Burn Management in Pediatric Patients
Authors:
Perry Stafford, MD, FACS, FAAP, FCCM, Professor of Surgery, UMDNJ–Robert Wood Johnson Medical School; Chief of Pediatric Surgery, Robert Wood Johnson University Hospital, New Brunswick, NJ
Terrence Curran, MD, Chief Resident, Robert Wood Johnson University Hospital, New Brunswick, NJ
Peer Reviewer:
Richard J. Cartie, MD, Director, Pediatric Critical Care Services, Joseph M. Still Burn Center, Inc., Augusta, GA.
Burn injuries account for half a million visits to the emergency department each year and present numerous challenges in management. The spectrum of burn injuries is immense, ranging from simple first-degree burns with no sequela to third-degree burns with hypermetabolic response. In addition, pediatric patients add unique challenges to providing optimal care.
For more severe burn injuries, the initial management focuses on early recognition of potential airway and circulatory compromise and adequate resuscitation. Although many small superficial burns may be managed successfully as an outpatient, burn evolution can lead to burns converting to a higher severity after several days; frequently a burn specialist is needed for pediatric patients. Current management has changed from daily dressing changes with silvadene to debridement, skin substitutes, and silver dressings that stay in place for 7 days. Successful burn management demands an understanding of the epidemiology, pathophysiology, initial resuscitation, associated injuries, and social concerns for each child, which are comprehensively reviewed in this article.
The Editor
Epidemiology
The American Burn Association National Burn Repository provides a detailed report of the severe burn injury cases in the United States. During a 10-year period from 2000-2010, there were 148,419 cases of acute burn injuries requiring admission to burn centers.1 Additionally, more than 500,000 burns require medical treatment every year.2 Burn injuries can be the result of exposure to a flame as in a house fire, scalding injuries, contact with hot objects, electricity, and chemical or radiation exposure. Males were more likely to be victims of burn injuries in all pediatric age groups.
More than 50% of cases had burn injuries encompassing less than 10% of total body surface area (TBSA). A little more than 1% of cases had burns over more than 50% of TBSA. Only 3.7% of burn victims admitted to burn centers die from their injuries. The lethal area (LA) 50 is about 70% TBSA. Major predictors of mortality are age (the very young and very old are at greater risk), TBSA burned, and inhalation injury. Every day, 435 children between ages 0 to 19 are treated in emergency departments for burn-related injuries and two children die as a result of being burned.3 The majority of minor burn injuries are treated successfully by the emergency department (ED) physician with outpatient follow-up.
Flame or flash burns account for nearly half of all burn injuries in the United States. Scalds, which account for the most common etiology of burn in patients younger than 5 years of age, are the second most common type of burn injury among all age groups. The severity of the burn is proportional to the temperature of the liquid, grease, or oil. Scalds by grease or water heated in a microwave have much greater severity and have a higher incidence of conversion to third-degree burns. (See Table 1.) Contact burns are generally small in size but can vary greatly in depth. Chemical and electrical burns are less common but can be extremely devastating injuries.

Pathophysiology and Etiology
The pathophysiology of a burn injury is complex and a basic knowledge of skin anatomy and physiology, burn classification, and the body's response to severe burns is required to successfully manage burn victims.
The anatomy of the skin helps explain the classification of burns. The skin has many functions, such as maintenance of fluid and electrolyte balance, protection against infection, and thermoregulation and metabolic functions. The skin is divided into three layers: the epidermis; the dermis, which is further divided into the papillary layer and the reticular layer; and the subcutaneous level. (See Figure 1.)

The epidermis is arranged in five layers: the stratum basale, the stratum spinosum, the stratum granulosum, the stratum lucidum, and the stratum corneum. The main cell is the keratinocyte; other cells include melanocytes, Langerhans cells (which are involved in the immune function of the skin), and Merkel cells (which are responsible for fine touch).
The dermis is a more complex layer of skin that is broken down into the papillary layer and the reticular layer. The fibroblast, which is the main cell of the dermis, is responsible for the synthesis and degradation of proteins.
The subcutaneous tissue is the connective tissue that contains free nerve endings and root hair plexuses.
The initial burn injury causes a coagulation necrosis of the epidermis and the extent of the burn depends on the factors associated with the exposure, such as temperature, duration, and specific heat of the burn agent.
