By Ken Grauer, MD
The electrocardiogram (ECG) in the figure was obtained from a man in his 60s who presented to the emergency department for a suspected kidney stone. The patient also noted some intermittent heartburn in recent weeks.
- How would you interpret his ECG?
- Should you activate the cath lab?
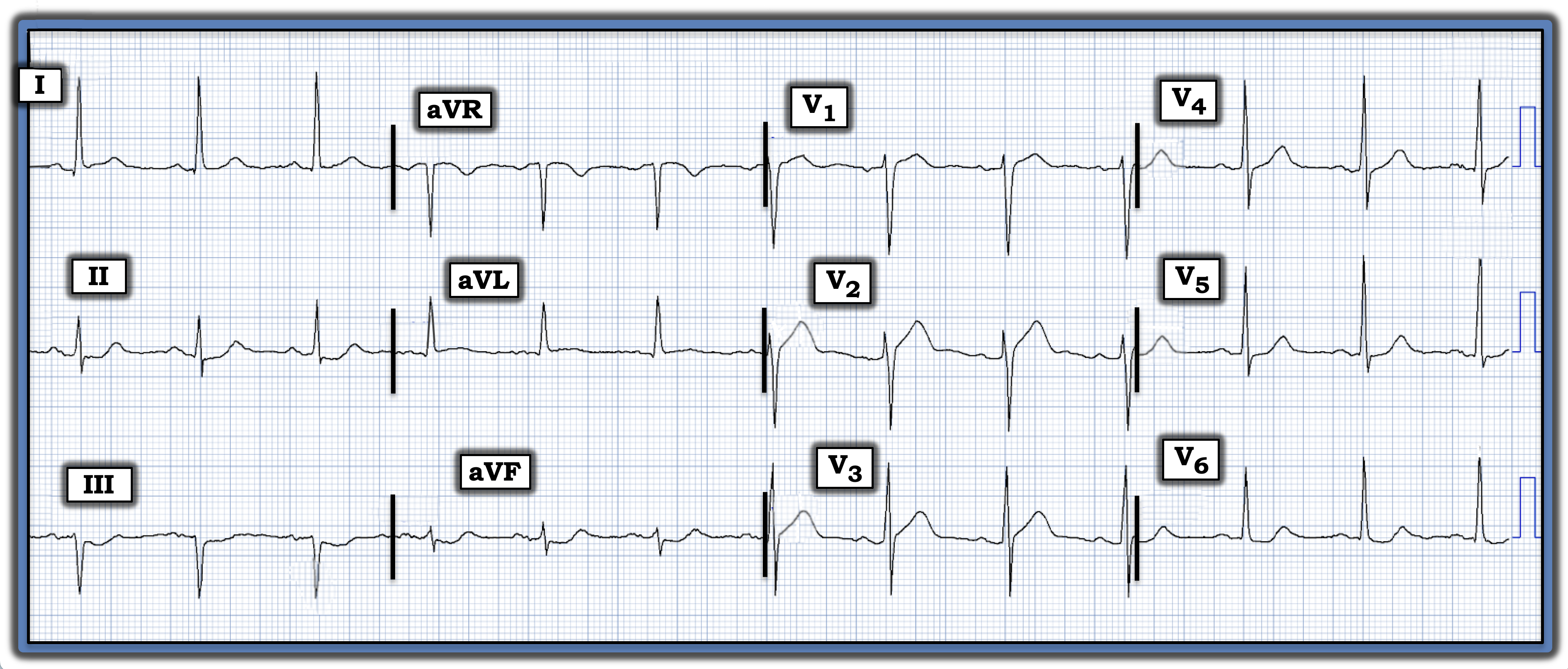
Interpretation: The ECG in the figure shows a normal sinus rhythm with normal intervals (PR, QRS, QTc), slight left axis deviation, and no sign of chamber enlargement. There are no significant Q waves, and R wave progression is normal (with transition to a predominant R wave already occurring by lead V3). That said, although the criteria for an ST elevation myocardial infarction are not satisfied, this ECG is very concerning.
- The lead that immediately drew my attention was lead V2. Whereas there normally often will be a slight amount of gently upsloping ST elevation in both leads V2 and V3, the ST segment takeoff in V2 is much straighter than normal, with more than the usual amount of J-point ST elevation.
- Neighboring leads V1 and V3 also each manifest abnormal ST segment straightening.
- In support of these anterior lead findings being “real” is the reciprocal ST depression in each of the inferior leads (with terminal T wave positivity in leads II and aVF) — and subtle-but-real ST coving and elevation in lead aVL.
- Lastly, there is ST segment flattening with slight depression in lateral chest leads V5 and V6.
Not all patients with acute myocardial infarction have chest pain. Some such patients have no symptoms at all in association with their acute myocardial infarction, whereas others have a non-chest pain equivalent symptom, such as shortness of breath, fatigue, flu-like syndrome, mental status change, or gastrointestinal discomfort, such as “heartburn.”
- Especially given the history in today’s case of heartburn — I would be concerned about an ongoing acute event, most likely acute proximal left anterior descending (LAD) coronary artery occlusion.
- While the cardiologist on call might not want to activate the cath lab on the basis of this single ECG, searching for a previous tracing on this patient for comparison, ordering serial troponin tests, and repeating the ECG (ideally within 10-30 minutes) would be in order.
Follow-Up: Cardiac catheterization ultimately was performed on today’s patient, and it revealed multi-vessel disease with “culprit” lesions in both the proximal LAD and the first diagonal branch of the LAD.
- Unfortunately, the cardiac catheter was delayed for almost seven hours. Had the treating providers recognized the described, potentially acute changes on the initial ECG, cardiac catheterization and percutaneous coronary intervention could have been performed much sooner.
Note: For more information about this case, visit https://tinyurl.com/KG-Blog-423.

