Sports-Related Head Injuries: Learn the Rules of this Serious Game
Authors: Don W. Penney, MD, MSc, FACEP, Neurological Surgeon; Professor, Department of Emergency Medicine, Medical College of Georgia, Augusta; and Ronald M. Perkin, MD, MA, FAAP, FCCM, Professor and Chairman, Department of Pediatrics, The Brody School of Medicine at East Carolina University, Greenville, NC.
Peer Reviewer: Norman C. Christopher, MD, Director, Emergency/Trauma Services, Children’s Hospital Medical Center of Akron, Akron, OH.
Pediatric athletic head injuries are a significant problem, especially for emergency medicine physicians. The dedication of many young athletes to performance and their avoidance of restrictions makes it imperative that ED physicians recognize and give appropriate recommendations to parents and coaches of young athletes. The cumulative damage that may result from repetitive minor head trauma is not recognized by the majority of athletes, and the ED physician has the burden of conveying these potential risks to the family. This article provides a comprehensive review of sports-related head injuries and recommendations on grading of concussions, imaging, and the safe return of the athlete to competition.—The Editor
Introduction
There are approximately 300,000 sports-related head injuries each year in the United States.1-3 Most of these head injuries are considered mild to moderate in severity, and many go unrecognized and untreated. Increasingly, team trainers, coaches, and parents are utilizing the emergency department to provide care and management recommendations. Optimal care of the head-injured athlete requires an appreciation of the types of head injuries that occur and a firm understanding of the treatment options. It is equally important to understand and recognize the constellation of signs and symptoms that diagnose a post-concussion syndrome. Prevention of the potentially fatal second-impact syndrome (SIS) by accurate assessment of the athlete who has suffered a concussion and ensuring the resolution of his signs and symptoms prior to his return to play is mandatory.4,5
Sports-related head injuries commonly are seen in the pediatric population. Children with mild head injuries comprise up to 93% of all head-injured children admitted to the hospital.6 As many as 20% of all pediatric head injuries have been reported to be sports related.7 As in the adult population, it is incumbent upon health care professionals, trainers, and coaches to properly identify the severity of a child’s head injury and provide the appropriate medical management before clearing him to return to competition.
Despite the high frequency of athletic-related head injuries in both the pediatric and adult populations, research on the topic is scarce.8-10 The fact that there is a dearth of Class I evidence (evidence provided by one or more well-designed randomized controlled clinical trials) attests to this. Management recommendations and current guidelines are based on Class II and Class III evidence only. At least 25 different guidelines for the evaluation of concussion have been published.1,11 Although there is a common thread in each of these guidelines, there is no uniform consensus as to which of the published guidelines is most appropriate.
This manuscript provides a review of athletic head injuries and suggested methods of grading of concussions. A method of sideline neurological assessment, including a mini-mental status exam, also is presented. Discussions of post-concussion syndrome and SIS, as well as current recommendations for return to competition, are included.
Epidemiology
The incidence of sports-related head injury varies regionally, and is influenced by the types of sports played (contact vs non-contact, organized vs non-organized, officiated vs non-officiated), the age of the population, and the existence of active injury prevention programs.
Sports are categorized by their probability for collision or contact.12 In "collision" sports (e.g., boxing, ice hockey, football, and rodeo), athletes purposely hit or collide with each other or inanimate objects, including the ground, with great force. In "contact" sports (e.g., basketball and soccer), athletes routinely make contact with each other or inanimate objects, but usually with less force than in collision sports. Efforts usually are not made to separate collision and contact sports, because there is no clear dividing line between them. In "limited-contact" sports (e.g., softball and squash), contact with other athletes or inanimate objects is infrequent or inadvertent. Some limited-contact sports (e.g., downhill skiing and gymnastics) can be as dangerous as contact or collision sports. The categorization, however, gives an idea of the comparative likelihood that participation in a particular sport will result in acute traumatic injuries resulting from blows to the body.12
Certain sports, in particular, have a higher incidence of head injuries. These include football, boxing, rugby, ice hockey, soccer, martial arts, equestrian sports, and wrestling.
In the United States, football injuries far exceed other sports injuries. Football, because of the number of participants and the nature of the game, has the highest incidence of head injuries. With approximately 1.5 million participants yearly and up to 20% of the players sustaining a concussion, the issue of appropriate management is not inconsequential.13,14 There are up to eight football-related head injury deaths each year in the United States.15
One group reported that 19% of high school athletes experience at least one minor head injury.16 Alarmingly, the author stated that 70% of the injured players returned to competition the same day as an injury that resulted in loss of consciousness.
The National Athletic Trainer’s Association (NATA) conducted a three-year study of the frequency, type, and severity of injuries in high school football for the 1986-1988 seasons.17 This study involved 351 teams with more than 21,000 players, 5260 games, and 27,288 practices. There were 12,786 injuries reported; 598 (4.7%) were identified as concussions.