The three zones of a cutaneous burnthe zone of coagulation, the zone of stasis, and the zone of hyperemiawere described first by Jackson in 1953 and represent the local inflammatory response.
The zone of coagulation marks the epicenter of the injury and the cells in this area suffer irreversible damage. This tissue eventually turns into the initial burn eschar. The zone of stasis surrounds the zone of coagulation and the cells in this area initially are viable, but their survival depends on adequate resuscitation. The zone of hyperemia is indicative of vasodilation and increased blood flow to the area.
The local injury disrupts the skin barrier and leads to many burn-related complications, such as infection, heat loss, alterations in feelings and sensations, and evaporative water loss.4
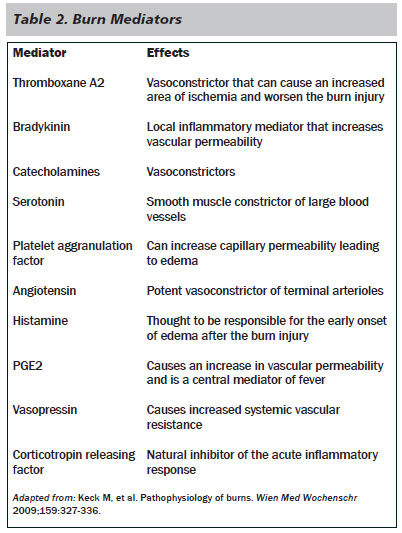
In burns encompassing more than 30% of the TBSA, a systemic inflammatory reaction may accompany the local inflammatory reaction. During this phase, there is a systemic release of proinflammatory mediators such as thromboxane A2, bradykinin, PGE2, catecholamines, serotonin, oxygen radicals, platelet aggranulation factor, angiotensin II, and others, which lead to the development of "burn shock." (See Table 2.)
Burn shock is typically the sequela of large burns (> 20% TBSA) from a hypermetabolic reaction secondary to release of the proinflammatory mediators discussed previously. Systemic effects include increased cardiac output, decreased renal blood flow (renal failure), and intestinal ischemia resulting in translocation of bacteria from the ischemic gut that eventually may cause sepsis from bacteremia. The hypermetabolic response also results in an increased body temperature, increased oxygen requirements, increased glucose consumption, proteolysis, and lipolysis.5 In addition, severe burn injury causes a global immunosuppression that leads to an increased risk for infectious complications.
Classification of Burns
Clinical estimation of burn depth may be subjective and challenging, with one study showing only a 60%-80% concurrence between surgeons.6 Clinicians need to consider the burn wound dynamic and realize that the depth of an injury may progress or deepen in the first 24-72 hours after injury. Laser Doppler imaging may have potential as a more accurate means of estimating burn depth.6
Burns traditionally are classified as superficial (first-degree), partial thicknesssuperficial or deep dermal (second-degree), or full thickness (third-degree).
Superficial Burns. Superficial burns usually are red and glistening, with minor pain and a brisk capillary refill at the site of injury. These burns involve only the epidermis and a classic example is a minor sunburn.
Partial Thickness Burns. Partial thickness burns may be divided into superficial or deep dermal. Superficial partial thickness burns are painful, moist, red, and often have blisters and a brisk capillary refill. These burns involve the epidermis and the superficial part of the dermis and usually heal spontaneously within 1-3 weeks, without scarring. Deep partial thickness burns are paler in color, drier, have blisters, and dull or absent sensation. These burns involve the epidermis and the deep reticular dermis. Deep partial thickness burns heal spontaneously, but typically take 3-4 weeks. The degree of scarring is related to the time needed for reepithelialization.
Full Thickness Burns. Full thickness burns result when the epidermis is lost with damage to the subcutaneous tissue. Typically the burns appear dry, white or black, without blisters, and without capillary refill or sensation.
Superficial and partial thickness burns usually heal with minimal intervention whereas deep dermal partial thickness and full thickness burns likely require surgical excision and grafting to produce a functional result. (See Table 3.)

