, to limit trauma-induced coagulopathy.
- Resuscitative endovascular balloon occlusion of the aorta (REBOA) shows promising outcomes in patients with abdominal hemorrhage, but ongoing research is needed to identify the most appropriate patient populations and clinical settings for its application.
Death from hemorrhage may be rapid and allows the acute care practitioner a limited time frame to make critical interventions. The approach has changed drastically, and the authors provide the current strategies available to minimize blood loss until definitive hemostasis may occur.
— Ann Dietrich, MD, Editor
Case Study
You are working in a single coverage, rural emergency department when a 70-year-old male presents after a motor vehicle collision with heart rate 103 bpm, blood pressure 80/p, evident bruising to his flank, and an unstable pelvis. A second patient presents from the same accident. She is a 20-year-old female with a crush injury, with heart rate 130 bpm, blood pressure 70/p, and a partial right upper extremity amputation. What injuries should be considered? What is the best way to stabilize these patients? What are current advances, pharmacologic and nonpharmacologic, to stabilize these patients? This article will discuss management strategies for hemorrhage control.
Introduction
Epidemiology
Trauma is a significant global health issue, leading to more than 4.6 million deaths annually worldwide.1 In the United States, unintentional injury is the primary cause of death in people ages 1 to 44 years, and the fourth leading cause of death overall.2 Death from hemorrhage often occurs rapidly, with a median time of two to three hours after presentation, and about 50% of these deaths occur within the first 24 hours.3,4,5 Many of these deaths are preventable. Early recognition of subtle but potentially significant hemorrhage, an understanding of the underlying physiology, and timely and appropriate use of resources can decrease morbidity and mortality. This has led to the development of a multimodal approach, called damage control resuscitation (DCR), with the goal of minimizing blood loss until definitive hemostasis may be achieved.6 Hemorrhage control in trauma has changed drastically over the last two decades, with better understanding of the physiologic changes from trauma and improved approaches to resuscitation.6 Crucial management begins in the prehospital setting.
Patient Population
Trauma is a unique disease process, since it often affects young and otherwise healthy individuals. However, trauma does not discriminate. Patients with a significant mechanism of injury, at the extremes of life (pediatrics and geriatrics), and with medical comorbidities and polypharmacy are at higher risk for hemorrhage, shock, and mortality.
Mechanism of Injury
The mechanism of injury is a useful screening tool to determine which patients may be at risk for significant hemorrhage. Advanced Trauma Life Support (ATLS) guidelines describe significant mechanisms of injury as falls from a critical height of 6 m (20 ft),7 high-energy deceleration impacts, and penetrating wounds.8 It is important to have a higher index of suspicion with these mechanisms to facilitate the early identification and management of potential injuries.
Blunt trauma can lead to occult injuries. A deceleration injury involves a difference in speed between fixed and non-fixed parts of the body, causing injuries such as liver and spleen lacerations and bowel damage. The most common organs injured in blunt trauma injuries are the spleen (40% to 55%), liver (35% to 45%), and small bowel (5% to 10%). There is a 15% incidence of retroperitoneal hematoma in patients who undergo laparotomy for blunt injury.8
Penetrating trauma leads to different types of injuries. Stab wounds and low-velocity gunshot wounds cause direct tissue damage with laceration and cutting. Stab wounds most commonly cause injury to the liver (40%), small bowel (30%), diaphragm (20%), and colon (15%).8 The type of weapon used in gunshot wounds can determine the type and degree of tissue injury. Explosive devices can cause combined blunt and penetrating damage.
Elderly Patients
The geriatric population is a high-risk group for trauma and is a group of patients that is estimated to grow to 69 million Americans over the age of 65 years by 2030.9 In the guidelines from the Eastern Association for the Surgery of Trauma (EAST), a lower threshold for trauma activation and a high level of care are recommended for geriatric trauma patients. This population is at increased risk for adverse outcomes after injury due to comorbidities, limited cardiovascular reserve, and general frailty. In a study by Calland et al, those patients with a base deficit of -6 mEq/L or less correlated with severe injury and significant mortality, up to 60% risk, compared to those with -5 mEq/L and with less than 23% mortality.10 Elderly patients frequently take anticoagulation and antiplatelet agents that increase the risk of hemorrhage; these iatrogenic coagulopathies should be recognized, evaluated, and corrected.10 For geriatric patients, data suggest that they are less likely to die if their care comes from a trauma center that serves a higher number of geriatric patients.9
Complications of Trauma
Trauma is a complex process. The injuries themselves often pose a significant risk to the patient. However, the complications associated with trauma can carry a significant increase in morbidity and mortality as well.
Hemorrhagic Shock
Hemorrhage is the most common cause of shock in trauma patients. Early detection and management of hemorrhagic shock is vital to survival. Multiple studies have been performed to determine early signs of hemorrhagic shock and predict the requirement of blood products. In severely injured patients, the lethal triad of acidosis, coagulopathy, and hypothermia worsens morbidity and mortality. No single vital sign or laboratory finding on its own can definitively diagnose shock.