Types of Athletic Head Injuries
Sports should contribute to the physical and mental health of children. Unfortunately, head injuries occur in sports and can cause permanent, irreversible damage to the central nervous system.18
Most acute head injuries are caused by a combination of rotational (angular) and translational (linear) acceleration, as well as the force of impact to the head.18 Rotational acceleration of the brain (caused by rapid turning of the head) can result in diffuse shearing forces deep in the brain, causing axonal injury. Rotational vectors applied to the head often produce injury in the brain at anatomical sites of fixation of the brain, particularly in the midbrain as it passes through the tentorial opening at the foramen magnum. Translational acceleration will cause tensile (pulling apart) and compressive forces, which usually result in skull fractures and injury to the adjacent structures (i.e., blood vessels, brain parenchyma, dura). Brain acceleration can occur without impact to the head; 35% of concussions in college football involved no impact to the head.18 Because adolescents are larger, faster, stronger, and more skilled at delivering a forceful impact than their younger counterparts, the incidence of head injury is higher in adolescents.18,19
Acute brain injuries can be divided into two categories: 1) focal brain injuries, including epidural hematomas (EDH) and subdural hematomas (SDH) as well as cerebral contusions; and 2) diffuse axonal damage, ranging from concussions to diffuse axonal injuries (DAI). DAI pathophysiologically results from shearing of white matter tracts from the cortex through the brainstem, producing coma in the most severe form. Recognition of focal brain injuries is crucial, because they potentially are the most life-threatening and require emergency transport and neurosurgical evaluation.20 The most common focal brain injury and etiology of sports-related fatality (87% of all head-related football fatalities) is the SDH.7,18,19
The most common sports-related head injury is the concussion, the syndrome characterized by immediate and transient impairment of neural function due to mechanical force.9,15,21 A concussion can occur even if there is no loss of consciousness (LOC).18 The most common signs and symptoms include confusion, memory loss (antegrade and retrograde), decreased level of consciousness, headache, slowed information processing, diminished attention span, and decreased coordination immediately or within minutes of the head injury.15,18
Repeat head injury is of special concern because the effects of repeated concussion now are being recognized as cumulative in nature.1,15,22-24 SIS results when a second concussive injury occurs prior to the resolution of symptoms from the first head injury.1,4 The mechanism of SIS is believed to be loss of vascular autoregulation, which may result in cerebral edema and increased intracranial pressure (ICP).23 Cognitive impairment and diminished neuropsychological functioning can result from repeated concussions.23,24 Sports-related mild traumatic brain injuries (MTBI) in still-developing young athletes can have significant long-term consequences involving cognitive, memory, and fine motor functions.25-27
Concussion. Derived from the Latin concussus ("a shaking"), concussion is the most common type of head injury that occurs in athletes. There is no universal agreement on the standard definition or nature of concussion.1,2,28 A frequently used definition of a concussion is a trauma-induced alteration in mental status that may or may not involve LOC.15,29
Concussions are sometimes described as MTBI.1,26 The American Congress of Rehabilitation Medicine has proposed this definition of MTBI: A traumatically induced physiologic disruption of brain function with at least one of the following: 1) any period of documented loss of consciousness; 2) memory loss of events just before or just after the injury event; 3) any alteration of mental state at the time of injury event; 4) focal neurologic deficits that may or may not be transient.30
There are several common features of concussions that help define the nature of the concussive head injury. The features of concussion as listed by one group include: 1) it is caused by either a direct blow to the head or elsewhere on the body with an "impulsive" force transmitted to the head; 2) it results in an immediate and short-lived impairment of neurologic function; 3) it may result in neuropathologic changes, although the acute clinical symptoms largely reflect a functional disturbance rather than structural injury; and 4) it may result in a graded set of clinical syndromes that may or may not involve LOC.31 The resolution of the clinical and cognitive symptoms typically follows a sequential course.
The hallmarks of cerebral concussion are confusion and amnesia.15,29 The athlete with a concussion may demonstrate easy distractibility and poor vigilance. He or she may be unable to maintain a coherent stream of thought or carry out a sequence of goal-directed actions. The confusion and memory disturbance can be of immediate or delayed onset, necessitating close observation of the head-injured athlete.29,32
Consciousness is a multifaceted function of the brain dependent on alertness and awareness of self and the environment. These functions likewise involve sensation, perception, memory, attention, and cognition. Consciousness is not localized to a specific brain region, but permeates the entire brain.33 Alteration of consciousness results when the integrity of the reticular activating system located throughout the brainstem is disrupted.33 Other anatomical areas involved in consciousness include the lamina terminalis and the anterior frontal lobe. Historically, grading of concussions had been based on the presence or absence of a loss of consciousness. By definition, an athlete does not have to experience a loss of consciousness to have suffered a concussion.29 Any immediate post-traumatic impairment of neural function, including an altered mental status, qualifies as a concussion.
Different schools of thought exist on grading the severity of concussion. (See Table 1.)1,2,34-37 Some classifications place greater emphasis on the duration of confusion and post-traumatic amnesia, while others place more emphasis on the presence of a loss of consciousness.28 All classifications of concussion are in agreement that the hallmarks of cerebral concussion are confusion and amnesia. No system of grading is foolproof.18 Often the history obtained from the athlete is distorted by the very presence of the head injury, which produces confusion of the specific detail of the injury and is compounded by the athlete’s willingness to under-report signs and symptoms in hopes of an earlier return to competition.