Extent of Burns
An accurate assessment of the surface area involved is an essential component of the assessment and treatment of the child with a burn injury. The simplest method is the well known "Rule of 9s." (See Figure 2.) In children, the head accounts for 18% of TBSA, the chest and back each account for 18%, each upper extremity accounts for 9%, and each lower extremity accounts for 14%. In this method the values assigned to certain body regions change with age, representing the disproportionate growth of the head and extremities and reaching adult values at 15 years of age. A quick way to estimate smaller burns is to assign a value of 1% TBSA to the area represented by the patient's hand and fingers.

Management of the Burn Patient
The initial management of burn injury can be divided into two phases: Prehospital care and ED management.
Prehospital Care. Prehospital care can have a substantial effect on outcome, both in beneficial and detrimental ways, depending on the interventions performed.
First and foremost is the safety of the provider. Once the situation is deemed safe, the victim must be removed from the source of the burn. Next any clothing, jewelry, and other such items should be removed unless they are stuck to the patient. The assessment should focus on the airway, breathing, and circulation. Spinal immobilization should be utilized in any patient with a traumatic burn or an uncertain mechanism of injury.
The decision to intubate in the field depends on local EMS protocols and the status of the airway. The presence of inhalation injury or other injury to the airway should make securing the airway a priority since subsequent swelling could make intubation difficult.7 The American Burn Association has defined specific criteria for the placement of IV access.8 These include:
- Burns with a TBSA of > 20% and an EMS transport time > 1 hour
- Hypovolemic shock from associated injuries
- Management of life-threatening ventricular dysrhythmias, potential life threatening airway obstruction, or cardiac arrest8
The next step is to cool the burn and transport the patient to the nearest hospital for advanced care. Cooling the burn may be accomplished with either cold tap water for up to 20 minutes or clean, moist dressings, but under no circumstances should ice or ice water be employed. This can cause ischemia to the area, global hypothermia, and worsen the injury.9 Hypothermia should be avoided, especially in children. Patients with chemical burns may need longer periods of irrigation.
Initial ED Evaluation and Management
The initial evaluation and management of the burn patient frequently establishes the path for hospitalization and ultimate outcome. Decisions made during the first few hours after injury can have long-term effects on both the functional and cosmetic outcomes.
The goals in the initial management of the burn patient are:
- A thorough evaluation, as with any trauma patient;
- Evaluation and management of any traumatic associated injuries that might produce life-threatening hemorrhage, such as fractures, intra-abdominal hemorrhage, and chest trauma;
- Appropriate evaluation of the status of the burn wound;
- Determination of the appropriate management course for the patient;
- Differentiation of whether hospital or ambulatory care is most appropriate; and
- Initiation of appropriate hospital care, if needed, or arrangement for follow-up care.10
Intubation. Early identification of patients who will require intubation is critical. In addition to the normal indications for intubation of a trauma patient, signs of inhalation injury, including stridor, hoarseness, drooling, dysphagia, soot around the mouth, facial burns, and burned nares should prompt consideration for intubation to prevent compromise of the airway. Recently, Pediatric Advanced Life Support guidelines have modified recommendations to include the utilizations of cuffed endotracheal tubes in children. Low-pressure cuffed endotracheal tubes should be placed in critically burned children expected to require prolonged mechanical ventilatory support, regardless of the child's age. In patients with large surface area burns (> 20% of TBSA), the release of systemic pro-inflammatory mediators may be expected to result in the development of acute respiratory distress syndrome and early intubation with a cuffed tube should be strongly considered.11
Fluid Resuscitation. Burn injury may lead to a combination of hypovolemic and distributive shock. Circulation should be assessed and IV access should be obtained quickly. Large bore peripheral IVs are most suitable for high-volume resuscitation. In young children in whom IV access is difficult, intraosseous access can be obtained, often in the anteromedial aspect of the tibia. Fluid resuscitation should be instituted with lactated ringers according to one of the fluid formulas designed for children. The various fluid resuscitation formulas are based on percentage of TBSA (See Figure 2) and weight and are targeted to address dynamic and ongoing fluid shifts.

