AUTHORS
Jessica Zhen, MD, Attending Emergency Medicine Physician USAF, MC, Wright Patterson AFB, OH; Core Faculty Member, Emergency Medicine Residency WPAFB/Wright State University Boonshoft School of Medicine, Dayton, OH
Jordan Hickey, MD, Resident Emergency Medicine Physician, Wright State University Boonshoft School of Medicine, Dayton, OH
PEER REVIEWER
Steven M. Winograd, MD, FACEP,Attending Emergency Physician, Keller Army Community Hospital, West Point, NY
Executive Summary
- Ancillary testing in hyperglycemic emergencies includes tests of metabolic state and investigations for triggering events.
- The severity of diabetic ketoacidosis (DKA) is categorized by serum pH, serum bicarbonate level, and mental status.
- End-tidal carbon dioxide (ETCO2) can be used to assess for the expected respiratory alkalosis seen with DKA in hyperglycemic patients; an ETCO2 above 35 mmHg excludes the presence of DKA and an ETCO2 below 21 mmHg is diagnostic of DKA.
- The treatment priorities of DKA are fluid resuscitation to address dehydration and improve tissue perfusion, correcting electrolyte abnormalities, correcting acidosis, and correcting hyperglycemia.
- Insulin therapy corrects the hyperglycemia more quickly than it resolves the ketoacidosis in DKA, so intravenous dextrose infusion is required during insulin infusion once serum glucose reaches 250 mg/dL.
- There is no evidence to support the use of intravenous sodium bicarbonate to treat DKA.
- Fluid and insulin treatment of hyperosmolar hyperglycemic syndrome typically is done at slower rates than in DKA to maintain changes in serum osmolality at < 3 mOsm/kg per hour.
- Treat awake and alert hypoglycemic patients with oral carbohydrates, using pure glucose for patients on alpha glucosidase inhibitors.
This issue concludes our two-part discussion of diabetic emergencies. Part I covered pathophysiology and clinical presentation, and part II will cover diagnostic evaluation and management.
— Joseph Stephan Stapczynski, MD, Editor
Diagnostic Studies
Most adult patients presenting the emergency department (ED) with diabetic ketoacidosis (DKA), hyperosmolar hyperglycemic syndrome (HHS), or euglycemic diabetic ketoacidosis (EDKA) will be ill, as mentioned in part I, and likely will have a known diagnosis of diabetes. Often, they will have had elevated glucose readings on home glucometers or admit to nonadherence with insulin regimens. Histories such as this streamline the diagnostic workup for hyperglycemia, acidosis, and electrolyte abnormalities. However, even in adults, especially with the rising incidence of prediabetes and diabetes, it is possible that one of these emergencies is the initial presentation of diabetes, and without that known, ordering the studies for this complication is not as obvious. Patients also may present altered or obtunded or without access to records or medication information.
Confirming DKA, HHS, or EDKA with laboratory studies is only part of the puzzle; while it will help guide therapy and disposition, there often is an underlying trigger that needs to be diagnosed and addressed to fully treat the patient. These triggers may have associated metabolic derangements and organ abnormalities that also must be evaluated and monitored. Similarly, associated trauma is not uncommon, either as a trigger for the diabetic emergency or as a result, and should be considered. Most often, a broad laboratory and diagnostic workup is essential to fully diagnose, treat, and monitor these patients appropriately. (See Table 1.)
Table 1. Diagnostic Evaluation |
Essential Studies
Considerations To Identify Triggering Events
|
Diabetic Ketoacidosis
In DKA, the hyperglycemia typically is in the 300 mg/dL to 500 mg/dL range, venous blood gas (VBG) will show the metabolic acidosis with a compensatory respiratory alkalosis, and serum bicarbonate will be decreased.1 Ketones will be present on urinalysis, but serum testing specifically for beta hydroxybutyrate also should be performed for quantitative measurement. Beta hydroxybutyrate is the most common ketone and is produced in a much higher ratio than acetoacetate, a ratio that continues to increase with worsening DKA. In addition, serum beta hydroxybutyrate levels > 3.8 mmol/L have high specificity and sensitivity for the diagnosis of DKA.1
As mentioned previously, DKA is associated with several electrolyte abnormalities: pseudohyponatremia and a normal or elevated serum potassium level despite overall low total body potassium. A similar situation occurs with phosphate where the total body level is low because of insulin deficiency and metabolic acidosis, but the serum levels are normal until they fall due to intracellular shifts occurring with insulin and fluid treatment.1 Other laboratory findings include leukocytosis usually in the range of 10,000 cells/μL to 15,000 cells/μL, likely stress-induced from excess cortisol, catecholamines, and pro-inflammatory cytokines. However, if the white blood cell (WBC) count is > 25,000 cells/μL or with > 10% bands, it suggests ongoing infection.1,2 Other laboratory findings that are common in DKA are elevated lipase despite the lack of intraabdominal pathology and elevated triglycerides. The hemoglobin A1c (HbA1c) level can help differentiate chronic hyperglycemia of uncontrolled diabetes from acute metabolic decompensation from someone who previously had well-controlled diabetes.2
The American Diabetes Association (ADA) categorizes DKA in adults into one of three stages of severity:3
• Mild: blood pH mildly decreased between 7.25-7.30, serum bicarbonate decreased to 15 mmol/L to 18 mmol/L, and the patient is alert;
• Moderate: blood pH 7.00-7.25, serum bicarbonate decreased to 10 mmol/L to 15 mmol/L, and mild drowsiness may be present;
• Severe: blood pH below 7.00, serum bicarbonate decreased below 10 mmol/L, and stupor or coma may be present.