Recognition of a head injury is easy if the athlete has lost consciousness.4 It is much more difficult to recognize the far more frequent head injuries in which there is no loss of consciousness, but rather only a transient loss of alertness. More than 90% of all cerebral concussions fall into this mild category, in which there has not been an LOC but only a brief period of post-traumatic amnesia or loss of mental alertness.4 Because SIS can occur after a mild concussion, just as it can after a more serious head injury, it becomes important to recognize all grades of concussion.4,15
Attempts to qualify post-traumatic amnesia to determine the severity of head injury can be arduous. Post-traumatic amnesia (PTA) is the term used to describe the period following head injury in which the athlete is unable to remember. The duration of amnesia is determined by questioning the athlete after he or she has fully recovered. In practice, quantification of the duration of PTA can be unsatisfactory. Problems include the fact that it is determined retrospectively and depends on the athlete’s own judgment of the time memory returned and his or her recollections of the associated events which allow it to be timed. Consideration of the duration of post-traumatic disorientation has been considered as an alternative to post-traumatic amnesia; however, research studies have not found the two to be coterminous. Other problems associated with determining PTA include variability from one examiner to another; whether PTA estimates include the time elapsed since the injury or time from clinical assessment; and variability of estimates from the athlete, if he or she is questioned more than once. Head-injured athletes commonly will experience a return of "islands of memory" before the return of continuous memory. Estimates of PTA duration made in the first hours after the injury have been reported to change in more than 25% of cases when athletes were interviewed after complete recovery.38
The importance of careful questioning to establish the precise return of continuous memory cannot be over-estimated. One group hypothesizes that there are two phases in the amnestic changes due to concussion; one occurs immediately after impact, and the second phase develops up to an hour later.39 The return of "memory islands" could represent recovery of the first phase before the second has developed. Explanations of the second phase are speculative; however, localized cortical edema and biochemical changes have been proposed. "Islands of memory," as described by one research team, are considered to occur when a strong stimulus is applied during recovery from the immediate injury.40
A mild cerebral concussion does not result in an LOC. Athletes often have confusion and amnesia and can be distracted easily, demonstrating an inability to focus their attention and carry out goal-specific tasks. They often continue to play, as their gross motor skills usually are not impaired. This particular type of head injury is difficult to diagnose unless the athlete complains of symptoms, or a vigilant team of health care providers appreciates the occurrence of a head injury, often through an altered mental status.
A classic cerebral concussion is associated with a transient loss of consciousness. Unconsciousness occurs at the time of impact and recovery occurs within minutes. After regaining consciousness, athletes often will be confused and amnestic and can complain of headache, nausea, dizziness, and visual changes. Neuropsychological signs and symptoms that often are present include poor concentration, reduced attention span, reduced capacity to process information, and difficulty in integrative and abstract thinking. Unless the athlete is observed, questioned, and examined, a team physician or trainer could easily be misled that the athlete has had a complete recovery. Physically, the player may demonstrate nothing more than a vacant stare and some minor motor incoordination. It is imperative that an athlete with this type of injury not be allowed to return to competition because of the increased risk of re-injury and potential for development of SIS.28
Returning an athlete to competition following a head injury is determined by the severity of the injury and the history of previous head injuries. This implies the need for some form of medical record for each and every athlete that documents a history of antecedent injury. Studies have demonstrated that a player who has suffered a concussion has a four times greater likelihood of having a second one, when compared to the athlete who has never had a concussion.34
Generally, the decision to return the athlete to active competition will be based on several factors, including:
- Presence of head injury;
- Presence of LOC;
- The length of the LOC;
- The presence of altered mental status (i.e., confusion, agitation, disorientation);
- The presence and length of amnesia;
- A period of observation and re-evaluation;
- The clearance of all concussive symptoms and sensorium; and
- A medical history with no previous head injuries or concussions.
In 1986, Robert Cantu proposed a set of guidelines for the safe return to competition for athletes who have suffered a concussion.35,41 (See Table 2.) His guidelines, which have become widely accepted, are based on a grading of the concussion that is determined by the presence or absence of a loss of consciousness, the length of time of unconsciousness, and by the presence and length of post-traumatic amnesia. Numerous other classifications and guidelines for return to competition have subsequently been published. The Colorado Medical Society and the American Academy of Neurology guidelines are two that have been well accepted. It is important that one system be adopted and utilized by a team and that records are maintained on each individual player suffering a traumatic brain injury. The effect of concussion can be cumulative and if return to competition occurs too early, it can render the athlete vulnerable to repeat injury.22
Recognizing and managing Grade 2 and Grade 3 level concussions (per any grading system) require removal from the game or practice and a period of observation and retesting before return to competition. Generally, return to competition after concussion must be deferred until all symptoms have abated and diagnostic studies are normal.28 Head computed tomography (CT) may be required if neurological symptoms continue. In the pediatric population, those who have suffered a sports-related head injury with an associated LOC; are amnestic at the time of evaluation; or who have continued headache, vomiting, or focal neurological deficit have a prevalence of intracranial injury detectable on CT that ranges from 0-7%.10
After any form of concussion, continued headache or associated concussive symptoms would require further evaluation and CT scanning. Any CT-documented post-traumatic pathology (i.e., contusion, hemorrhage, or edema) would conclude the player’s season.
Post-Concussion Syndrome. Patients with minor head injuries may continue to have residual complaints stemming from their initial concussion.8 Symptoms such as continued headache (especially with exertion), nausea, vertigo, dizziness, irritability, impaired memory, and impaired concentration and attention that fail to resolve after a head injury may represent a post-concussion syndrome.18,28
Proposed diagnostic criteria for the diagnosis of a post concussion syndrome have been published in the Diagnostic and Statistical Manual (1994) of the American Psychiatric Association (DSM-IV). The DSM-IV proposal criteria requires that two of three major criteria be present for the diagnosis of a post concussion syndrome. However, a significant number of concussions of the mild to moderate type (Cantu/Colorado classification) would not satisfy the DSM-IV criteria and, therefore, would not be eligible for the diagnosis of a post-concussion syndrome. Perhaps the presence of continued signs and symptoms after head injury should support a diagnosis of post-concussion syndrome.