The Parkland formula is the most commonly used fluid resuscitation protocol4 mL/kg per percent of TBSA burn with one-half of the calculated crystalloid fluid administered in the first 8 hours and the second half in the next 16 hours. (See Table 4.) In general for children with less than 10% TBSA, oral fluids or maintenance intravenous fluids usually is adequate. Children with 10%-15% TBSA generally respond to 1.5 maintenance. Children with burns greater than 15% TBSA and who weigh less than 20 kg should receive a modified Parkland formula that includes additional maintenance fluid containing glucose. Close monitoring of the blood glucose levels should be performed. Children younger than 2 years of age may become hypoglycemic because of decreased glycogen stores and have a higher rate of fluid loss because of their thinner skin and greater body surface area (BSA)/weight ratio.12 For children, an alternative formula to calculate fluid needs is the Galveston formula, which is based on BSA rather than body weight. Although some pediatric burn centers believe it is more accurate than the Parkland formula, it is more challenging and time-consuming to calculate.
- Lactated Ringer (LR) solution is used at 5,000 cm3/m2 X % BSA burn plus 2,000 cm3/m2/24 h of maintenance. One half of the total fluid is given in the first 8 hours, with the balance given over the next 16 hours. The maintenance fluid should be Ringers lactate with 5% dextrose.
- In children, maintain urine output at 1 cm3/kg/h, a pulse of 80-180 per min (age dependent) and a base deficit of < 2.
Do not routinely use blood products during a resuscitation due to the increased risk of sepsis13 and the lack of proven benefit.14 In addition, 5% albumin as a resuscitation fluid is not recommended because it has had poorer outcomes in studies.15 A recent Cochrane meta-analysis of 67 randomized controlled trials of trauma, burn, and post-surgery patients did not find any evidence that colloid resuscitation reduced mortality more effectively than crystalloids.16 The main endpoint in resuscitation is adequate urine output, which in children should be at least 1 to 1.5 mL/kg/hr. A Foley catheter must be placed to guide the resuscitation.
History and Physical Exam. A complete history of the circumstances surrounding the injury must be obtained. Pay close attention to specifics such as the etiology of the burn (flame, scald, electrical, chemical, time of exposure, whether the injury occurred in a closed space, and the possibility of additional trauma), and ascertain if the history matches the injury and developmental age of the child. These important facts help guide the care of the victim. The mechanism of injury also can guide subsequent radiological evaluation. Falls, loss of consciousness, blast injury (fireworks or home), or other mechanisms suggestive of other injuries should include appropriate diagnostic testing.
A thorough physical examination must be performed. As always, vital signs should be assessed including continuous pulse oximetry. Specific injuries to look for include head injuries, upper airway obstruction, cardiac arrhythmias, eye and ear injuries, and circumferential burns (which can lead to extremity compartment syndrome). A TBSA should be calculated. Each burned area should be assessed by location and pattern. Circumferential burns should be noted and a careful assessment of the neurovascular status performed. There is a big difference between a scald burn that wraps around a forearm and is soft with good pulses and a lower leg burn with thick white burn tissue and no Doppler pulse. The latter injury likely will require an emergent escharotomy. Discussion with burn center personnel and transfer to a burn center is appropriate for burn injuries that require further evaluation and treatment.
Escharotomy. The eschar is tough and rigid. As edema forms in an injured extremity following the burn, the eschar restricts the expansion of the tissue and results in an increase in interstitial pressure that compromises vascular flow. Incising the eschar allows return of flow and stops further ischemic injury; full-thickness burns are insensate so anesthetics are not needed. Perform escharotomy along the lateral aspect of an extremity with a linear and lengthwise incision; the incision must go completely through the eschar. Use of an electrocautery simplifies the procedure and can reduce the amount of bleeding.
If the chest is involved and the eschar compromises ventilation, an escharotomy involving the anterior chest may be performed. Incisions are made along the costal margin, along the anterior axillary lines, and across the top of the chest, freeing up the anterior chest wall. Fluid resuscitation may cause this injury to worsen quickly. Frequent Doppler and compartment pressure measurements are necessary.
Other Considerations. Laboratory studies, including a complete blood count (an elevated hemoglobin typically indicates hypovolemia), electrolytes with BUN and creatinine, a urinalysis to assess for myoglobinuria, and a blood gas for those burned in fires to assess for carbon monoxide poisoning, should be considered. Creatinine kinase and lactate dehydrogenase levels should be considered in patients with larger burns to assess response to fluid resuscitation.