An interesting and easy yet underused method to assist in the diagnosis of DKA is end-tidal carbon dioxide (ETCO2) monitoring/capnography. Typically, a VBG or arterial blood gas (ABG) is performed to confirm metabolic acidosis, which is one of the diagnostic criteria for DKA. However, these tests are reliant on laboratory turnaround, which can be frustratingly slow if the patient is requiring critical interventions. Therefore, ETCO2 can be used as a proxy for the PaCO2 portion of the ABG, since it has a direct relationship with arterial carbon dioxide and metabolic acidosis.4 In DKA, metabolic acidosis (decreased pH) ensues because of the presence of ketoacids and loss of bicarbonate. The body attempts to compensate by blowing off more carbon dioxide via increasing the minute ventilation to cause a respiratory alkalosis, which lowers ETCO2 measurements. Therefore, there is a linear correlation between the respiratory alkalosis seen in DKA and ETCO2. As acidosis worsens, serum pH decreases, bicarbonate decreases, and ETCO2 also decreases.1
For adult patients presenting to the ED with hyperglycemia (> 550 mg/dL) and a suspected diagnosis of DKA, studies have near 100% sensitivity in excluding the presence of metabolic acidosis with ETCO2 levels > 35 mmHg.1,4,5 In addition, the specificity nears 100% in identifying metabolic acidosis and DKA with ETCO2 levels < 21 mmHg.1,4,5 Capnography can serve as a very easy, quick, cheap, and noninvasive means to assess for metabolic acidosis in patients presenting to the ED with possible DKA. Furthermore, knowing the relationships between acidosis, bicarbonate, and ETCO2 measurements allows for easy continuous monitoring, noting clinical improvement or deterioration as well as response to treatments.
Hyperosmolar Hyperglycemic Syndrome
Profound hyperglycemia is likely one of the first and very striking features of HHS, since point-of-care (POC) testing usually will read just“high,” since serum glucose results often are > 1,000 mg/dL. The other important laboratory abnormality is the serum osmolality, which is always elevated in HHS, helping distinguish it from DKA. As discussed previously, this is because of an increased effective plasma osmolality; the substantial amount of glucose in the serum with largely electrolyte-free water output via osmotic diuresis increases the osmolality, which is exacerbated by impaired thirst mechanism and/or reduced access to water, allowing for normal or increased effective sodium and osmolality.6 HHS does not cause an osmolar gap, and if one is found, further studies should be done to find a source of the unmeasured anions. Of note, because of the significant degree of hyperglycemia, the correction factor of 2.4 mEq/L vs. 1.6 mEq/L for correction of pseudohyponatremia likely is more accurate.7 Similar to DKA, leukocytosis can be seen, as well as potassium derangements. Although it often is seen in DKA, kidney injury typically is associated with HHS.
The ADA includes the following as diagnostic features of HHS:3
• plasma glucose levels > 600 mg/dL;
• serum osmolality > 320 mOsm/kg;
• profound dehydration, up to an average of 9 L;
• serum pH > 7.30;
• serum bicarbonate > 15 mEq/L;
• absent to small ketonuria and absent to low ketonemia < 3 mmol/L;
• blood urea nitrogen (BUN) > 30 mg/dL;
• creatinine > 1.5 mg/dL;
• some alteration in consciousness.
Euglycemic Diabetic Ketoacidosis
What distinguishes EDKA from DKA is a normal glucose in the presence of the expected metabolic acidosis and ketosis; serum glucose will be < 250 mg/dL, pH will be < 7.3, serum bicarbonate will be < 18 mEq/L, and ketones will be present in blood and urine. As with the other hyperglycemic emergencies, there may be leukocytosis, but significant elevation should prompt investigation for concurrent infection. Potassium alterations occur as in DKA and HHS, with the propensity to appear normal despite overall total body depletion. Magnesium and phosphate often are low, potentially more so than in the other hyperglycemic conditions, since EDKA occurs in a starved state. On the other hand, while there may be mild hyponatremia, it generally is less severe than the pseudohyponatremia seen in profound hyperglycemic states.8
Hypoglycemia
A POC fingerstick glucose will diagnose hypoglycemia rapidly. As mentioned, a level < 70 mg/dL is considered low, but < 54 mg/dL is the clinically important level. However, it still is important to get a serum glucose value via a chemistry panel test. In patients with a history of diabetes who present symptomatic with documented low glucose, it likely is due to their medications, but a thorough history, physical examination, and laboratory workup should be conducted to rule out underlying triggers. Although outside the scope of this discussion, it is important to note that if hypoglycemia occurs in someone without diabetes, it is highly suspicious for pathology and a gamut of more unique testing must be performed to search for an underlying cause: insulin level, C-peptide level, proinsulin level, serum ketone levels, oral hypoglycemic agent screening, insulin antibody testing, glucose response to glucagon, imaging for insulinoma, and fasting workups.
Differential Diagnosis
In considering the differential diagnosis of diabetic emergencies, it is necessary not only to consider alternate pathologies regarding symptoms and initial laboratory findings, but once the diagnosis is made, it is important to create a differential regarding the inciting event for the emergency. The underlying causes have been discussed previously, and this section will focus on the differential diagnoses based on initial presentation and workup.
Hyperglycemic Emergencies
In evaluating a patient with a potential hyperglycemic emergency, it must be considered that it is not uncommon for patients presenting to the ED to have an initial elevated glucose on POC testing, but that does not always mean it is a contributing factor to their presenting symptoms. It could be high simply because of poor diabetes control, an undiagnosed diabetic condition (that is not necessarily an emergency), or the use of steroids. It is important to remember that glucose is regularly elevated in other causes of critical illness secondary to the release of stress hormones.9,10 As previously discussed, it is important to obtain essential laboratory values (e.g., pH, anion gap, plasma osmolality, ketones) to help differentiate among the various hyperglycemic emergencies. Particularly when there is concern for DKA and EDKA, other causes of ketosis and anion gap metabolic acidosis should be considered.9,11,12 (See Table 2.)
Table 2. Differential Diagnosis of Anion Gap Metabolic Acidosis |
|
Hypoglycemia
It is exceptionally important to obtain a POC glucose level promptly for any patients presenting with symptoms of hypoglycemia. It is an abnormality that must be discovered early, since it usually is easy to address quickly and stabilize while further workup is being obtained and before further damage occurs secondary to the neuroglucopenia. In particular, because neurological symptoms are so prevalent in hypoglycemia, it is a diagnosis that must be considered in every patient presenting with altered mental status or any focal neurological deficit, particularly if they have a known history of diabetes. Other causes of encephalopathy and neurological deficits should continue to be in the differential diagnosis, however, until the workup and full evaluation are completed, and it can be determined that hypoglycemia is the cause of symptoms and not the consequence of another pathology. (See Table 3.)
Table 3. Differential Diagnoses to Consider with Neurological Symptoms of Hypoglycemia11,39 |
|
Management
Similar to all presentations to the ED, the evaluation of hyperglycemic emergencies begins with a primary survey — airway, breathing, circulation, disability, and exposure — and intervening in these areas when necessary.