Physicians and trainers should be alerted to continued complaints and symptoms in the head-injured athlete. Referral for further neurological evaluation and, possibly, imaging is recommended. Formal neuropsychological assessment can be beneficial in managing these patients.22 A large number of patients with a post concussion syndrome have no neurological deficits on clinical examination, yet their symptoms can be disabling and may preclude them from participation in sports. Neuropsychological testing can detect subtle but significant cognitive abnormalities with much greater sensitivity than a standard neurological examination.24
Second-Impact Syndrome. SIS refers to a condition in which a fatal brain swelling, at times subclinical, can develop after a minor head injury in an athlete who still is symptomatic from a previous concussion.4,28,32,42,43 What one group44 called the "second-impact syndrome of catastrophic head injury" in 1984 was first described in 1973.4,45 SIS underscores the need for strict adherence to return to competition guidelines, circumventing this potentially catastrophic occurrence.
Typically, the athlete suffers post-concussion symptoms after the first head injury. These may include headache, labyrinthine dysfunction, visual, motor, sensory changes, or mental difficulty, especially thought and memory process.4 Before these symptoms resolve, which may take days to weeks, the athlete returns to competition and receives a second blow to the head. Affected athletes may appear stunned, but usually remain on their feet. What happens in the next seconds to minutes sets this syndrome apart from a concussion or even a SDH.4,28 The athlete, conscious yet stunned, quite precipitously collapses to the ground, semicomatose with dilating pupils, loss of eye movement, and evidence of respiratory failure or apnea.28
Pathophysiologically, it is believed that subclinical brain edema from a previous head injury renders the brain more susceptive to further injury, even minor in nature. Current understanding of this syndrome is that the initial injury/concussion deranges the brain’s autoregulatory and metabolic systems enough to produce vascular engorgement and poor brain compliance, allowing for marked changes in ICP with small changes in intracranial volume.4,32 Brain compliance refers to the intracranial relationship of volume change to pressure change. Essential to this discussion is the fact that during the minutes to few days after concussion injury, brain cells that are not irreversibly destroyed remain alive but exist in a vulnerable state. This concept of injury-induced vulnerability describes the fact that patients suffering from head injury are extremely vulnerable to the consequences of even minor changes in cerebral blood flow and increases in ICP and apnea.32 When head injury occurs, major compensatory mechanisms are set into action to accommodate for any increase in intracranial volume. If the limits of these compensatory mechanisms are exceeded, ICP begins to rise; a substantial increase in pressure with any subtle change in volume occurs. This increased ICP can result in herniation, cerebral ischemia, and brain death.43,46
The risk factors for SIS currently are not understood. Limited knowledge suggests that children and adolescents are at higher risk; hence, increased clinical vigilance may be necessary after all head injuries in this age group.43
Approximately 50 cases of SIS have been reported since 1980. The National Institute for Catastrophic Sports Injury Research reported 35 football-related cases between 1980 and 1993.4
The treatment of SIS should be prevention by adherence to return-to-competition guidelines after an initial head injury. Any athlete sustaining a second head injury prior to the resolution of symptoms from the antecedent injury has the potential to develop SIS.4,32 An athlete who is symptomatic from a head injury must not participate in contact or collision sports until all cerebral symptoms have subsided, and preferably for at least one week after. Whether it takes days, weeks, or months to reach the asymptomatic state, the athlete must never be allowed to practice or compete while still suffering post concussion symptoms.32
Recognition of the condition on the field and initiating measures to reduce ICP is indicated. This form of head injury should be managed as a severe head injury, including control of the airway and rapid sequence intubation.9 If signs of raised ICP are apparent, or there is clinical evidence of herniation, hyperventilation and intravenous administration of mannitol should be considered until more definitive treatment is available at a medical facility. Prevention of hypotension and hypoxia is crucial. Rapid transport to a hospital with neurosurgical capabilities is mandatory.
Diffuse Axonal Injury. Diffuse axonal injury (DAI) is most common in victims of motor vehicle accidents but occasionally is seen in severe athletic-related head trauma. Severe DAI unaccompanied by a mass lesion occurs in almost half of patients with severe head injury and is responsible for one-third of all head-injury-related deaths.15 It is the most common cause of persistent vegetative state and significant disability following head injury.
DAI is believed to be caused by angular or rotational forces applied to the head that result in a shearing type injury that stretches and tears axons diffusely.1,47 When the reticular activating system of the brainstem is disrupted, consciousness is lost. Unconsciousness also can be produced by a diffuse injury to both cerebral hemispheres. The cerebral impairment may be so severe that the respiratory drive is affected, and the athlete hypoventilates or becomes apneic, hypoxic, and hypercapnic.47,48 The extent of apnea is directly related to the amount of energy transmitted to the brainstem.48
The number of axons injured and degree of edema increase with the traumatic force. Less severe axonal injury is reversible; more severe injury can be permanent.47
Cerebral concussion is considered a mild form of DAI. Magnetic resonance imaging (MRI) can be helpful in demonstrating characteristic lesions (tissue tear hemorrhages) commonly associated with more severe forms of DAI; however, it does not determine the severity of DAI, which remains a clinical determination.
Intracranial Hemorrhage. Intracranial hemorrhage is the most common cause of death in athletes.28 The four types of primary intracranial hemorrhages are epidural hematoma (EDH), SDH, intraparenchymal hematoma, and subarachnoid hematoma (SAH).