Other considerations include checking the tetanus status of all patients and administering tetanus immunization as appropriate. Placement of a nasogastric or orogastric tube should be completed in children with major burns. Intravenous antibiotics should not be administered in the initial treatment of most burn patients, as this may increase the chance of colonization with more virulent and resistant organisms; they should be reserved for children with secondary infections.
Wound Dressing
Fortunately most burns seen in the ED are minor. ED physicians should cool the burn area with towels moistened with cool sterile saline; avoid immersion in ice baths. Approaches to the topical coverage of burn wounds have undergone significant change with the replacement of topical antimicrobials for intermediate-depth partial thickness burn injuries by early application of biosynthetic dressings or cytoprotective factors. Dressing application and selection depends on burn depth extent and host factors for healing. Enzymatic debriding agents, oat-derived agents, hydrogels, and biochemical skin substitutes frequently are used on noninfected wounds. Increasingly early excision for deep or extensive thermal injuries has decreased morbidity and favorably affected survival. If the patient has a burn that requires transfer to a burn center, treatment should be limited to removing the source of the thermal burn, debriding contaminated tissue, and covering the burned area with a nonadhesive cover (petroleum-based gauze) then a sterile, dry towel or sheet.
Electrical Injury
Electrical injury can occur through a variety of mechanisms, including lightning strikes, household outlets, and in children, injuries secondary to chewing on a live electrical cord. Electrical injury can be categorized as low-voltage, high-voltage, and very high-voltage (lightning).17

Low-Voltage Burns. Low-voltage burns rarely cause significant tissue damage. (See Table 5.) The exception occurs when a child bites or chews on an electrical cord. (See Figure 3.) Typically the child is younger than 6 years of age and bites or sucks on a household electrical cord. A local arc of current crosses from one side of the mouth to the other and may involve the orbicularis oris muscle. Cosmetic deformity of the lips may occur if the burn crosses the commissure. Initially, significant edema may be noted and within 2-3 days eschar formation. These patients should be referred for early follow-up to a burn specialist, plastic surgeon, or oral surgeon. Life-threatening bleeding can occur at 2-3 weeks post injury if the labial artery is exposed when the eschar falls off. Initial presentations may underestimate the extent of the ultimate injury; patients require aggressive airway management. Parents should be made aware of this possibility and advised on management strategies.

Otherwise, children who sustain low-voltage electrical injuries, with no loss of consciousness, should receive initial lab evaluations that include CK levels, an ECG, and ECG monitoring for 4-6 hours. In the pediatric population, healthy children with household current exposures (120V to 140V, no water contact) can be safely discharged if they are asymptomatic, do not have a ventricular fibrillation or cardiac arrest in the field, and have no other injuries requiring admission.18,19 Conversely, if there is significant soft tissue damage or an arrhythmia, they should be admitted for telemetry monitoring for at least 24 hours.20
High-Voltage Burns. High-voltage injuries can cause massive amounts of tissue damage as well as other injuries, including fractures either from a fall or from contraction of major muscle groups. These patients should be properly resuscitated and evaluated by a burn surgeon. Creatine kinase and CK-MB often is used in electrical injury to evaluate for cardiac injury, but there is a lack of evidence supporting its use as a diagnostic tool of cardiac injury in electrical burn, especially in the absence of ECG changes.20
Very High-Voltage Burns. Lightning injury is a dramatic occurrence that many people believe is uniformly fatal; however, because the electrical energy from a lightning strike often flows over the surface of the body rather than through it, the survival rate is 65% or higher. Cardiac standstill and paralysis of the respiratory center are the most common reasons for sudden death. A seemingly lifeless victim still should be treated because of a rare phenomenon known as keraunoparalysis, which is a transient paralysis with extreme vasoconstriction and sensory disturbances of one or more extremities. Lichtenberg's flowers are sometimes seen. Perform CPR and attempt to resuscitate the victim. Complications associated with lightning injury include cardiac and neurologic complications, ruptured tympanic membranes, and vertigo.
Inhalation Injury
Although children are less likely than adults to experience significant smoke inhalation, it remains a serious and life-threatening problem. In the pediatric population, children with coexistent burn and inhalation injuries require a cohesive team of pediatric intensive care physicians, nurses, and burn specialists to optimize outcome. Inhalation injury can present as an isolated injury or in combination with surface area burns. Initially the heat generated during combustion can cause significant thermal injury to the upper airway, requiring aggressive early airway intervention.