DKA
Even with only a brief evaluation and minimal information, such as hyperglycemia on a POC glucose, if there is a high suspicion for DKA, management should be initiated prior to receiving confirmatory laboratory tests.11 Overall, the management of DKA has the following goals:1,9,11,13-16
• fluid resuscitation to address dehydration and to improve hemodynamic stability and tissue perfusion;
• correcting electrolyte derangements;
• correcting acidosis;
• correcting hyperglycemia;
• identifying and treating the inciting event.
As with most dynamic pathologies, frequent and methodical reevaluation of patients is key in monitoring the effectiveness of and then adjusting the next steps of treatment. This includes repeat physical examination to assess for changes (e.g., mental status, circulation, breathing status, and accurate intake and output), as well as hourly POC glucose checks and repeat laboratory tests to monitor electrolytes, kidney function, and acid-base status.17,18
Fluid Resuscitation and Continuous Intravenous Fluids
While the extent of volume depletion can vary, it is typical that patients presenting with DKA can have a fluid deficit of ~100 mL/kg, which is approximately 4 L to 6 L, but it can be as high as 10 L.9,11,13,16 As such, the initial step in management should be obtaining intravenous (IV) access and administering fluids to replenish intravascular volume. This will allow for perfusion of organs, improving hemodynamic stability in patients with hypotension, decreasing insulin resistance, and working to decrease the levels of serum glucose and ketone levels.1,2,11,17-19
It is largely agreed upon that IV fluid administration is one of the cornerstones of DKA management, but there has been much academic debate regarding which fluids to choose and at what rate they should be given. Many protocols are based on the most recent ADA guidelines released in 2009 that recommend the initial use of a normal saline bolus at 15 mL/kg/hr to 20 mL/kg/hr.3,11,20 However, concerns have been raised for the use of sodium chloride infusions and their risk of causing a hyperchloremic metabolic acidosis, contributing to the already present acidosis and potentially prolonging its resolution.11,21,22 Several studies in the early 2010s investigated whether balanced electrolyte solutions (e.g., lactated Ringer’s) would be more beneficial in DKA resuscitation. And while they showed that balanced fluids may reduce the risk of developing hyperchloremic metabolic acidosis, no true benefit was found in the time that it took to normalize acid-base disturbances.23,24
However, more recently, a Phase II trial comparing 0.9% sodium chloride to Plasmalyte-148 (a buffered solution) demonstrated a shorter time to normalization of acid-base disturbances.25 Similarly, in 2020, a subgroup analysis was completed using two previous large randomized controlled trials that demonstrated a significant decrease in time of DKA resolution in patients who were given balanced electrolyte solutions when compared to those resuscitated with normal saline.26
That said, the most recently released society guidelines come from the Joint British Diabetes Societies in 2021, which continue to recommend normal saline as the fluid of choice in initial resuscitation.27 This is partially because of the logistical aspect that normal saline can be premixed with potassium chloride, another crucial aspect in the treatment of DKA that will be discussed later, rather than separately administering balanced solutions and potassium replacement. Nonetheless, despite current guidelines, the use of buffered solutions over normal saline may be considered on a case-by-case basis and as more research is completed, future guidelines may shift to recommending their use.
If the patient is hemodynamically unstable, they may require further fluid boluses until they begin to reach a more euvolemic state and blood pressure has stabilized.2 Otherwise, after the initial bolus, the adult patient can be switched to a maintenance infusion rate at 250 mL/hr to 500 mL/hr. In hyponatremic patients, it may be best to use normal saline, whereas if the patient is eunatremic or hypernatremic, half-normal saline should be used.1,11,13,16 (See Figure 1.)
Figure 1. Approach to Intravenous Fluids in the Management of Diabetic Ketoacidosis |
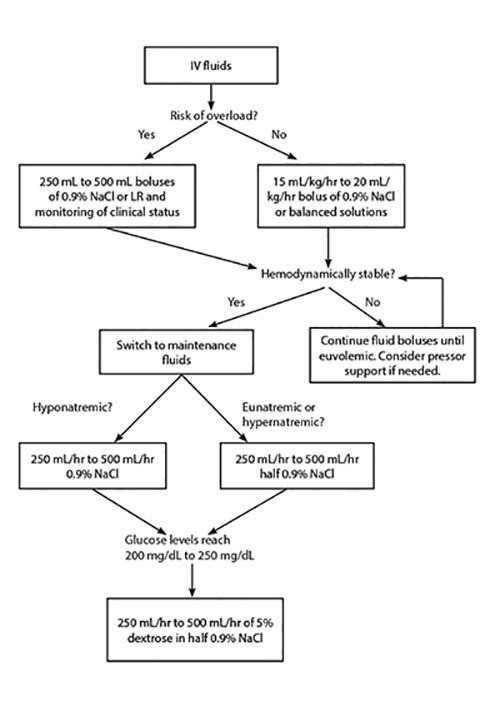 |
IV: intravenous; NaCl: sodium chloride; LR: lactated Ringer’s |
In most cases, glucose will normalize quicker than ketoacidosis. As such, because insulin administration is needed to resolve the ketoacidosis, its time of required use likely will exceed the time that it takes for glucose to normalize. Because of this, once glucose levels begin to approach 200 mg/dL to 250 mg/dL (different sources vary on this cutoff level), dextrose must be added to the IV fluids to allow for continued insulin administration and avoid hypoglycemia. This can be accomplished by switching fluids to 5% dextrose in half-normal saline.1,11,18,22,28
The approach to IV fluid administration described earlier often is referred to as a “one-bag” system, since the fluids are completely altered based on glucose levels, and only one IV is running at a time. Alternatively, there is the “two-bag” system that is not currently used regularly in the adult population but also is an option for management. Rather than entirely switching to IV fluids with a set amount of dextrose once a patient’s blood glucose levels reach a certain range, the two-bag system works to keep insulin and fluid infusion rates constant while titrating the amount of dextrose administration to blood glucose levels. In this method, the patient will have a consistent level of IV insulin being infused. Simultaneously, the patient would have two bags of IV fluids being administered, each with different compositions (one is half-normal saline and the other is 10% dextrose with half-normal saline), and the rate at which each is titrated is based on glucose levels to keep an overall constant rate of fluid infusion.15,29,30
This approach to DKA management has largely been studied only in pediatric populations, but several studies have demonstrated benefits that may be translatable to the adult population. For instance, various studies have shown a quicker bicarbonate, ketone, and pH correction; shorter stays in the pediatric intensive care unit (PICU); and a reduction in the length of time spent receiving insulin therapy.31-33 More recently, several studies have evaluated the two-bag system in adults. In 2017, a retrospective study showed the use of the two-bag system led to quicker closure of the anion gap and blood glucose levels when compared to the one-bag system.30 Similarly, a before-and-after implementation in an ED setting of a two-bag method protocol demonstrated a quicker resolution of acidosis, decreased duration of IV insulin, and decreased need for hospitalization or intensive care unit (ICU) admissions.29 Lastly, a retrospective review was published in 2019 that, although it did not show the same benefits as previously mentioned in the adult studies, it did support the safety of the two-bag approach and that it is an appropriate alternative to the one-bag approach.34 Ultimately, further research will need to be completed to elucidate the efficacy of the two-bag approach in adults, but if benefits continue to be seen, the future approach to DKA management may shift toward its more consistent use.