An athlete who has sustained severe head trauma can develop any form of intracranial hemorrhage. SAH is the most common post-traumatic hemorrhage; however, acute SDH is the most lethal and is the most common cause of death in athletes.
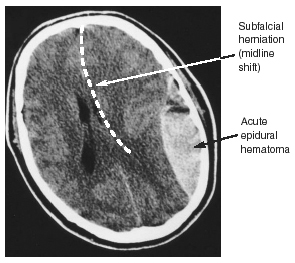
Epidural Hematoma. EDH is a hemorrhage that occurs between the periosteal layer of the dura mater and the skull. EDHs often are associated with skull fractures, usually are arterial in origin, and most commonly occur in the middle cranial fossa. The high incidence in the middle cranial fossa arises from the fact that the middle meningeal artery is located close to the squamous temporal bone, which easily fractures with trauma. The bony fragments can tear the vessel, resulting in an EDH. (See Figure 1.)15
|
An EDH usually is the most rapidly progressing intracranial hematoma; it may reach a fatal size in 30-60 minutes.28 The athlete may have a lucid interval, although this does not always occur. Thus, the athlete initially may remain conscious or regain consciousness after the head trauma and then experience an increasing headache and progressive decline in level of consciousness. This occurs as the clot accumulates and the ICP increases. This lesion, if present, almost always will declare itself within 1-2 hours from the time of injury.20,28 Usually, the brain substance is free from direct injury; thus, if the clot is evacuated promptly, full recovery may be expected.
Subdural Hematoma. SDHs are located between the dura mater and the arachnoid and usually are crescentic-shaped and associated with a high mortality. Athletes who suffer a severe impact at the time of injury generate brain acceleration within the skull, with over-stretching and rupture of the parasagittal bridging veins. Unlike EDH, with this injury there often is associated injury to the brain tissue.
An acute SDH generally becomes apparent immediately following impact to the head.20 After contact to the head, or in some instances a blow to another part of the body that shakes the brain sufficiently, the athlete becomes disoriented, nauseated, and loses consciousness. In severe cases, the athlete develops posturing and may have pupillary changes. These patients need immediate treatment, hospitalization, and, often, surgical intervention.
The majority of SDHs are supratentorial in location and most commonly are found in the frontoparietal region. (See Figure 2.) The high degree of mortality associated with an acute SDH, even those treated surgically, arises from the significant amount of associated underlying brain injury.15,28,41 This underscores the need to rapidly transport severely head-injured athletes to hospitals with neurosurgical capabilities to diagnose and surgically evacuate those with significant mass effect. This form of intracranial hemorrhage usually renders an athlete unconscious from the time of impact, and emergent resuscitation may be necessary.28 Improved outcome has been achieved by resuscitation, rapid transport, and early surgery (within four hours of injury).18
|
Intraparenchymal Hemorrhage. This usually is a well-defined hematoma within the brain parenchyma that occurs post-traumatically as a result of a disruption of a cerebral blood vessel. Progression in size or severity of the hemorrhage occurs in up to 30% of patients within 24 hours.28
Differentiation from a hemorrhagic contusion can be difficult, owing to the fact that contusions can evolve and coalesce into a collection of blood. The mechanism of injury is acceleration of the brain within the calvarium occurring at the time of impact, resulting in disruption of one or more parenchymal vessels. (See Figure 3.)
|
Subarachnoid Hematoma. Extravasation of blood into the subarachnoid space may appear as a high density collection within the cerebrospinal fluid spaces, including sulci, cisterns, and fissures. The irritative properties of the blood may precipitate a seizure. CT demonstration of post-traumatic SAH is limited to a few days as a result of erythrocyte lysis and rapid absorption. SAH in excess of the degree of trauma may signify an underlying brain anomaly (i.e., aneurysm or arteriovenous malformation).28,41 If clinical suspicion exists, further investigation may be indicated.
Cerebral Contusion. A cerebral contusion, or bruising of the brain, usually is cortical in location.49 It represents a combination of necrosis, hemorrhage, infarction and edema of the brain involved. Cortical contusions usually are direct coup or contrecoup injuries that occur when the brain impacts against the bony prominences of the skull. Contusions commonly involve the inferior aspect of the frontal lobes and the anterior temporal lobes, where they lie buttressed against the greater wing of the sphenoid bone. Signs and symptoms of contusion are unconsciousness, disturbance in strength or sensation, changes in visual awareness, or focal neurologic signs such as seizures.
Emergency Sports Head Injury Assessment
After an athlete is injured, the examiner must take control of the situation, both on the field during the immediate post-injury period and on the sideline subsequent to transport off the field. A systematic head-to-toe evaluation should be completed. Proper cervical spine precautions should be exercised, and a cervical spine injury must be assumed until proven otherwise, especially in anyone who has had an LOC or has a post-traumatic altered mental status.18 In dealing with a helmeted unconscious athlete, the helmet should be left in place until adequate assistance is available and insurance that a medical team familiar with a technique for removal of helmets is in place. Those providing medical coverage at athletic events can develop and practice the safe removal of helmets in injured athletes with available protocols. (See Table 3.) Sports medicine experts advise against removal of the helmet in the field, to prevent neurological injury. Removal of the helmet is a high-risk maneuver, and when performed by an inadequately trained medical staff can lead to further neurological injury.50,51 One study estimated that up to 25% of spinal cord injuries occur after the initial traumatic event, during transfer and early management.52 If cardiopulmonary resuscitation is necessary, removal of the face mask will allow access to the airway.
|
Common situations that increase morbidity and mortality in the injured athlete include airway obstruction, respiratory failure, cardiac arrest or arrhythmia, severe head injury, cervical spine injury, hyperthermia, and coagulopathy.
