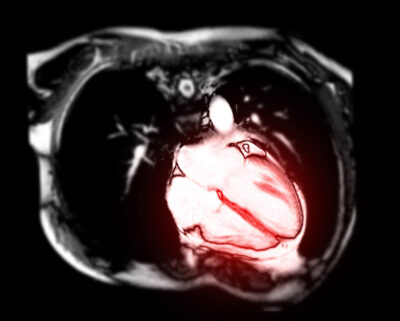
An international study of patients with moderate or asymptomatic severe aortic stenosis has demonstrated that increased amounts of left ventricular fibrosis, as measured by cardiac magnetic resonance imaging, is associated with worse outcomes.
ABSTRACT & COMMENTARY
A New Technique for Predicting Outcomes in Asymptomatic AS
November 1, 2024
