CAUTIs: What to Do, What Not to Do
SHEA/APIC/IDSA complete compendium update for HAIs
“If you take a room of 1,000 people, all of them are going to have bacteria in their urine,” says lead author Payal Patel, MD. “Getting a urine culture on all of them doesn’t give you any great evidence of infection. Many randomized controlled trials have shown us that screening for asymptomatic bacteremia in patients just doesn’t help. We feel confident saying that screening shouldn’t be considered a routine part of infection prevention.”
Exceptions include “the few patient populations for which this is anticipated to have more benefit than harm, pregnant women, [and] patients undergoing endoscopic urologic procedures associated with mucosal trauma,” the recommendations state.1
Periodically updated to reflect the most current infection control guidelines, the compendium is a collaborative effort by the Society for Healthcare Epidemiology of America (SHEA), the Infectious Diseases Society of America, the Association for Professionals in Infection Control and Epidemiology, the American Hospital Association, and The Joint Commission.
“Treatment of asymptomatic bacteriuria is not an effective strategy to prevent CAUTI in other patient groups, as it increases the risk of antibiotic-associated complications more than any potential benefit prevention of symptomatic CAUTI,” the guidelines note. “The conditions that predisposed the patient to have bladder colonization (anatomic, immunologic) are not resolved by antibiotics, and so the bacteriuria recurs.”
Another practice the guidelines specifically warn against is routine use of antimicrobial- and antiseptic-impregnated catheters.
“There still continues to be work in this space, so potentially things could change,” Patel said. “But there have been a lot of studies looking at whether antimicrobial- or antiseptic-impregnated catheters could prevent CAUTI. Unfortunately, the evidence does not show that those are going to help. One of the reasons is that this is a really difficult way to try to prevent infection. You’re just never going to be able to — and you probably shouldn’t — sterilize the bladder completely.”
CAUTIs are one of the most prevalent healthcare-associated infections. Approximately 75% of them are caused by indwelling Foley catheters. They are left in place beyond their point of utility and can become contaminated by handling and adjustments, seeding an infection that is going to complicate the patient’s stay.
Accordingly, the new recommendations include a graphic outlining the steps to take to “disrupt” this process and remove the catheter in a timely fashion. (See Figure 1.)
Figure 1. Disrupting the Lifecycle of the Indwelling Urethral Catheter to Reduce Catheter-Associated Infection and Trauma |
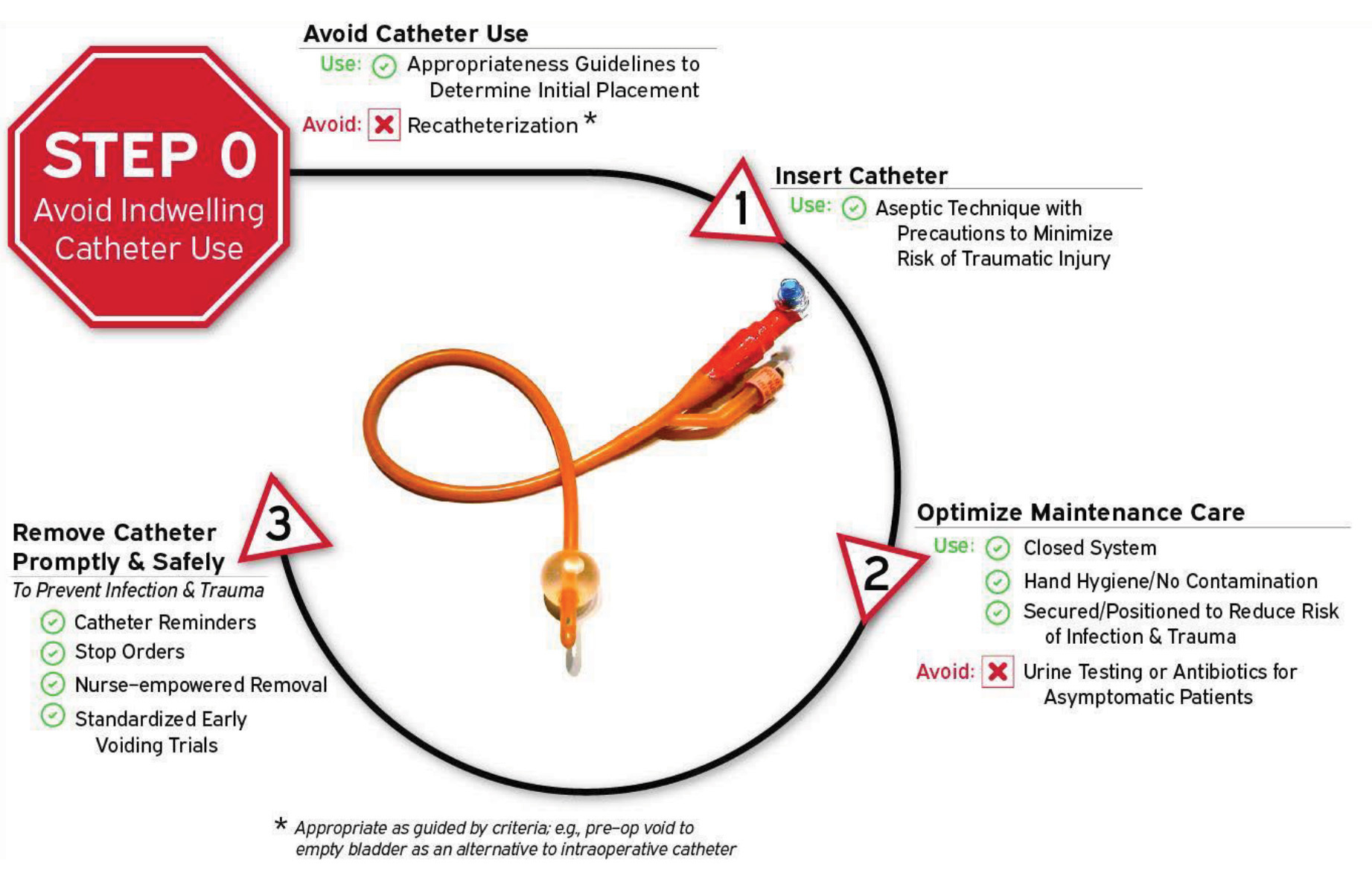 |
Source: Patel PK, Advani SD, Kofman AD, et al. Strategies to prevent catheter-associated urinary tract infections in acute-care hospitals: 2022 update. Infect Control Hosp Epidemiol 2023;44:1209-1231. |
“The drainage bag of the bacteriuric patient is a reservoir for organisms that may be transmitted through the hands of healthcare personnel,” the guidelines state. “The drainage bag can also become contaminated by contact with hands due to inadequate hand hygiene, contact with the patient’s skin or hands, or contact with the floor or vessel used to empty the bag. Outbreaks of infections associated with resistant gram-negative organisms attributable to bacteriuria in catheterized patients have been reported.”