Proper assessment and management of head-injured athletes require adherence to guidelines presented in the Advance Trauma Life Support (ATLS) protocols prepared by the American College of Surgeons Committee on Trauma. As recommended, these guidelines include the primary survey, resuscitation, a secondary survey, and re-evaluation and definitive care.
The key to assessment of vital signs is to constantly be vigilant for change from baseline values. Be aware of trends in parameter changes (i.e., How has it changed? What does the change imply?).
The respondent’s initial obligation is to determine whether the injured player is breathing spontaneously, has an unobstructed airway, and has a pulse. Second, medical personnel should quickly determine whether further evaluation on the sidelines is appropriate or whether emergent transport to a hospital is needed. If the athlete has an adequate airway, respiration, and pulse, the initial evaluation of the level of consciousness should be performed in the position in which the athlete lies.
In the absence of a pulse and adequate respiration, the neck should be stabilized by an experienced person. With the assistance of two or three trained personnel, the athlete may be log-rolled into a supine position so that cardiopulmonary resuscitation can be initiated effectively.
Athletes with head injuries frequently have a blank expression, may appear confused, exhibit delayed verbal responses, and seem emotionally labile.32 The standard method of assessing the level of consciousness is by establishing a Glasgow Coma Score (GCS). By observing the patient’s eyes and motor and verbal responses, one can quantify the level of consciousness. A GCS of 13 or greater is classified as a mild head injury and usually has an excellent prognosis for recovery. By far, the most common sports-related head injury is the mild variety known as concussion.15 Some authors have objected to the term "mild head injury," stating that no injury to the brain should be considered minor.2,41,53 On the other hand, a GCS of 8 or less is considered severe.
Management of Concussion
The guidelines for the management of concussion in sports adapted by the American Academy of Neurology (AAN) specifically called for the development of a standardized, systematic sideline evaluation for the immediate assessment of concussion in athletes.37,54 The AAN guidelines, in line with the concussion literature, stress that a sideline examination should test orientation and probe for deficits in attention, concentration, and memory.54 (See Table 4.)
|
The player also should be questioned about the symptoms of dizziness, light-headedness, vertigo, blurring or double vision, photophobia, ringing in the ears, headache, nausea, and vomiting. Many of these symptoms may be present initially after an acute head injury, while headache, nausea, and vomiting may not become evident for several minutes after the precipitating trauma. Vomiting is not very common after athletic injuries, but when it is present, it suggests significant injury with elevated ICP.
A player initially should be observed for a minimum of 15 minutes on the sidelines and reevaluated as needed. If any symptoms develop, the athlete should not return to competition that day. If the player has not lost consciousness, is oriented, and is asymptomatic, provocative testing should be performed to determine whether symptoms will occur with physical stress. (See Table 4.)
The following recommendations for management of concussion are based on the AAN guidelines.37,53 Recommendations by Cantu and the Colorado Medical Society have been discussed and are presented in Table 2.
Grade 1 Concussion. Grade 1 concussions are defined by symptoms of transient confusion without amnesia, no LOC, and concussion symptoms and/or mental status abnormalities that resolve in fewer than 15 minutes. This is both the most common and most difficult form of concussion to recognize, as the individual is not rendered unconscious and experiences only momentary confusion. The majority of concussions sustained in sports and recreational activities are this type. Although this type of concussion is often downplayed and referred to in terms of "being dinged" or "having their bell rung," an athlete who sustains a Grade 1 concussion should be removed from the game and reevaluated before reentering the playing area.
A second Grade 1 concussion on the same day will result in the player being removed from the contest for the remainder of the day and undergoing evaluation by a physician. It also is recommended that a player who has sustained three Grade 1 concussions not be allowed to return to play until he or she is symptom-free for at least one week. In addition, no further contact sports are permitted for at least three months, and then only if the individual is asymptomatic at rest and with exertion. CT or MRI scanning is recommended in all instances in which headache or other associated symptom either worsens or persists longer than one week after the concussion.
Grade 2 Concussion. Grade 2 concussion is defined by the presence of transient confusion with amnesia and concussion symptoms and/or mental status abnormalities lasting more than 15 minutes, although there is no LOC. With this type of concussion, the individual exhibits confusion and may have post-traumatic amnesia of the events following the impact. In more severe cases, the individual may experience retrograde amnesia of events preceding the injury. After an individual has sustained a Grade 2 concussion, he or she should be removed from play and not allowed to return to the playing area.
After the first Grade 2 concussion, the individual should refrain from playing any contact sport for at least one week, again only after the player is asymptomatic at rest and during exertion. Additionally, a physician should perform a neurological exam before the individual is allowed to return to play. If the individual experiences worsening headaches and other associated symptoms, and/or these symptoms last longer than a week, a CT or MRI is recommended. Return to contact play after a second Grade 2 concussion should be deferred for at least two weeks or, in most cases, a month. After three or more Grade 2 concussions, the individual seriously should consider terminating play for the remainder of the season, and perhaps beyond when any abnormality (i.e., brain swelling or contusions) appears on the CT or MRI scan.
Grade 3 Concussion. It usually is quite easy to recognize a Grade 3 concussion, and this level of concussion is applied to anyone who experiences LOC no matter how brief. Initial treatment for Grade 3 concussion—the most severe and serious of the grades—calls for the individual to be transported to the nearest hospital for neurological evaluation and observation.