The last consideration in the administration of fluids in DKA management is the risk of iatrogenic fluid overload. While fluid resuscitation is key in the treatment of DKA, it should be used with caution in patients with heart failure, those who are dialysis dependent, and patients with advanced liver disease. It is imperative to monitor the overall status of these patients closely to help guide fluid resuscitation (e.g., vitals, improved signs of dehydration, urine output, and cardiac function). These patients may benefit more from starting with smaller boluses of IV fluids (250 mL to 500 mL) and close monitoring of changes to clinical status.3,20,22,35 Some experts recommend the use of ultrasound, primarily the views of the inferior vena cava and cardiac windows, to better determine a patient’s volume status and adjust fluid administration accordingly.22 The administration of IV fluids in DKA management is summarized in Figure 1.
Electrolyte Replacement
As previously mentioned, it is not uncommon for a patient with DKA to have multiple associated electrolyte abnormalities, so it is important to check their levels frequently throughout treatment, initially every two hours, and then the timing can be spread out once the patient becomes more stable.1 The most consequential of these irregularities is potassium. Because of extracellular shifts secondary to acidosis, lack of insulin, and volume depletion, patients may present with normal-to-high levels of serum potassium even though they have a total body potassium deficit. The treatments initiated in DKA management to address these abnormalities can exacerbate this deficit, making potassium replacement an important factor to address.11,16-18,20,28 Potassium levels should be obtained promptly and assessed prior to starting insulin therapy. Typically, if a patient’s initial potassium is > 5.2 mEq/L, insulin can be started without prior potassium replacement. However, if the patient’s potassium is 3.3 mEq/L to 5.2 mEq/L, insulin can be started with concurrent potassium replacement. Lastly, if the patient’s potassium is < 3.3 mEq/L, insulin must be held until adequate potassium replacement has occurred.11,28
Recent reviews even suggest a more conservative approach to potassium replacement, proposing that insulin not be initiated until potassium levels reach 3.5 mEq/L.1 Per ADA recommendations, the goal on repeated potassium serum monitoring should be to maintain a level of 4 mEq/L to 5 mEq/L. To accomplish this, 20 mEq to 30 mEq of potassium should be given for every 1 L of fluids administered.3,20 Alternatively, the more recent British guidelines recommend
40 mEq of potassium for each liter of fluids administered when potassium levels are < 5.5 mEq/L.27 (See Figure 2.)
Figure 2. Approach to Potassium Replacement in Diabetic Ketoacidosis Management Based on ADA Guidelines |
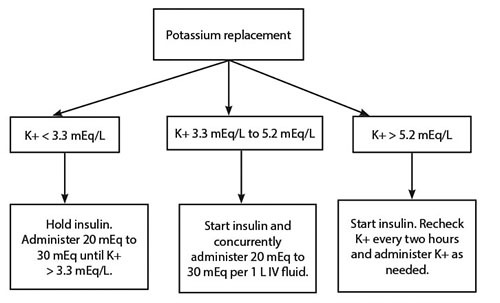 |
ADA: American Diabetes Association; K+: potassium; IV: intravenous |
Hypomagnesemia also may result as a consequence of osmotic diuresis. Therefore, magnesium also should be monitored closely and replaced, since it will aid in potassium absorption and also can help mitigate the risk of dysrhythmias if the patient is profoundly hypokalemic.1 One to two grams of IV magnesium sulfate can be given over an hour for replacement as needed, with a goal level of > 2 mg/dL.1,11
Phosphate replacement also could be considered if a patient’s serum levels are severely depleted (e.g., < 1 mEq/dL, cardiac dysfunction, respiratory depression, skeletal muscle weakness, seizures); however, it is not routinely recommended. There is a risk of inducing hypocalcemia with phosphate repletion, so it should be used cautiously. If needed, 20 mEq to 30 mEq of potassium phosphate can be added to 1 L of replacement fluid.1,3,20,28
Insulin Administration
As stated before, the goal of insulin therapy is not only to decrease serum glucose levels by promoting peripheral glucose metabolism, but also to inhibit ketone production and subsequently resolve the ketoacidosis. However, the resolution of glucose levels usually occurs prior to the resolution of acidosis, so the ultimate goal of insulin therapy should be the closure of the anion gap.11,15,20 After the initial fluid resuscitation is complete, and the patient’s potassium is within appropriate levels, insulin administration should be initiated. Because of its easy titration and short half-life, it is recommended to start patients on continuous IV regular insulin at an infusion rate of 0.1 units/kg to 0.14 units/kg per hour without a preceding loading dose.3,11,20,27 At this rate, it is expected that blood glucose levels will decrease by 50 mg/dL to 75 mg/dL per hour.11,13
If this decrease is not seen within the first hour of its infusion, the insulin rate can be doubled, and it also is necessary to ensure that other measures of treatment — fluids and electrolyte replacement — are optimized.1,11,13 As previously discussed, once glucose levels reach 250 mg/dL, the patient must start to receive dextrose in fluids, since the insulin infusion should continue until the anion gap is resolved, and it is necessary to mitigate the risk of hypoglycemia. Once glucose levels are < 200 mg/dL, the insulin infusion rate can be decreased to 0.02 units/kg to 0.05 units/kg per hour.3,11,16
The insulin transfusion should continue until glucose is < 200 mg/dL and two of the following qualifiers have been met:11,20
• serum bicarbonate level > 15 mEq;
• venous pH > 7.3;
• anion gap < 12 mEq/L;
• ability to tolerate oral intake.