Trauma-Induced Coagulopathy
One-third of patients with bleeding from trauma show signs of coagulopathy on admission to hospitals.5,11 Trauma-induced coagulopathy has been associated with blood product transfusion recommendations, with significant associated morbidity and mortality. Recent updates to existing protocols have been made to include 1:1 ratios of packed red blood cells to fresh frozen plasma and platelets. This appears to reduce the risk of trauma-induced coagulopathy.5,11 One systematic literature search done in 2019 compared whole blood transfusions with component therapy and found no evidence to support or reject whole blood over component therapy in adult trauma patients.12
Diagnostics
Hemodynamics: ATLS Classification of Blood Loss
The ATLS classification of hemorrhagic shock is a useful guide to quantify blood loss, but, interestingly, it has not been well validated.13 A retrospective review of trauma patients in the German trauma registry found decreased variability in ATLS shock classification when using base deficit as an additional indicator. The updated 10th edition of ATLS in the hemorrhagic shock classification table (see Table 1) now includes base deficit. Blood loss may be obvious in some patients, but even in these patients, vital signs and visualization of blood loss are not good estimates of hemorrhagic shock.14,15 New scoring systems to predict the extent of shock and injury have been developed. However, many of these are not practical for application in a timely fashion and none have taken hold as a new standard of care. In many disease processes, laboratory studies can be helpful in diagnosing and risk-stratifying patients. Unfortunately, because of the close proximity of most traumatic events to hospital presentation, laboratory studies and other diagnostics generally are not helpful in quickly risk-stratifying this population. The following sections briefly discuss a few studies and their utility and pitfalls.
Table 1. Classes of Hemorrhagic Shock |
||||
Estimated Volume of Blood Loss |
Vitals |
Mental Status |
Urine Output |
|
Class I Shock |
< 750 mL |
Heart rate < 100 bpm Normal blood pressure |
Normal |
> 30 mL/hr |
Class II Shock |
750 mL to 1,500 mL |
Heart rate 100-120 bpm Normal blood pressure |
Slight confusion |
20-30 mL/hr |
Class III Shock |
1,500 mL to 2,000 mL |
Heart rate 120-140 bpm Decreased blood pressure |
Anxious and confused |
< 20 mL/hr |
Class IV Shock |
> 2,000 mL |
Heart rate > 140 bpm Decreased blood pressure |
Agitated to lethargic |
Negligible |
Adapted from: American College of Surgeons Committee on Trauma. ATLS® Student Manual, 10th ed. American College of Surgeons; 2018. |
||||
End Tidal CO2
Low end-tidal CO2 (ETCO2), CO2 < 35, may be a novel early predictor for hemorrhagic shock and the need for massive transfusion. A study by Caputo et al demonstrated that nasal cannula ETCO2 had a negative association with lactate and was predictive of operative intervention in penetrating trauma patients.16 Low ETCO2 had strong association with standard indicators for shock and was predictive of patients meeting CAT+ (≥ 3 units of packed red blood cells/h) criteria in the first six hours after admission.
Hemoglobin and Hematocrit
In nontraumatic causes of hemorrhagic shock, hemoglobin and hematocrit often are used to assess severity of blood loss, ongoing hemorrhage, and response to treatment. However, in trauma patients, these values often are normal on initial presentation and may take hours to drop.17,18 Serial measurements of hematocrit have a high sensitivity for detecting ongoing blood loss.19 In a study by Bruns et al, an initial hemoglobin below 10 g/dL in the first 30 minutes of patient arrival was associated with a three times higher need for intervention.20
Base Deficit and Lactate
Base deficit and lactate are measures of perfusion. Both of these studies have been shown to correlate with mortality and adequacy of resuscitation.21,22 Elevated lactate levels at presentation have been shown to correlate to mortality in trauma patients.23 In addition, failure to clear lactate in the first 24 hours was shown to be a strong negative prognostic marker after injury.23 As previously mentioned, base deficit was added to the ATLS shock classification table in the most recent edition.8
Coagulation Markers
Standard laboratory evaluation of coagulation is the following: prothrombin time (PT), activated partial thromboplastin time, platelet counts, and fibrinogen. However, these tests only monitor the initiation of clot production and may appear normal despite the patient being coagulopathic. Viscoelastic hemostatic assays (VHA), such as thromboelastography (TEG) and rotational thromboelastometry (ROTEM), which promptly evaluate the entire clotting process, are newer and may be used to direct blood product resuscitation.24-26 Early amplitudes in the VHA, TEG, and ROTEM provide fast results, which is critical in the resuscitation of bleeding patients. Introducing the use of early amplitudes can reduce time to diagnosis of coagulopathy and may be used in TEG monitoring of trauma patients.27 The VHAs appear to show promise in tailoring resuscitation to the individual patient if they can have quick turnaround times and be cost effective. In 2020, the EAST published a new coagulopathy guideline conditionally recommending use of TEG/ROTEM to guide transfusions, especially when compared to traditional coagulation parameters, in adult trauma patients. They found that using TEG/ROTEM-guided transfusion practices led to fewer total blood products administered and reduction in mortality in trauma patients.28
Management
Damage control resuscitation (DCR) is a multifaceted method for hemorrhage control. This approach includes mechanical hemostasis, limited crystalloid and artificial colloids, permissive hypotension, and balanced resuscitation.6,29 This is a drastic change from 20 years ago, when trauma teams would infuse 20 to 30 liters of crystalloid, transfuse 10 units of red blood cells, and stay in the operating room to repair all injuries and close the fascia on all patients.30 Mortality was high, and survivors experienced coagulopathy, renal failure, abdominal compartment syndrome, wound complications, and acute respiratory distress syndrome.29,30 Many studies in the combat setting have advanced the literature about optimal trauma resuscitation and management. The main principles include:6
• avoid/reverse hypothermia;
• minimize blood loss and apply early hemorrhage control measures;
• target low-normal blood pressures before definitive hemostasis;
• minimize crystalloid administration;
• use massive transfusion protocol to ensure blood product is given in pre-specified ratio;
• avoid delays to surgical and/or angiographic hemostasis;
• obtain functional laboratory measures to guide resuscitation;
• give pharmacologic adjuncts to safely promote hemostasis.6
Prehospital
Hemorrhage in the field remains the leading preventable cause of death in combat and the second leading cause of death in the civilian setting.3-5 Patients with traumatic injuries are on the clock. While there is minimal evidence behind the historical “golden hour,” we know that patients with active hemorrhage who achieve hemostasis and receive definitive care sooner have better outcomes.31,32 Many of the principles described in the EAST guidelines, such as normothermia, hemorrhage control, and conservative fluid administration, can and should be initiated in the field to optimize conditions for the patient. The subsequent section will discuss means of hemostasis that can be started in the field.