One month should be the minimum period the individual is barred from contact sports after sustaining a Grade 3 concussion. With multiple Grade 3 concussions, the individual must remain out of play for the remainder of the season and should be strongly discouraged from returning to playing any contact sports.
Management of Moderate and Severe Head Injury
The priority in managing the patient who has moderate (GCS 12-9) or severe (GCS < 8) head injury is to minimize secondary brain injury, with evaluation and treatment occurring simultaneously. Maintenance of adequate hemodynamics and oxygenation are of utmost importance. If hypoxic or ischemic injury occurs in addition to the traumatic injury, the prognosis worsens.47,55 The ABCs (airway, breathing, circulation) of emergency medical care apply as in every life-threatening situation. Endotracheal intubation and mechanical ventilation should be performed in patients who have a GCS of 8 or less, hypoventilation, apnea, cardiorespiratory arrest, or other significant injury.55,56 Hypoxia and hypercarbia should be avoided through the use of supplemental oxygen and controlled ventilation, because even mild-to-moderate hypoxia or hypercarbia can affect cerebral blood flow and result in further brain injury. Patients who exhibit signs of impaired cardiac output, such as tachycardia or borderline or low blood pressures, should receive a bolus of isotonic fluid intravenously to ensure adequate circulating volume to maintain blood flow to the compromised brain. The neurologic status of the patient must be followed during the period of resuscitation using the GCS to evaluate the response to therapy. The use of hyperventilation (PCO2 of 30-35 torr) and mannitol (0.25-0.50 mg/kg) is appropriate for patients in whom herniation is impending until the neurologic evaluation is completed and the patient is stabilized. Seizures are common after traumatic and hypoxic brain injury and should be treated with benzodiazepines, phenytoin, and phenobarbital as needed.
After initial evaluation and stabilization, all athletes who have moderate or severe head injury require CT of the head. Significant SDH or EDH requires urgent or emergent evacuation to prevent secondary injury. Severe cerebral edema identified by CT may require placement of an ICP monitor, which necessitates consultation with a pediatric neurosurgeon. In the patient whose mental status is altered, there is a significant possibility of a spinal cord injury that requires appropriate immobilization. Spinal cord immobilization must be continued until proper evaluation is completed.
Conclusion
Head injuries in sports cause acute—and in some instances long-term—serious problems. The symptoms of mild head injury may be transient, but the cumulative effect may have permanent sequelae. Appropriate acute and subacute management can prevent secondary potentially disabling or fatal injury.
It is essential that all individuals who participate in sports and recreational activities take into consideration the risk of traumatic brain injury and make every effort to prevent such potentially catastrophic injury. Physicians, athletic trainers and coaches must work together as partners and become attuned to the problems and recognize even the mildest forms of concussion in athletes. Most importantly, athletes need to be educated and aware of the recognition and management of concussions so they can participate in their own care from an informed perspective.
References
1. Landry GL. Central nervous system trauma: Management of concussions in athletes. Pediatr Clin N Am 2002;49:723-741.
2. Poirier MP, Wadsworth MR. Sports-related concussions. Pediatr Emerg Care 2000;16:278-283.
3. Perriello VA, Barth JT. Sports concussions. Contemp Pediatr 2000;17:132-140.
4. Cantu RC. Second-impact syndrome. Clin Sports Med 1998;17:37-44.
5. Loiselle JM, Poirier MP, Schutzman S. Closed head injury in children. Pediatr Emerg Care 2002;18:48-52.
6. Moynihan JA, Perkin RM. Current concepts in the management of minor closed head injury in children. Trauma Reports 2001;2:1-12.
7. American Academy of Pediatrics, Section on Sports Medicine and Fitness. Guidelines for Pediatricians: Head Injuries. Sports Shorts 2000;1:1.
8. Macciocchi SN, Barth JT, Littlefield LM. Outcome after mild head injury. Clin Sports Med 1998;17:27-36.
9. Bernhardt DT. Football: A case-based approach to mild traumatic brain injury. Pediatr Ann 2000;29:172-176.
10. American Academy of Pediatrics. The management of minor closed head injury in children. Pediatrics 1999;104:1407-1415.
11. McCrory PR. Were you knocked out? A team physician’s approach to initial concussion management. Med Sci Sports 1997;29:207-212.
12. American Academy of Pediatrics, Committee on Sports Medicine and Fitness. Medical conditions affecting sports participation. Pediatrics 2001;107:1205-1209.
13. Barth J, Alves W, Ryan T, Macciocch S, et al. Mild Head Injury in Sports: Neuropsychological Sequelae and Recovery of Function. In: Levin H, Eisenberg H, Benton A, eds. Mild Head Injury. New York: Oxford Press; 1989: 257-275.
14. Buckley W. Concussion in college football: A multivariate analysis. Am J Sports Med 1988;16:51-56.
15. Warren WL, Bailes JC. On the field evaluation of athlete head injury. Clin Sports Med 1998;17:13-26.
16. Gerberich SG, Priest JD, Boen JR, et al. Concussion incidences and severity in secondary school varsity football players. Am J Public Health 1983;73: 1370-1375.
17. Bailes JE, Lovell MR, Maroon JC. Sports Related Concussion. St. Louis: Quality Medical Publishing, Inc.; 1999:1.
18. Chorley JN. Sports-related head injuries. Curr Opin Pediatr 1998;10:350-355.
19. Mueller FO. Fatalities from head and cervical spine injuries occurring in tackle football: 50 years’ experience. Clin Sports Med 1998;17:169-182.