Since the duration of catheterization is the most important risk factor for developing infection, the authors recommend at least daily review of continued catheterization, which can include automated reminders of the presence of a catheter or review during rounds of all patients with urinary catheters. Nurse-driven protocols for catheter removal are an option to expedite the process, but some facilities still require a physician’s order. Hospital Infection Control & Prevention asked if this still is a controversial issue.
“I don’t think so,” Patel says. “Nurse-driven protocols are all a part of this idea of improving the appropriateness of catheter [use]. In the culture of your hospital, if that is the easiest way to do it, and everyone’s on board, that is a fantastic way to do it. Another way is when people are ordering the placement of the catheter, have a checklist — does this patient meet any of these criteria to have a catheter placed? If the answer is ‘no,’ then consider an alternative. That’s a way to stop it before it even gets placed.”
With the CAUTI paper, the full compendium of updates has been published in the SHEA journal, Infection Control and Hospital Epidemiology. This began last year with publication of strategies to prevent ventilator- and non-ventilator-associated pneumonia.2 That has been followed by compendium updates on infection control and hand hygiene, methicillin-resistant Staphylococcus aureus, Clostridioides difficile infections, surgical site infections, and central line-associated bloodstream infections.3-7
“These were going to be published anyway; timing became more important because of the pandemic,” Patel says. “Hospitals were under such stress during COVID, and we saw a rise in a number of healthcare-associated infections. That’s why I think the timing of the compendium is really important. This is a good time to kind of focus back, when they may have maybe a little bit more time and resources to think about this. As we go into the next few years, we can really be focusing on infection prevention.”
REFERENCES
- Patel PK, Advani SD, Kofman AD, et al. Strategies to prevent catheter-associated urinary tract infections in acute-care hospitals: 2022 update. Infect Control Hosp Epidemiol 2023;44:1209-1231.
- Klompas M, Branson R, Cawcutt K, et al. Strategies to prevent ventilator-associated pneumonia, ventilator-associated events, and nonventilator hospital-acquired pneumonia in acute-care hospitals: 2022 update. Infect Control Hosp Epidemiol 2022;43:687-713.
- Popovich KJ, Aureden K, Ham DC, et al. SHEA/IDSA/APIC Practice Recommendation: Strategies to prevent methicillin-resistant Staphylococcus aureus transmission and infection in acute-care hospitals: 2022 update. Infect Control Hosp Epidemiol 2023;29;44:1-29.
- Glowicz JB, Landon E, Sickbert-Bennett, EE, et al. SHEA/IDSA/APIC Practice Recommendation: Strategies to prevent healthcare-associated infections through hand hygiene: 2022 update. Infect Control Hosp Epidemiol 2023;44:355-376.
- Kociolek LK, Gerding DN, Carrico R, et al. Strategies to prevent Clostridioides difficile infections in acute-care hospitals: 2022 update. Infect Control Hosp Epidemiol 2023;44:527-549.
- Buetti N, Marschall J, Drees M, et al. Strategies to prevent central line-associated bloodstream infections in acute-care hospitals: 2022 update. Infect Control Hosp Epidemiol 2022;43:553-569.
- Calderwood MS, Anderson DJ, Bratzler DW, et al. Strategies to prevent surgical site infections in acute-care hospitals: 2022 update. Infect Control Hosp Epidemiol 2023;44:695-720.
New compendium recommendations by the nation’s leading infection control groups on catheter-associated urinary tract infections (CAUTIs) emphasize that, in most cases, screening for asymptomatic bacteriuria does more harm than good.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