Direct Pressure and Pressure Dressings
Direct pressure and pressure dressings often are the first line of defense in hemorrhage. This technique requires little to no resources and has been shown to be an effective and safe means of hemostasis for smaller wounds.33 Successful direct pressure usually involves irrigating the wound, identifying the bleeding vessel, and applying direct one- to two-finger manual compression of the region uninterrupted for five to 15 minutes.34 The downside of this technique is that the source is not always easily visualized, the method requires personnel available to attend only to that wound, and the technique is useful only for smaller wounds with a clear, single source. This technique can be combined with a pressure dressing, with or without hemostatic agents, and possible temporary closure. When applied, pressure dressings should not be bulky and should be tight enough to provide hemostasis while maintaining distal perfusion and sensation. If distal neurovascular status is compromised, the pressure dressing now begins to function as a tourniquet. Some commercial products are available for temporary wound hemostasis. Wound closure clamps essentially grab the wound edges, pull them together, and lock in place. Wound closure clips are placed on the wound margin, typically the scalp, to provide compression on the edges.
Extremity Trauma: Tourniquets
Exsanguination from extremity trauma is a preventable cause of death.35,36 Tourniquets have been well studied on the battlefield and found to have significant association with lives saved, leading to a policy of all military personnel carrying tourniquets.36 In 2009, Kragh et al published a prospective study that was conducted in Baghdad over seven months in 2006. They evaluated 2,838 injuries and admitted civilian and military casualties with major limb trauma. A total of 232 patients had 428 tourniquets applied to 309 limbs. Early tourniquet placement, prior to the onset of shock, was associated strongly with survival.36 Tourniquets serve as the standard of care for control of severe external hemorrhage in the military setting.37,38
Prehospital data on tourniquet use in the civilian setting has been limited and often only references blunt trauma patients. However, in 2019, an eight-year retrospective analysis of penetrating extremity trauma was studied at Level I trauma centers. A group of patients with prehospital tourniquets placed was compared to a matched group of patients without tourniquets. The tourniquet group was found to have a higher systolic blood pressure on arrival to the emergency department (ED), decreased need for blood products, and decreased rate of limb complications without evidence of major complications.39 Both the American College of Surgeons Committee on Trauma (ACS-COT) and the American College of Emergency Physicians (ACEP) recommend tourniquets in the setting of life-threatening extremity hemorrhage.40,41 If indicated, placement of a tourniquet before extrication and transport is advised whenever possible.
Tourniquets have a few varieties. The common categories are open or closed, and manual or pneumatic. Open tourniquets do not require the provider to fully cinch around a limb prior to engaging the tourniquet, and they come apart completely for placement around the limb. Pneumatic tourniquets tend to be more expensive than the manual versions. Despite these differences, most studies demonstrate similar hemostasis among the various models when applied properly.42,43 Multiple commercial tourniquets are available. Common items, such as belts, sheets, and other cords, may be used, but they are less efficient.44 Tourniquet placement should be maintained until definitive surgical management can be accomplished.29,41,45
When placing a tourniquet, it is important to document a neurovascular exam prior to placement, as well as the time at which the tourniquet was placed. Some military studies suggest a limit of two hours, with take down of the device and assessment every two hours.46 Other studies have shown limb viability up to six hours with tourniquet use.45 Additional tourniquets can be applied if the first did not achieve hemostasis. Once hemostasis has been achieved, the tourniquet should not be removed until definitive surgical management is possible.
Junctional Hemorrhage and Other Sites of Significant Blood Loss
Junctional hemorrhage is bleeding that occurs at the junction of an extremity with the abdomen and pelvis that cannot be controlled adequately by an extremity tourniquet.47 Four mechanical devices have been Food and Drug Administration (FDA)-approved for junctional hemorrhage, but they are not well studied. The Committee on Tactical Combat Casualty Care (CoTCCC) recommends three of the four devices.47 Another type of junctional hemorrhage control device also has been approved for axillary use. Meusnier et al evaluated the Combat Ready Clamp (CroC) compared to the SAM Junctional Tourniquet (SJT) for ease of use and complete interruption of popliteal flow. Both devices were equally effective in arterial occlusion, but the SJT was preferred by users for ease of application and had quicker “hemostasis” in this small study.48 In a study by Rall et al, the Abdominal Aortic and Junctional Tourniquet (AAJT) was able to increase mean arterial pressure (MAP) in hemorrhagic swine without any clear adverse consequences.49 These devices have been used and studied primarily in simulation and military settings. Many of these devices require assembly and can be very bulky to store and transport. Their broad applicability to the civilian setting has yet to be demonstrated.50
Hemostatic Agents
Since direct manual pressure and tourniquet application are not feasible for all types of injuries, multiple topical hemostatic agents have been developed. These hemostatic dressings can be classified by their mechanism of action: factor concentrators, mucoadhesives, and procoagulant supplementers.51 The FDA has approved a number of these agents.51 These agents are used widely but have not been validated or well studied. The benefit of these products is that they typically are compact and lightweight, making them easy to store and transport for both in-hospital and out-of-hospital use. Most of these agents have similar efficacies; however, they may be caustic to surrounding tissue. Combat Gauze, Celox Gauze, and Chito Gauze are the only ones deemed safe and efficacious and, thus, considered first-line recommended hemostatic agents by the CoTCCC.52-54 These agents should be packed into the wound, and the provider should apply three to five minutes minimum of direct pressure, followed by a pressure dressing.