At this point in time, the transition to subcutaneous (SC) insulin can be started. The transition to SC insulin should overlap with IV therapy for about two to four hours to circumvent relapse hyperglycemia. Per the more recent British recommendations, patients also should be given either their home dose of basal insulin or started on 0.25 units/kg of short-acting insulin during DKA management to aid in preventing rebound hyperglycemia as well.27,28 Otherwise, the transition to SC insulin is going to vary on a case-by-case basis and individual institutional policy and usually will involve the help of the available diabetes specialists. While it is not always a reality, it is likely that by this point the patient has been admitted and this transition step will be managed by the inpatient team.1,9,15,27
Considering Bicarbonate
Bicarbonate administration is not routinely recommended in the management of DKA, since acidosis is treated with and usually resolves with the methods discussed earlier. Additionally, the use of bicarbonate has been associated with possible risks, such as worsened intracellular acidosis, worsening of hypokalemia, cerebral edema, increased time to acidosis resolution, paradoxical central nervous system acidosis, hypertonicity, and hypernatremia.1,2,11,16 Nonetheless, the ADA recommends the administration of sodium bicarbonate if the initial pH is < 6.9 because of the severity of acidosis and the critical nature of the patient’s pathology.3 In contrast, the British guidelines do not recommend its use in DKA patients because of potential risks and lack of evidence reporting benefits.27,28 As such, the use of bicarbonate should be used judiciously and on a case-by-case basis when needed.
EDKA
Management of EDKA adheres to the same principles as that of DKA: fluid resuscitation, insulin administration, and electrolyte replacement. While the IV fluid resuscitation and electrolyte monitoring and repletion follow the same management as discussed earlier, the insulin administration for EDKA differs slightly than for DKA. Because the serum glucose is relatively normal (≤ 250 mg/dL), dextrose (5% or 10%) should be added initially to fluids to help prevent hypoglycemia and expedite clearance of ketosis.9,36,37 Similarly, it is recommended to avoid an insulin bolus and use the lower dose (0.1 unit/kg per hour) for continuous insulin infusion until the anion gap closes.9,36,37 Additionally, if the patient is taking an sodium-glucose cotransporter 2 (SGLT-2) inhibitor, it is important to discontinue this until recovery and then consult endocrinology to determine the best regimen for continued outpatient management of diabetes.
HHS
Similarly, while HHS is very similar to DKA and shares many of the same principles of treatment and goals, there are some key differences that affect management. This is important to know, since most protocols combine DKA and HHS, including ADA recommendations. First, because HHS occurs over a period of several days, as opposed to DKA which develops quite rapidly, physiologic abnormalities should be corrected more slowly and controlled to prevent complications, such as cerebral edema and osmotic demyelination syndrome (ODS).7 Therefore, fluid administration, including rate and composition, depends on both the corrected serum sodium levels and serum osmolality. Beginning with normal saline (NS, 0.9% sodium chloride) boluses and infusion for immediate resuscitation in the setting of hypotension and hypovolemia is appropriate and can follow the same recommendations as for DKA discussed earlier.
However, once stabilized, the glucose, serum osmolality, and corrected sodium should be calculated and used to help guide fluids. The fluids themselves should help to decrease glucose levels at approximately 75 mg/dL to 100 mg/dL per hour. The change in serum osmolality should be kept at 3 mOsm/kg per hour or less to prevent rapid alterations that can lead to cerebral edema.7 As for the sodium, for every 100 mg/dL drop in glucose, there is a 2.4 mEq/L increase in sodium. Both serum osmolality and corrected sodium should be monitored every one to two hours during treatment.
General principles for fluid therapy in HHS are listed in Table 4.
Table 4. General Principles of Fluid Therapy in Hyperosmolar Hyperglycemic Syndrome7 |
Inadequate fluid administration is suggested if:
Continue with 0.9% normal saline (NS) if:
Switch to 0.45% NS or lactated Ringer’s (LR) if:
Hold fluids if:
If severe overcorrection > 8 mOsm/kg per hour, administer D50 boluses. |
In HHS, half of the fluid deficit should be restored in the first 18-24 hours and the remainder over the next 24 hours to aid with this slow correction back to normal physiology.7
Insulin administration in HHS treats the hyperosmolality rather than ketoacidosis in DKA.7 In addition, although the glucose is significantly more elevated in HHS than in DKA, the fluid administration helps decrease both glucose and the hyperosmolality, and it is acceptable to hold insulin infusion until there is a plateau in glucose levels. For these reasons, a decreased insulin need makes sense, and proceeding without a bolus to a lower infusion dose can be effective. The recommended insulin dose is a 0.05 unit/kg to 0.1 unit/kg per hour regular insulin infusion along with the patient’s home dose of long-acting insulin or 0.3 U/kg glargine SC.7
Using protocols developed for DKA is acceptable for treating HHS, but insulin should be reduced or stopped once glucose levels reach 300 mg/dL while fluids are continued until hyperosmolality resolves.7,38 The goal in treating HHS is correction of serum glucose, electrolytes, and osmolality. (See Table 5.)
Table 5. Correction Targets in Hyperosmolar Hyperglycemic Syndrome Management7,12,38 |
|
Hypoglycemia
As previously discussed, it is important to obtain a POC glucose when hypoglycemia is suspected because prompt recognition and treatment are crucial to avoid detrimental effects. Treatment is based on the patient’s level of alertness and ability to swallow.
In an asymptomatic patient who is found to be hypoglycemic on testing, treatment is straightforward. Provide a source of carbohydrates for them to eat and recheck glucose in 15 minutes. Repeat as needed and ensure proper medication dosages and patient understanding of medication administration. For a symptomatic patient who is awake and alert, similar treatment can be used with oral administration of approximately 15 g to 20 g of quickly absorbable carbohydrates (e.g., fruit juice, regular soda, sugar water, crackers, hard candies, or glucose tablets). Retest POC glucose after 15 minutes and again repeat as necessary. Once glucose levels are stabilized and remain ≥ 70 mg/dL, the patient should have a meal or snack with longer-acting carbohydrates to prevent recurrence of hypoglycemia. Of note, if the patient is taking an alpha glucosidase inhibitor, only pure glucose, such as glucose tablets, should be ingested. This is because the medication slows digestion of disaccharides, so other forms of carbohydrates will be less effective in acutely raising blood sugar.39
If the patient is unconscious or significantly altered, or if there is a concern for aspiration or the patient is not receiving anything by mouth for any other reason, treatment with IV dextrose should be initiated. Intravenous treatment generally consists of a bolus dose of 50 mL of 50% dextrose (D5W), typically in a prefilled syringe colloquially called D50. Glucose then should be rechecked in 15 minutes. If the patient still is hypoglycemic, these initial steps can be repeated two more times, rechecking glucose every 15 minutes.