20. Lackstead EF, Patel DR. Catastrophic pediatric sports injuries. Pediatr Clin N Am 2002;49:581-591.
21. Davis PM, McKelvey MK. Medicolegal aspects of athletic head injury. Clin Sports Med 1998;17:71-82.
22. Collins MW, Lovell MR, McKeay DB. Current issues in managing sports-related concussion. JAMA 1999;282:2283-2285.
23. Genuardi FJ, King WD. Inappropriate discharge instructions for youth athletes hospitalized for concussion. Pediatrics 1995;95:216-218.
24. Collins MW, Grindel SH, Lovell MR, et al. Relationship between concussion and neuropsychological performance in college football players. JAMA 1999; 282:964-970.
25. Patel DR, Pratt HD, Greydanus DE. Pediatric neurodevelopment and sports participation. When are children ready to play sports? Pediatr Clin N Am 2002;49:505-531.
26. Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA 1999;282:958-963.
27. Ponsford J, Willmott C, Rothwell A, et al. Impact of early intervention on outcome after mild traumatic brain injury in children. Pediatrics 2001;108: 1297-1303.
28. Proctor MR, Cantu RC. Head and neck injuries in young athletes. Clin Sports Med 2000;19:693-715.
29. Kelly JP, Rosenberg JH. Diagnosis and management of concussion in sports. Neurology 1997;48:575-580.
30. Kay T, Harrington DE, Adams R, et al. Definition of mild traumatic head injury. J Head Trauma Rehabil 1993;8:86-87.
31. Johnston KM, McCrory P, Mohtadi NG, et al. Evidence-based review of sport-related concussion: Clinical science. Clin J Sport Med 2001;11:150-159.
32. Wojtys EM, Horda D, Landry G, et al. Concussion in sports. Am J Sports Med 1999;27:656-687.
33. Zeman A. Consciousness. Brain 2001;124:1263-1289.
34. Roos R. Guidelines for managing concussion in sports. Phys Sports Med 1996;24:67-74.
35. Cantu RC. Guidelines for return to contact sports after a cerebral concussion. Phys Sports Med 1986;14:75-83.
36. Colorado Medical Society. Report of the Sports Medicine Committee: Guidelines for the Management of Concussions in Sports (revised). Denver:Colorado Medical Society;1991:1.
37. American Academy of Neurology. Practice parameter: The management of concussion in sports (summary statement). Neurology 1997;48:581-585.
38. Gronwall D, Wrightson P. Duration of post-traumatic amnesia after mild head injury. J Clin Neuropsychology 1985;2:51-60.
39. Gronwall D, Wrightson P. Memory and information processing capacity after a closed head injury. J Neurol Neurosurg Psychiatry 1981;44:889-895.
40. Russell WR, Nathan PW. Traumatic amnesia. Brain 1946;69:280-300.
41. Cantu RC. Return to play guidelines after a head injury. Clin Sports Med 1998;17:45-60.
42. Clarke KS. Epidemiology of athletic head injury. Clin Sports Med 1998;17:1-11.
43. McCrory PR, Berkoric SF. Secondary impact syndrome. Neurology 1998;50: 677-683.
44. Saunders RL, Harbaugh RE. The second impact in catastrophic contact sports head trauma. JAMA 1984;252:538-539.
45. Schneider RC. Head and Neck Injuries in Football: Mechanisms, Treatment and Prevention. Baltimore:Williams and Wilkins;1973.
46. Cantu FL, Voy R. Second impact syndrome: A risk in any contact sport. Phys Sports Med 1995;23:27-34.
47. Gedeit R. Head injury. Pediatr Rev 2001;22:118-123.
48. Atkinson JLD. The neglected pre-hospital phase of head injury: Apnea and catecholamine surge. Mayo Clin Proc 2000;75:37-47.
49. Zuckerman GB, Conway EE. Accidental head injury. Pediatr Am 1997;26: 621-632.
50. Swenson T, Lauerman N, Blanc R. Cervical spine alignment in the immobilized football player: Radiographic analysis before and after helmet removal. Am J Sports Med 1997;25:226-230.
51. Warren WL, Bailes JE. On the field evaluation of athletic neck injury. Clin Sports Med 1998;17:99-110.
52. Podolsky S, Baratt LJ, Simon PR, et al. Efficacy of cervical spine immobilization methods. J Trauma 1983;23:461-465.
53. Stein SC. Minor head injury: 13 is an unlucky number. J Trauma 2001;50: 759-760.
54. McCrea M, Kelly JP, Kluge J, et al. Standardized assessment of concussion in football players. Neurology 1997;48:586-588.
55. Perkin RM, Moyniham JA, McLeary M. Current concepts in the emergency management of severe traumatic brain injury in children. Trauma Reports 2000;1:1-16.
56. Kaide CG, Hollingsworth JC. Current strategies for airway management in the trauma patient. Trauma Reports 2003;4:1-12.
Pediatric athletic head injuries are a significant problem, especially for emergency medicine physicians. The dedication of many young athletes to performance and their avoidance of restrictions makes it imperative that ED physicians recognize and give appropriate recommendations to parents and coaches of young athletes. The cumulative damage that may result from repetitive minor head trauma is not recognized by the majority of athletes, and the ED physician has the burden of conveying these potential risks to the family. This article provides a comprehensive review of sports-related head injuries and recommendations on grading of concussions, imaging, and the safe return of the athlete to competition.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.