In 2016, the CoTCCC also proposed the addition of XSTAT to its hemorrhage control guidelines. XSTAT is a radiopaque hemostatic sponge system that can be deployed into deep tracks of wounds. Currently it cannot be used on the neck or torso. It is in early phases of use and is fairly costly, but it could reduce the need for extremity tourniquets.9,55 At this time, there are no large studies looking at the use of XSTAT in the civilian population. Warriner et al examined its use in 10 civilian patients with penetrating trauma. It was able to effectively stop hemorrhage in nine of the patients.56
Unstable Pelvic Injuries: Binders
Pelvic fractures can be life-threatening, with mortality reported as ranging between 7.6% and 50% for open pelvic fractures.57 Pelvic injuries can be overlooked easily in normotensive trauma patients with distracting injuries. A retrospective cohort study that examined blunt trauma between August and December 2011 found a high proportion of missed fractures (31%).57 If pelvic instability exists or if the patient is persistently hypotensive without a clear source, pelvic binding with a pelvic circumferential compression device (PCCD) should be considered. Pelvic circumferential compression can provide tamponade by “closing” the pelvis and reducing the potential volume of the pelvis from nearly 6 L of potential space to 1 L to 2 L.58 (See Figures 1 and 2 for X-rays of pelvis before and after placement of a pelvic binder.)
Figure 1. Patient with APC2 Fracture |
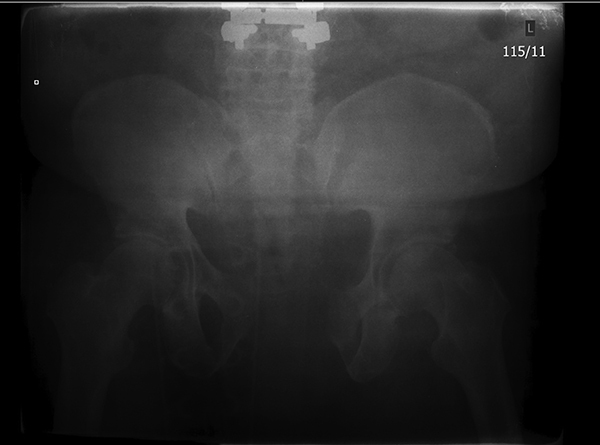 |
There is pubic diastasis of more than 2.5 cm and there is anterior widening of the SI joint. Source: Uzcategui M, Menaker J. Blunt pelvic trauma. Trauma Reports 2014;15:6. |
Figure 2. Patient with APC2 Fracture After Placement of a Pelvic Binder |
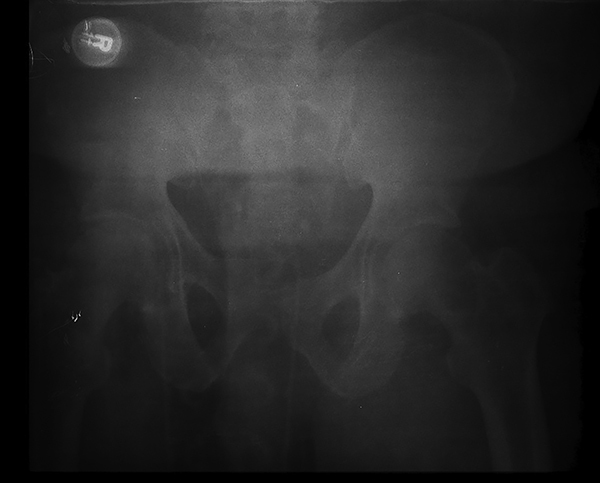 |
Placement of the pelvic binder with approximation and stabilization of the anterior and posterior elements, resulting in decreased pelvic volume. Source: Uzcategui M, Menaker J. Blunt pelvic trauma. Trauma Reports 2014;15:6. |
When an unstable pelvic fracture is suspected or diagnosed, ATLS guidelines advise the use of a PCCD as a temporizing measure until definitive fixation can be achieved.8 Several commercial products exist for these purposes, or a simple bedsheet can be used. Many studies indicate that when placed correctly, these various modalities have similar efficacies.59-63 Appropriate placement is crucial to efficacy. The PCCD should be placed at the level of the greater trochanter, not the abdomen, to optimize compression. In addition, efforts should be made to minimize friction and pressure points on the skin, since this can lead to skin breakdown and ulcerations.
Binders should be used only as temporizing measures until definitive hemostasis can be achieved, since prolonged use can cause skin breakdown and nerve damage.64 For pelvic injuries that continue to be hemodynamically unstable despite stabilization and closure, further invasive intervention should be implemented, such as external fixation, open fixation, or embolization. (See Figure 3.)