In the case of a patient continuing to be hypoglycemic after these initial interventions, or if IV access is unable to be obtained, 1 mg of intramuscular or subcutaneous glucagon should be administered.
In patients who require ongoing boluses, who do not return to their neurological baseline, who cannot tolerate taking medication by mouth, or who have hypoglycemia secondary to long-acting medications, an infusion of D5W or D10W should be initiated for ongoing maintenance. As always, frequent glucose monitoring is essential.
Of note, hypoglycemia related to sulfonylurea toxicity can be particularly difficult to treat, with a potentially prolonged course. Octreotide should be administered concurrently with the IV dextrose, as mentioned earlier. Octreotide is a somatostatin analog that inhibits insulin release from pancreatic beta cells. Solo treatment with IV dextrose in sulfonylurea toxicity can cause transient hyperglycemia, which triggers insulin release and resulting hypoglycemia. The octreotide helps prevent the insulin release, ultimately creating a steadier state.11,40-44 The most common dose of octreotide is 50 mcg to 100 mcg intramuscular or subcutaneous every six hours.
Additional Aspects
It is essential to initiate therapy as quickly as possible for hyperglycemic crises, since delayed care can lead to serious complications and sequelae, including seizures, coma, and organ failure. Within the first 48-72 hours, the majority of the deaths in hyperglycemic crises are due to the precipitating cause, potassium derangements, and cerebral edema.20 As previously mentioned, HHS has a higher overall mortality rate than DKA, which is even more exemplified when treatment is delayed. Acute myocardial and bowel infarction can occur secondary to prolonged hypotension in DKA, and the massive dehydration in HHS can lead to additional complications, such as stroke, pulmonary embolism, disseminated intravascular coagulation, and mesenteric vein thrombosis.20
Studies have shown a higher risk of venous thromboembolism (VTE), particularly in HHS, both during hospitalization and for several months following resolution.9,20 While British guidelines recommend prophylactic low molecular weight heparin for HHS patients throughout admission, the ADA guidelines do not include any recommendations on anticoagulation;9 however, it is likely that patients are receiving VTE prophylaxis as part of routine hospital protocols, especially in the intensive care unit (ICU).
It is important to recognize how chronic kidney disease worsens the prognosis, since the kidneys play a vital role in managing the pH and electrolyte abnormalities.20 On the flip side, the pathophysiology of DKA and HHS can lead to acute worsening of kidney function or even development of end-stage kidney disease. Dialysis patients with hyperglycemic emergencies have differences in presentations, laboratory results, and treatment. They do not have the typical osmotic diuresis, so there is less volume and electrolyte loss, and they can have a mixed metabolic acidosis with metabolic alkalosis due to the increased bicarbonate in the dialysate.9 Being conservative with IV fluid administration to avoid volume overload is necessary. In addition, they typically are hyperkalemic, so less potassium supplementation is necessary.
Although some patients may present critically ill and airway, breathing, and circulation take priority, intubation should be avoided unless absolutely necessary. Because of the metabolic acidosis, minute ventilation increases to expire more CO2, thereby compensating the metabolic acidosis via a respiratory alkalosis. Any period of apnea, even if short during intubation, can cause further acidosis and elevation of CO2 levels. Following intubation, matching the minute ventilation can be difficult, and that level of compensation is difficult to achieve. Ultimately, intubation may worsen the acidosis and contribute to circulatory collapse. If intubation is absolutely required, use mask ventilation during any apnea, use measures to optimize first-pass success, use short-acting paralytics, and set a ventilator mode that lets the patient set the rate and tidal volume for hyperventilation.9
While prompt management is essential, there also are complications to be aware of from treatment. Hypoglycemia and hypokalemia are the most common adverse effects, but they can be avoided with careful monitoring.12,45 One of the most feared complications with treatment of DKA is cerebral edema, which usually develops within the initial 12 hours but can be delayed up to two to three days. It almost exclusively occurs in people younger than 20 years of age and has a significant mortality rate of 20% to 40%.9,12,45 Cerebral edema is more common with sicker presentations. The pathophysiology is not fully understood but does not appear to be related to initial osmolality or osmotic changes during management of DKA; however, some small animal studies suggest that a rapid decline in osmolality can contribute to cerebral edema in HHS, so it is recommended to keep serum glucose near 300 mg/dL during treatment.9 Symptoms are those of increased intracranial pressure, and treatment is with mannitol and/or hypertonic saline.
Disposition
Hyperglycemic Emergencies
For hyperglycemic crises, nearly all patients require admission to the hospital. Often, this will be to the ICU due to the frequency of POC glucose checks, laboratory tests, monitoring needs, and attendance to medication drips. For very mild cases that respond well to resuscitation or only require subcutaneous insulin, discharge may be possible, but only after a thorough workup, and this is best done in consultation with the patient’s endocrinologist.9
While IV insulin is the standard of care per ADA guidelines, there are some studies showing similar outcomes with the use of subcutaneous insulin in mild to moderate DKA.9 Subcutaneous shorter-acting insulin (aspart or lispro) administered every one to two hours has shown no difference in mortality, duration of treatment until correction of hyperglycemia or resolution of ketoacidosis, length of hospital stay, episodes of hypoglycemia, or total insulin dose.9,16,46,47 This potentially could reduce ICU admission and costs in mild to moderate DKA, but still requires close glucose monitoring.
Resolution of hyperglycemic emergencies is indicated by correction of dehydration and normalization of serum glucose and electrolytes. For DKA, serum glucose should be < 200 mg/dL, and additional parameters must be attained: serum bicarbonate ≥ 15 mEq/L, pH ≥ 7.3, and anion gap ≤ 12 mEq/L.20 For HHS, these criteria plus normalization of osmolality are needed.