Direct laryngoscopy and fiber-optic endoscopy are useful to evaluate the extent of airway edema and burns, although occasionally vasoconstriction from hypovolemia may result in underappreciation of the severity of injury. If upper airway injury is suspected, elective intubation should be considered because progression of edema over the next 24-48 hours may make later intubation difficult if not impossible. In addition, this allows for direct delivery of 100% oxygen as well as bronchoscopy and inhalation therapies.
Particulate matter may mechanically clog and irritate the airways, causing reflex bronchoconstriction. In addition, asphyxiant gases including carbon monoxide (CO) and hydrogen cyanide that are released during thermal decomposition may produce injury. Other byproducts produced by combustion of furniture and cotton (aldehydes) or rubber and plastics (chlorine gas, ammonia, hydrocarbons, various acids, and ketones) produce injury. Exposure to metal fumes and fluorocarbons, systemic toxins typically released during industrial fires, is rare in the pediatric population. Children are less likely to be affected by systemic toxins than by toxins from household products and products of smoke, including CO and cyanide poisoning.21 These adverse effects on pulmonary function may last for many months after injury.
Carbon Monoxide Poisoning. CO poisoning causes toxicity by binding the hemoglobin molecule in place of oxygen. Since CO binds with much greater affinity than oxygen, oxygen unloading is impaired at the cellular level and oxygenation is impaired. The symptoms of CO poisoning start when the CO level exceeds 15%. The initial symptoms are neurologic followed by myocardial dysfunction. CO poisoning should be considered when a metabolic acidosis persists despite adequate resuscitation.
The most effective method of establishing the diagnosis of CO poisoning is by elevated carboxyhemoglobin levels measured by co-oximetry.22 Initial treatment is 100% oxygen with intubation as indicated. Although hyperbaric oxygen displaces the carbon monoxide more quickly than oxygen alone, the logistics of taking a severely burned patient to the hyperbaric chamber may prevent this.
Cyanide Poisoning. Cyanide, the other chemical of common significance, is produced from the burning of synthetic chemicals such as polyurethane. Hydrocyanide binds to the cytochrome system and inhibits cell metabolism and ATP production. Cyanide toxicity is very similar to carbon monoxide toxicity and many times they present together.
The diagnosis of cyanide poisoning is from direct measurement of cyanide blood levels, which are not always available, but empiric treatment in children is not currently recommended.23
Many times, cardiopulmonary support is the only thing needed while the liver enzyme rhodenase detoxifies the blood. The Cyanide Antidote Kit contains amyl nitrite pearls, sodium nitrite, and sodium thiosulfate.24 Sodium nitrite leads to methemoglobinemia but appropriate dosing has not been established in children. This may lead to excessive methemoglobinemia and hypotension. Treatment with hydroxocobalamin may be more advantageous in children with smoke inhalation as it does not induce methemoglobinemia and has a rapid onset of action.
Treating Inhalation Injuries. Treatment for inhalation injury in children is aggressive pulmonary toilet, which includes chest physiotherapy, therapeutic bronchoscopy, coughing, and early ambulation when possible.
Several pharmacologic modalities, such as nebulized nitric oxide, albuterol, inhaled epinephrine, and aerosolized antithrombin combined with heparin, are available for inhalation injury. (See Table 6.)

Inhalation injury should be suspected in individuals exposed to open fires or those with characteristic physical examination findings, such as soot in the nares, stridor, or cough. Early intubation, fluid resuscitation, treatment of chemical poisoning, and use of inhaled therapies are the mainstay of treatment.
Pain Management
Pain management is essential in the treatment of burn injuries. There are many different modalities that can be used to control the pain from burns and the practitioner should be familiar with the armamentarium.
Pain from burns can be characterized as acute pain from the injury itself, chronic (or background) pain from wound healing, and acute on chronic pain secondary to physical therapy, dressing changes, and other procedures needed to care for the wound.
The first step in controlling the pain from a burn is to cool the burn. This should be done with cold, tap water or clean towels dampened with cold water. Ice and ice water should not be used to prevent vasoconstriction. Once cooling is properly accomplished, pharmacotherapy can be initiated.