Figure 3. Internal Fixation of Pelvic Fracture |
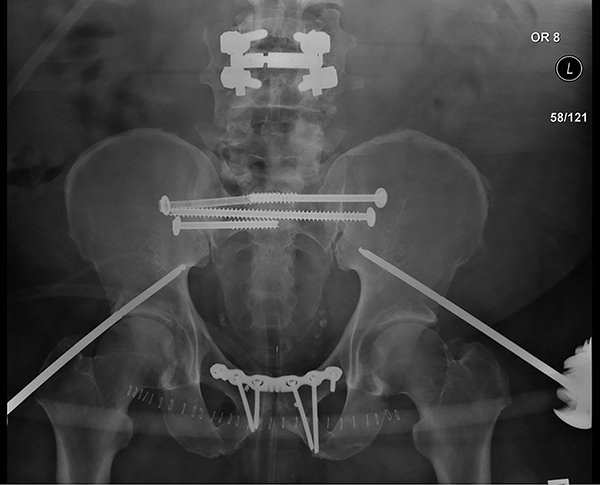 |
Patient originally stabilized with external fixation was bridged to definitive stabilization of the anterior and posterior elements with internal fixation. Source: Uzcategui M, Menaker J. Blunt pelvic trauma. Trauma Reports 2014;15:7. |
Definitive Hemostasis
To optimize care, patients should be transported to a hospital with trauma capabilities as soon as possible. The authors of a systematic review in 2006 showed a 15% reduction in mortality for patients treated in a trauma system, with a reported 50% decrease in preventable deaths.65 In addition to the aforementioned methods of hemorrhage control, which also can be applied in the hospital, once in the hospital, efforts should be made to expedite definitive surgical or angiographic management of bleeding.
In a study by Clarke et al, in hypotensive patients with isolated intra-abdominal injuries, the degree of hypotension and duration in the ED increased mortality by 1% for every three minutes in the ED. Meizoso et al studied hypotensive gunshot wound patients and found that delays greater than 10 minutes increased the likelihood of death by threefold, highlighting the crucial push to the operating room.66 To improve morbidity and mortality in the trauma patient, definitive surgery or angiography should not be delayed.
Non-Compressible Truncal Hemorrhage
Patients with non-compressible truncal hemorrhage (NCTH) have high mortality rates, from 18% to 50%, and are known to be at risk of imminent decompensation.67 These patients have limited bedside options for stabilization. One option is aortic occlusion (AO), which remains controversial for traumatic shock. The goal of AO is to preserve cerebral perfusion and coronary filling in life-threatening hypotension and hypovolemia due to hemorrhage in the chest.68 AO can be obtained in the more traditional method via a resuscitative thoracotomy or endovascularly. Resuscitative thoracotomy is achieved with a large open incision with aortic cross clamping. This technique typically is reserved for patients who have lost vital signs. This dramatic procedure has a poor survival rate of 0% to 15%.67
Comparing open approach, endovascular approach, and resuscitative thoracotomy, Chang et al conducted a multicenter, retrospective study of patients with NCTH. A total of 543 patients with NCTH were treated with open management (n = 309, 31%), endovascular management (n = 166, 31%), and resuscitative thoracotomy (n = 68, 12%). Mortality was 20%, 15%, and 79%, respectively.69 Endovascular management is recommended to be reserved for more hemodynamically stable patients, whereas open hemorrhage control is recommended for the unstable patient.
Resuscitative endovascular balloon occlusion of the aorta (REBOA) offers a less invasive alternative to open aortic occlusion.68,70-72 A retrospective case series by Moore et al between October 2011 and September 2015 examined 31 patients who underwent REBOA. A return to spontaneous circulation was observed in 60% of patients who had arrested prior to insertion (n = 10). After REBOA placement and balloon inflation, a significant increase in systolic blood pressure was observed in all patients with vital signs.67 The survival rate in this study was 32%.
In 2022, a prospective observational study conducted at six Level I trauma centers over 12 months looked at the use of REBOA in patients with evidence of hemorrhage below the diaphragm from both blunt and penetrating trauma. The study compared REBOA placement in Zone 1 (more proximal) and Zone 3 and found significant improvement in hemodynamics and a 59% rate of return of spontaneous circulation for patients in arrest. While encouraging, this study only looked at 75 total REBOA placements across these six trauma centers.73
The military has been using REBOA in the pre-hospital and austere setting with some success. Additionally, there is some evidence to support partial and intermittent occlusion techniques with REBOA to reduce complications such as distal ischemia. Ultimately, there are not sufficient data to guide consensus on the practice of REBOA use.74
Adjunctive Agents: Tranexamic Acid
The Clinical Randomization of Antifibrinolytic Therapy in Significant Haemorrhage (CRASH-2) trial was a randomized controlled trial that examined the administration of tranexamic acid (TXA) in 20,211 adult trauma patients.75,76 TXA is a synthetic lysine analogue and competitive inhibitor of plasminogen. At four weeks after injury, all-cause mortality was reduced by 1.5%. When TXA was administered between one and three hours of injury, mortality was reduced by 1.3%, whereas TXA administered after three hours increased risk of death by 1.3%.75,76 The EAST guidelines for DCR conditionally recommend early TXA for the severely hemorrhaging trauma patient.6 When TXA is administered prehospital, a follow-up infusion of TXA in the hospital is recommended (1 gram over eight hours).8
Conclusion
Early identification of massive hemorrhage is essential. Simple yet lifesaving interventions, such as good vascular access, tourniquet placement, and pelvic binding, should be used. Imaging and laboratory studies are of little use in the initial evaluation and management of the trauma patient in hemorrhagic shock. Hemorrhage is a significant cause of death in trauma patients. Many advances have changed the way trauma patients are managed, especially those in hemorrhagic shock. We have come full circle and returned to a more damage control-based system. Best practices for transfusion protocols and use of TXA have becomes more solidified in recent years. Use of TEG and ROTEM in guiding resuscitation have become more popular. Newer technology and devices such as XSTAT and REBOA, while ongoing research is needed to identify best practices, show promise in improving outcomes for trauma patients.
Case Conclusions
The 70-year-old male presents after a motor vehicle collision with heart rate 103 bpm, blood pressure 80/p, evident bruising to flank, and unstable pelvis.
What injuries should be considered? What is the best way to stabilize this patient?