Some risk factors associated with adverse outcomes, such as repeat ED visits, hospital admissions, or death, to be aware of include increased age, low socioeconomic status, living in urban settings, presence of comorbidities, coexisting elevated lactate, increased creatinine, a visit to the ED for hyperglycemia in the past month, and high glucose on presentation.48,49 Interestingly, this large study showed tachycardia and systolic blood pressure of 90 mmHg to 150 mmHg to be protective.49 Knowing these factors can aid in predicting worsening clinical status or need for more intensive care.
Hypoglycemia
For hypoglycemic emergencies, admission is not as definite. As mentioned previously, if the patient is having repeat episodes of hypoglycemia, is not back to baseline despite improved serum glucose, requires multiple doses of D50, is on a dextrose drip, has other pathology, or has toxicity from long-acting medications (particularly sulfonylureas), admission is indicated. The admission unit will be based on their monitoring needs and whether continuous infusions are running.
Summary
Overall, diabetes is an increasing disease among all age groups, making it guaranteed that patients with diabetic emergencies will be seen frequently in the ED. Knowing that both DKA and HHS can happen in both type 1 and type 2 diabetes mellitus and that infection is the biggest precipitating factor for both will help keep a broad differential and workup. SGLT-2 inhibitors are one of the most common causes for EDKA, which should cause consideration for the diagnosis.
All of the diabetic emergencies present with vague symptoms, so obtaining a POC glucose is a very easy and quick way to help rule in or out other causes. Capnography is another very simple way to help discern DKA that is not found in many hospital protocols.
Although DKA and HHS share similar treatment goals — addressing fluid status, repleting electrolytes, reversing acidosis, and improving the hyperglycemia — there are subtle differences that are very important. The serum sodium and osmolality guide fluid administration much more in HHS, which takes a longer period to develop in the first place. Caution should be taken with intubating DKA patients because of disruption of their respiratory compensation. Patients with kidney disease may have differing laboratory presentations and treatment requirements.
Nearly all patients with hyperglycemic emergencies require admission with various IV infusions, although there is a possibility of using subcutaneous insulin for mild DKA to avoid ICU or admission. On the other hand, many hypoglycemic patients may be able to be discharged unless there are other underlying disease processes to be managed or if they are on sulfonylureas. It is essential that providers consider these diagnoses, evaluate them efficiently and thoroughly, and ultimately treat them appropriately and quickly, since DKA, EDKA, HHS, and hypoglycemia can be deadly.
REFERENCES
- Long B, Willis GC, Lentz S, et al. Evaluation and management of the critically ill adult with diabetic ketoacidosis. J Emerg Med 2020;59:371-383.
- Gosmanov AR, Gosmanova EO, Kitabchi AE, et al. Hyperglycemic crises: Diabetic ketoacidosis and hyperglycemic hyperosmolar state. May 9, 2021. Endotext [Internet]. MDText.com, Inc.
- Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care 2009;32:1335-1343.
- Soleimanpour H, Taghizadieh A, Niafar M, et al. Predictive value of capnography for suspected diabetic ketoacidosis in the emergency department. West J Emerg Med 2013;14:590-594.
- Chebl RB, Madden B, Belsky J, et al. Diagnostic value of end tidal capnography in patients with hyperglycemia in the emergency department. BMC Emerg Med 2016;16:7.
- Baldrighi M, Sainaghi PP, Bellan M, et al. Hyperglycemic hyperosmolar state: A pragmatic approach to properly manage sodium derangements. Curr Diabetes Rev 2018;14:534-541.
- Long B, Willis GC, Lentz S, et al. Diagnosis and management of the critically ill adult patient with hyperglycemic hyperosmolar state. J Emerg Med 2021;61:365-375.
- Ramphul K, Joynauth J. An update on the incidence and the burden of diabetic ketoacidosis in the U.S. Diabetes Care 2020;43:e196-e197.
- Dingle HE, Slovis C. Diabetic hyperglycemic emergencies: A systematic approach. Emerg Med Pract 2020;22:1-20.
- Stoudt K, Chawla S. Don’t sugar coat it: Glycemic control in the intensive care unit. J Intensive Care Med 2019;34:889-896.
- Jalili M, Niroomand. Type 2 diabetes mellitus. In: Tintinalli JE, Ma OJ, Yealy DM, et al. Emergency Medicine: A Comprehensive Study Guide. 9th ed. McGraw-Hill Education;2020.
- Hirsch IB, Emmett M. Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Clinical features, evaluation, and diagnosis. UpToDate. Updated June 6, 2022. https://www.uptodate.com/contents/diabetic-ketoacidosis-and-hyperosmolar-hyperglycemic-state-in-adults-clinical-features-evaluation-and-diagnosis?search=dka&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2
- Eledrisi MS, Elzouki AN. Management of diabetic ketoacidosis in adults: A narrative review. Saudi J Med Med Sci 2020;8:165-173.
- Muneer M, Akbar I. Acute metabolic emergencies in diabetes: DKA, HHS and EDKA. In: Islam MS, ed. Diabetes: From Research to Clinical Practice. Advances in Experimental Medicine and Biology, vol. 1307. Springer;2020. https://doi.org/10.1007/5584_2020_545
- Pitocco D, Di Leo M, Tartaglione L, et al. An approach to diabetic ketoacidosis in an emergency setting. Rev Recent Clin Trials 2020;15:278-288.
- Umpierrez GE. Hyperglycemic crises: Diabetic ketoacidosis and hyperglycemic hyperosmolar state. In: Bonora E, DeFronzo RA, eds. Diabetes Complications, Comorbidities and Related Disorders. Springer Nature;2020:596-614.
- Dhatariya KK. Defining and characterising diabetic ketoacidosis in adults. Diabetes Res Clin Pract 2019;155:107797.
- Dhatariya K, Matfin G. Severe hyperglycemia, diabetic ketoacidosis, and hyperglycemic hyperosmolar state. In: Matfin G, ed. Endocrine and Metabolic Medical Emergencies: A Clinician’s Guide, 2nd ed. John Wiley & Sons Ltd.;2018:531-547.
- Lizzo JM, Goyal A, Gupta V. Adult diabetic ketoacidosis. In: StatPearls [Internet]. Updated Nov. 20, 2021. StatPearls Publishing; 2022.
