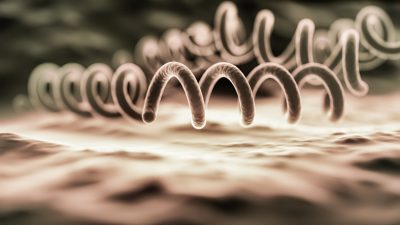
Syphilis has continued its upward trend, reaching the highest number of cases in the United States in 2023 since the 1950s. There was a brief dip in cases during the first few months of social isolation with COVID, but, overall, cases have doubled since 2015. It is obvious the current approach of testing those who present with symptoms or other sexually transmitted infections is not sufficient.
SPECIAL REPORT
Combatting the Resurgence of Syphilis
November 30, 2024