His airway, breathing, and pulses in all four extremities are intact. The vital signs, tachycardia, and hypotension suggest significant hemorrhage, even though his heart rate is not extremely high. The unstable pelvis suggests a pelvic fracture. A pelvic binder should be placed to tamponade the pelvis and reduce the potential 6 L of blood loss down to 1 L to 2 L. The flank bruising suggests concern for a retroperitoneal bleed. If there is blood available immediately, this patient would benefit from trauma blood. If there is no blood, minimal crystalloid intravenous fluid should be given with the goal of systolic blood pressure of 80-90s.
In the elderly patient population, it important to ask about past medical problems, specifically if they are taking blood thinners. Reversal agents can be given to facilitate hemostasis.
Once in the hospital, there can be further evaluation of hemorrhage. In this case, the patient is fluid responsive. The Focused Assessment with Sonography for Trauma (FAST) exam reveals no free fluid in the abdomen. A computed tomography scan shows continued extravasation into the pelvis and retroperitoneal hemorrhage. Angiography is performed to stop the bleeding.
The second patient from the same accident is a 20-year-old female with a crush injury, with heart rate 130 bpm, blood pressure 70/p, and a partial right upper extremity amputation.
What injuries should be considered? What is the best way to stabilize this patient?
Her airway and breathing were intact at the scene. Her vital signs indicate significant hemorrhage. A tourniquet was placed proximal to the right upper extremity amputation site, but bleeding continued. Another tourniquet was placed with successful hemostasis. The time the tourniquet was placed was documented. This may be the source of her significant blood loss, but the mechanism and crush injury are concerning for internal hemorrhage. Beyond the tourniquet and initial fluid or blood resuscitation, her transfer to a trauma center should be expedited.
Her vital signs remain unstable on arrival. Despite initial blood and fluid, she remains hypotensive. Massive transfusion protocol is activated, with blood products being given in a 1:1:1 ratio of packed red blood cells to fresh frozen plasma to platelets through two large-bore IVs. The crush injury with bruising to her chest and abdomen is concerning for intraperitoneal hemorrhage. FAST reveals significant intraabdominal fluid in the right upper quadrant and left upper quadrant. With her persistent tachycardia and hypotension, she is taken emergently to the operating room for exploratory laparotomy for definitive management. A partial hepatectomy and splenectomy are performed, which stops the bleeding.
REFERENCES
- GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1151-1210.
- Centers for Disease Control and Prevention. 10 Leading Causes of Death by Age Group, United States – 2015. https://www.cdc.gov/injury/wisqars/pdf/leading_causes_of_death_by_age_group_2015-a.pdf
- Geeraedts LMG Jr, Kaasjager HAH, van Vugt AB, Frölke JPM. Exsanguination in trauma: A review of diagnostics and treatment options. Injury 2009;40:11-20.
- Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: The PROPPR randomized clinical trial. JAMA 2015;313:471-482.
- Chang R, Cardenas JC, Wade CE, Holcomb JB. Advances in the understanding of trauma-induced coagulopathy. Blood 2016;128:1043-1049.
- Cannon JW, Khan MA, Raja AS, et al. Damage control resuscitation in patients with severe traumatic hemorrhage: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 2017;82:605-617.
- Liu CC, Wang CY, Shih HC, et al. Prognostic factors for mortality following falls from height. Injury 2009;40:595-597.
- American College of Surgeons Committee on Trauma. Advanced Trauma Life Support (ATLS®) Student Manual. 10th ed. American College of Surgeons; 2018.
- Sims K, Montgomery HR, Dituro P, et al. Management of external hemorrhage in tactical combat casualty care: The adjunctive use of XStatTM compressed hemostatic sponges: TCCC Guidelines Change 15-03. J Spec Oper Med 2016;16:19-28.
- Calland JF, Ingraham AM, Martin N, et al. Evaluation and management of geriatric trauma: An Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg 2012;73(5 Suppl 4):S345-S350.
- Cohen MJ, Kutcher M, Redick B, et al. Clinical and mechanistic drivers of acute traumatic coagulopathy. J Trauma Acute Care Surg 2013;75(1 Suppl 1):S40-S47.
- Avery P, Morton S, Tucker H, et al. Whole blood transfusion versus component therapy in adult trauma patients with acute major haemorrhage. Emerg Med J 2020;37:370-378.
- Lawton LD, Roncal S, Leonard E, et al. The utility of Advanced Trauma Life Support (ATLS) clinical shock grading in assessment of trauma. Emerg Med J 2014;31:384-389.
- Mutschler M, Nienaber U, Brockamp T, et al. A critical reappraisal of the ATLS classification of hypovolaemic shock: Does it really reflect clinical reality? Resuscitation 2013;84:309-313.
- Guly HR, Bouamra O, Spiers M, et al. Vital signs and estimated blood loss in patients with major trauma: Testing the validity of the ATLS classification of hypovolaemic shock. Resuscitation 2011;82:556-559.
- Stone ME Jr, Kalata S, Liveris A, et al. End-tidal CO2 on admission is associated with hemorrhagic shock and predicts the need for massive transfusion as defined by the critical administration threshold: A pilot study. Injury 2017;48:51-57.
- Lamm RL, Coopersmith CM. Chapter 10. Hypovolemic and hemorrhagic shock. In: Roberts PR, Todd SR, eds. Comprehensive Critical Care: Adult. Society of Critical Care Medicine; 2012:183-198.
- Thorson CM, Van Haren RM, Ryan ML, et al. Admission hematocrit and transfusion requirements after trauma. J Am Coll Surg 2013;216:65-73.
- Zehtabchi S, Sinert R, Goldman M, et al. Diagnostic performance of serial haematocrit measurements in identifying major injury in adult trauma patients. Injury 2006;37:46-52.