- Aldhaeefi M, Aldardeer NF, Alkhani N, et al. Updates in the management of hyperglycemic crisis. Front Clin Diabetes Healthc 2022. doi.org/10.3389/fcdhc.2021.820728
- Semler MW, Self WH, Wanderer JP, et al. SMART Investigators and the Pragmatic Critical Care Research Group. Balanced crystalloids versus saline in critically ill adults. N Engl J Med 2018;378:829-839.
- Farkas J. Diabetic ketoacidosis. Internet Book of Critical Care. Updated Aug. 6, 2021. https://emcrit.org/ibcc/dka/#fluid_administration
- Van Zyl DG, Rheeder P, Delport E. Fluid management in diabetic acidosis–Ringer’s lactate versus normal saline: A randomized controlled trial. QJM 2012;105:337-343.
- Mahler SA, Conrad SA, Wang H, Arnold TC. Resuscitation with balanced electrolyte solution prevents hyperchloremic metabolic acidosis in patients with diabetic ketoacidosis. Am J Emerg Med 2011;29:670-674.
- Ramanan M, Attokaran A, Murray L, et al. SCOPE-DKA Collaborators and Queensland Critical Care Research Network (QCCRN). Sodium chloride or Plasmalyte-148 evaluation in severe diabetic ketoacidosis (SCOPE-DKA): A cluster, crossover, randomized, controlled trial. Intensive Care Med 2021;47:1248-1257.
- Self WH, Evans CS, Jenkins CA, et al. Pragmatic Critical Care Research Group. Clinical effects of balanced crystalloids vs saline in adults with diabetic ketoacidosis: A subgroup analysis of cluster randomized clinical trials. JAMA Netw Open 2020;3:e2024596.
- Dhatariya K; Joint British Diabetes Societies for Inpatient Care. The management of diabetic ketoacidosis in adults. (JBDS 02). Revised June 2021.
- Karslioglu French E, Donihi AC, Korytkowski MT. Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome: Review of acute decompensated diabetes in adult patients. BMJ 2019;65:l1114.
- Haas NL, Gianchandani RY, Gunnerson KJ, et al. The two-bag method for treatment of diabetic ketoacidosis in adults. J Emerg Med 2018;54:593-599.
- Munir I, Fargo R, Garrison R, et al. Comparison of a ‘two-bag system’ versus conventional treatment protocol (‘one-bag system’) in the management of diabetic ketoacidosis. BMJ Open Diabetes Res Care 2017;5:e000395.
- So TY, Grunewalder E. Evaluation of the two-bag system for fluid management in pediatric patients with diabetic ketoacidosis. J Pediatr Pharmacol Ther 2009;14:100-105.
- Velasco JP, Fogel J, Levine RL, Ciminera P, et al. Potential clinical benefits of a two-bag system for fluid management in pediatric intensive care unit patients with diabetic ketoacidosis. Pediatr Endocrinol Diabetes Metab 2017;23:6-13.
- Veverka M, Marsh K, Norman S, et al. A pediatric diabetic ketoacidosis management protocol incorporating a two-bag intravenous fluid system decreases duration of intravenous insulin therapy. J Pediatr Pharmacol Ther 2016;21:512-517.
- Cho N, Bushell T, Choi M, Moussavi K. Evaluation of the two-bag system in adult diabetic ketoacidosis patients. J Pharm Pract 2021;34:17-22.
- Eledrisi MS, Beshyah SA, Malik RA. Management of diabetic ketoacidosis in special populations. Diabetes Res Clin Pract 2021;174:108744.
- Plewa MC, Bryant M, King-Thiele R. Euglycemic diabetic ketoacidosis. In: StatPearls [Internet]. StatPearls Publishing; 2022.
- Nasa P, Chaudhary S, Shrivastava PK, Singh A. Euglycemic diabetic ketoacidosis: A missed diagnosis. World J Diabetes 2021;12:514-523.
- Stoner GD. Hyperosmolar hyperglycemic state. Am Fam Physician 2017;96:729-736.
- Cryer PE. Hypoglycemia in adults with diabetes mellitus. UpToDate. Updated April 19, 2021. https://www.uptodate.com/contents/hypoglycemia-in-adults-with-diabetes-mellitus?search=hypoglycemia&source=search_result&selectedTitle=3~150&usage_type=default&display_rank=3#H1
- Lamos EM, Younk LM, Davis SN. Hypoglycemia. In: Matfin G, ed. Endocrine and Metabolic Medical Emergencies: A Clinician’s Guide, 2nd ed. John Wiley & Sons Ltd.;2018:506-530.
- Fanelli CG, Lucidi P, Bolli GB, Porcellati F. Hypoglycemia. In: Bonora E, DeFronzo RA, eds. Diabetes Complications, Comorbidities and Related Disorders. Springer Nature;2020:615-652.
- Muneer M. Hypoglycaemia. In: Islam MS, ed. Diabetes: From Research to Clinical Practice. Advances in Experimental Medicine and Biology. Springer;2020. https://doi.org/10.1007/5584_2020_534
- Nakhleh A, Shehadeh N. Hypoglycemia in diabetes: An update on pathophysiology, treatment, and prevention. World J Diabetes 2021;12:2036-2049.
- Chu J, Stolbach A. Sulfonylurea agent poisoning. UpToDate. Updated Aug. 12, 2020. https://www.uptodate.com/contents/sulfonylurea-agent-poisoning?search=sulfonylureas&source=search_result&selectedTitle=2~112&usage_type=default&display_rank=2#H1
- Wolf RA, Haw JS, Paul S, et al. Hospital admissions for hyperglycemic emergencies in young adults at an inner-city hospital. Diabetes Res Clin Pract 2019;157:107869.
- Rao P, Jiang S, Kipnis P, et al. Evaluation of outcomes following hospital-wide implementation of a subcutaneous insulin protocol for diabetic ketoacidosis. JAMA Netw Open 2022;5:e226417.
- Vincent M, Nobécourt E. Treatment of diabetic ketoacidosis with subcutaneous insulin lispro: A review of the current evidence from clinical studies. Diabetes Metab 2013;39:299-305.
- Yan JW, Spaic T, Liu S. Just the facts: Diagnosis and treatment of diabetic ketoacidosis in an emergency department. CJEM 2020;22:19-22.
- Siddiqi L, VanAarsen K, Iansavichene A, Yan J. Risk factors for adverse outcomes in adult and pediatric patients with hyperglycemia presenting to the emergency department: A systematic review. Can J Diabetes 2019;43:361-369.