- Bruns B, Lindsey M, Rowe K, et al. Hemoglobin drops within minutes of injuries and predicts need for an intervention to stop hemorrhage. J Trauma 2007;63:312-315.
- Davis JW, Mackersie RC, Holbrook TL, Hoyt DB. Base deficit as an indicator of significant abdominal injury. Ann Emerg Med 1991;20:842-844.
- Rutherford EJ, Morris JA Jr, Reed GW, Hall KS. Base deficit stratifies mortality and determines therapy. J Trauma 1992;33:417-423.
- Dezman ZD, Comer AC, Smith GS, et al. Failure to clear elevated lactate predicts 24-hour mortality in trauma patients. J Trauma Acute Care Surg 2015;79:580-585.
- Davenport R, Manson J, De’Ath H, et al. Functional definition and characterization of acute traumatic coagulopathy. Crit Care Med 2011;39:2652-2658.
- Prat NJ, Meyer AD, Ingalls NK, et al. Rotational thromboelastometry significantly optimizes transfusion practices for damage control resuscitation in combat casualties. J Trauma Acute Care Surg 2017;83:373-380.
- Baksaas-Aasen K, Gall L, Eaglestone S, et al. iTACTIC – implementing Treatment Algorithms for the Correction of Trauma-Induced Coagulopathy: Study protocol for a multicentre, randomized controlled trial. Trials 2017;18:486.
- Laursen TH, Meyer MAS, Meyer ASP, et al. Thrombelastography early amplitudes in bleeding and coagulopathic trauma patients: Results from a multicenter study. J Trauma Acute Care Surg 2018;84:334-341.
- [No authors listed]. Thromboelastography and rotational thromboelastometry in bleeding patients with coagulopathy: Practice management guideline from the Eastern Association for the Surgery of Trauma: Erratum. J Trauma Acute Care Surg 2021;90:766-767.
- Rossaint R, Bouillon B, Cerny V, et al. The European guideline on management of major bleeding and coagulopathy following trauma: Fourth edition. Crit Care 2016;20:100.
- Holcomb JB. Major scientific lessons learned in the trauma field over the last two decades. PloS Med 2017;14:4-7.
- Kauvar DS, Lefering R, Wade CE. Impact of hemorrhage on trauma outcome: An overview of epidemiology, clinical presentations, and therapeutic considerations. J Trauma 2006;60(6 Suppl):S3-S11.
- Malone DL, Dunne J, Tracy JK, et al. Blood transfusion, independent of shock severity, is associated with worse outcome in trauma. J Trauma 2003;54:898-907.
- Sharif MA, Wyatt MG. Vascular trauma. Surgery (Oxford International Edition) 2012;30:399-404.
- Park MJ, Gans I, Lin I, et al. Timing of forearm arterial repair in the well-perfused limb. Orthopedics 2014;37:e582-e586.
- Dorlac WC, DeBakey ME, Holcomb JB, et al. Mortality from isolated civilian penetrating extremity injury. J Trauma 2005;59:217-222.
- Kragh JF Jr, Walters TJ, Baer DG, et al. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg 2009;249:1-7.
- Schroll R, Smith A, McSwain NE Jr, et al. A multi-institutional analysis of prehospital tourniquet use. J Trauma Acute Care Surg 2015;79:10-14.
- Inaba K, Siboni S, Resnick S, et al. Tourniquet use for civilian extremity trauma. J Trauma Acute Care Surg 2015;79:232-237.
- Smith AA, Ochoa JE, Wong S, et al. Prehospital tourniquet use in penetrating extremity trauma: Decreased blood transfusions and limb complications. J Trauma Acute Care Surg 2019;86:43-51.
- Bulger EM, Snyder D, Schoelles K, et al. An evidence-based prehospital guideline for external hemorrhage control: American College of Surgeons Committee on Trauma. Prehosp Emerg Care 2014;18:163-173.
- American College of Emergency Physicians. Out-of-Hospital Severe Hemorrhage Control. Policy statement. Ann Emerg Med 2015;66:693.
- Gibson R, Housler GJ, Rush SC, et al. Preliminary comparison of new and established tactical tourniquets in a manikin hemorrhage model. J Spec Oper Med 2016;16:29-35.
- Gibson R, Aden JK 3rd, Dubick MA, Kragh JF Jr. Preliminary comparison of pneumatic models of tourniquet for prehospital control of limb bleeding in a manikin model. J Spec Oper Med 2016;16:21-27.
- Bequette BW, Kragh JF Jr, Aden JK Rd, Dubick MA. Belts evaluated as limb tourniquets: BELT study comparing trouser supporters used as medical devices in a manikin model of wound bleeding. Wilderness Environ Med 2017;28:84-93.
- Beekley AC, Sebesta JA, Blackbourne LH, et al. Prehospital tourniquet use in Operation Iraqi Freedom: Effect on hemorrhage control and outcomes. J Trauma 2008;64(2 Suppl):S28-S37.
- Dayan L, Zinmann C, Stahl S, Norman D. Complications associated with prolonged tourniquet application on the battlefield. Mil Med 2008;173:63-66.
- Kotwal RS, Butler FK Jr. Junctional hemorrhage control for tactical combat casualty care. Wilderness Environ Med 2017;28(2S):S33-S38.
- Meusnier JG, Dewar C, Mavrovi E, et al. Evaluation of two junctional tourniquets used on the battlefield: Combat Ready Clamp versus SAM junctional tourniquet. J Spec Oper Med 2016;16:41-46.
- Rall JM, Ross JD, Clemens MS, et al. Hemodynamic effects of the abdominal aortic and junctional tourniquet in a hemorrhagic swine model. J Surg Res 2017;212:159-166.
- van Oostendorp SE, Tan ECTH, Geeraedts LMG Jr. Prehospital control of life-threatening truncal and junctional haemorrhage is the ultimate challenge in optimizing trauma care; a review of treatment options and their applicability in the civilian trauma setting. Scand J Trauma Resusc Emerg Med 2016;24:110.
- Khoshmohabat H, Paydar S, Kazemi HM, Dalfardi B. Overview of agents used for emergency hemostasis. Trauma Mon 2016;21:e26023.
- Bennett BL, Littlejohn LF, Kheirabadi BS, et al. Management of external hemorrhage in tactical combat casualty care: Chitosan-based hemostatic gauze dressings—TCCC Guidelines-Change 13-05. J Spec Oper Med 2014;14:40-57.
- Butler FK Jr, Blackbourne LH, Gross K. The Combat Medic Aid Bag: 2025. CoTCCC Top 10 Recommended Battlefield Trauma Care Research, Development, and Evaluation Priorities for 2015. J Spec Oper Med 2015;15:7-19.
- Holcomb JB, Butler FK, Rhee P. Hemorrhage control devices: Tourniquets and hemostatic dressings. Bull Am Coll Surg 2015;100(1 Suppl):66-70.
- Kragh JF Jr, Aden JK, Steinbaugh J, et al. Gauze vs XSTAT in wound packing for hemorrhage control. Am J Emerg Med 2015;33:974-976.
- Rodriguez MI, Jensen JT, Gregory K, et al. A novel tamponade agent for management of post partum hemorrhage: Adaptation of the Xstat mini-sponge applicator for obstetric use. BMC Pregnancy Childbirth 2017;17:187.
- Yong E, Vasireddy A, Pavitt A, et al. Pre-hospital pelvic girdle injury: Improving diagnostic accuracy in a physician-led trauma service. Injury 2016;47:383-388.
- Ghaemmaghami V, Sperry J, Gunst M, et al. Effects of early use of external pelvic compression on transfusion requirements and mortality in pelvic fractures. Am J Surg 2007;194:720-723.
- Vaidya R, Roth M, Zarling B, et al. Application of circumferential compression device (binder) in pelvic injuries: Room for improvement. West J Emerg Med 2016;17:766-774.
- Chesser TJS, Cross AM, Ward AJ. The use of pelvic binders in the emergent management of potential pelvic trauma. Injury 2012;43:667-669.
- Bonner TJ, Eardley WG, Newell N, et al. Accurate placement of a pelvic binder improves reduction of unstable fractures of the pelvic ring. J Bone Joint Surg Br 2011;93:1524-1528.
- Mallinson T. Alternative improvised pelvic binder. African J Emerg Med 2013;3:195-196.
- Pizanis A, Pohlemann T, Burkhardt M, et al. Emergency stabilization of the pelvic ring: Clinical comparison between three different techniques. Injury 2013;44:1760-1764.
- Jain S, Bleibleh S, Marciniak J, Pace A. A national survey of United Kingdom trauma units on the use of pelvic binders. Int Orthop 2013;37:1335-1339.
- Celso B, Tepas J, Langland-Orban B, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma 2006;60:371-378.
- Meizoso JP, Ray JJ, Karcutskie CA 4th, et al. Effect of time to operation on mortality for hypotensive patients with gunshot wounds to the torso: The golden 10 minutes. J Trauma Acute Care Surg 2016;81:685-691.
- Moore LJ, Martin CD, Harvin JA, et al. Resuscitative endovascular balloon occlusion of the aorta for control of noncompressible truncal hemorrhage in the abdomen and pelvis. Am J Surg 2016;212:1222-1230.
- DuBose JJ, Scalea TM, Brenner M, et al. The AAST prospective Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry: Data on contemporary utilization and outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA). J Trauma Acute Care Surg 2016;81:409-419.
- Chang R, Fox EE, Greene TJ, et al. Multicenter retrospective study of noncompressible torso hemorrhage: Anatomic locations of bleeding and comparison of endovascular versus open approach. J Trauma Acute Care Surg 2017;83:11-18.
- Napolitano LM. Resuscitative endovascular balloon occlusion of the aorta: Indications, outcomes, and training. Crit Care Clin 2017;33:55-70.
- Brenner M, Teeter W, Hoehn M, et al. Use of resuscitative endovascular balloon occlusion of the aorta for proximal aortic control in patients with severe hemorrhage and arrest. JAMA Surg 2018;153:130-135.
- Aso S, Matsui H, Fushimi K, Yasunaga H. Resuscitative endovascular balloon occlusion of the aorta or resuscitative thoracotomy with aortic clamping for noncompressible torso hemorrhage: A retrospective nationwide study. J Trauma Acute Care Surg 2017;82:910-914.
- Moore LJ, Fox EE, Meyer DE, et al. Prospective observational evaluation of the ER-REBOA catheter at 6 U.S. trauma centers. Ann Surg 2022;275:e520-e526.
- Cannon J, Morrison J, Lauer C, et al. Resuscitative endovascular balloon occlusion of the aorta (REBOA) for hemorrhagic shock. Mil Med 2018;183(suppl_2):55-59.
- Roberts I, Shakur H, Coats T, et al. The CRASH-2 trial: A randomised controlled trial and economic evaluation of the effects of tranexamic acid on death, vascular occlusive events and transfusion requirement in bleeding trauma patients. Health Technol Assess 2013;17:1-80.
- CRASH-2 collaborators; Roberts I, Shakur H, Afolabi A, et al. The importance of early treatment with tranexamic acid in bleeding trauma patients: An exploratory analysis of the CRASH-2 randomised controlled trial. Lancet 2011;377:1096-1101, 1101.e1-1101.e2.