For minor burns, over-the-counter medication often is sufficient. Acetaminophen and nonsteroidal anti-inflammatory drugs are adequate choices. More severe injuries require stronger medications and may require a combination of opioids and sedatives.
The institution of a practice guideline for pain management assists with the timely administration of effective therapies. First, pain management must begin upon initiation of medical care, starting with intravenous opioids. Second, other medications such as benzodiazepines can be used to supplement the effectiveness of opioids. Finally, there should be a standard method to quantify pain and anxiety on a regular basis.
Opioids are the mainstay in the treatment of burn-related pain. Benefits include the care provider's familiarity with their action and dose requirements, ability to increase the dose to reach effectiveness, the variety of routes of administration (IV, oral, and mucosal), and the variety of different drugs with different profiles of onset and potency (i.e., morphine vs. fentanyl). Unwanted side effects include nausea and vomiting, vasodilation that can lead to increased fluid requirements, and eventual constipation with chronic use.
Repeat dosing may be necessary. Pediatric burns often require more frequent and larger doses than typically recommended. It is not uncommon to repeat full doses until adequate pain control is achieved.
Child Abuse
Any time a child presents with burn injuries, ED physicians must consider the possibility of abuse. Non-accidental burns are a significant source of intentional injuries in children. There are unique characteristics of a burn and the circumstances surrounding the injury that should alert the ED physician to the possibility of intentionally inflicted injuries.
The following items should alert a physician to the possibility of abuse: history that is not compatible with the child's developmental age; an inconsistent, changing story; a delay between the time of injury and the presentation for care; and shifting blame, including placing blame on the victim's siblings.
Wound features that are consistent with abuse include, but are not limited to, burns localized to the buttocks and perineum, a glove and stocking type distribution, well-demarcated burns (see Figure 4), absence of splash marks, contact burns with distinct outlines (see Figure 5), and cigarette burns. Additionally, a child who passively tolerates painful procedures should raise concerns.


Prior injuries and prior burns also may be suggestive of non-accidental injury. A full skeletal survey for occult injury should be considered, especially in younger nonverbal children, given the high percentage of occult injuries in patients with intentional burns.
ED physicians should notify local law enforcement as well as child protective services when suspicion or concern for abuse exists. Most pediatric burn patients will be transferred to a burn center, so it is better to have made initial contact with all investigative services prior to transfer.
Disposition
The American Burn Association has defined criteria for burns that warrant admission or referral to a burn center. (See Table 7.) Most pediatric patients will be admitted or called in to a burn center referral system.

Summary
Burn injuries frequently are seen in the ED and caring for pediatric burn patients can be complex. ED physicians need knowledge of the pathophysiology, hypermetabolic response, and appropriate intervention strategies. Knowledge of proper fluid resuscitation, how to approach the patient with multiple injuries, pain management, and early recognition of child abuse all are critical to treating children with burn injuries.
References
1. National Burn Repository. Report of Data from 2000-2009. Available at: www.ameriburn.org/2010NBRAnnualReport.pdf. Accessed Nov. 15, 2010.
2. American Burn Association. Resources. Available at: www.ameriburn.org/resources_factsheet.php. Accessed Nov. 15, 2010.
3. Centers for Disease Control and Prevention. Protect the ones you love: Child injuries are preventable. Available at: www.cdc.gov/Safechild/Burns/. Accessed Nov. 15, 2010.
4. Keck M, et al. Pathophysiology of burns. Wien Med Wochenschr 2009;159:327-336.
5. Jeschke MG, et al. Pathophysiologic response to severe burn injury. Ann Surg 2008;248:387-401.
6. La hei ER, et al. Laser Doppler imaging of paediatric burns: Burn wound outcome can be predicted independent of clinical examination. Burns 2006;32:550-553.
7. Branfoot T. Consensus on the pre-hospital approach to burns patient management. Injury 2006;37:668-669.
8. American Burn Association. Stabilization and transport from the pre-hospital scene. ABLS pre hospital manual. Chicago, IL: American Burn Association; 2001:44-45.
9. Allison K, Porter K. Consensus on the pre-hospital approach to burns patient management. Injury 2004;35:734-738.
10. Miller S. Optimizing outcome in the adult and pediatric burn patient. Trauma Reports 2009:10:17-24.
11. Grosfeld JL, ed. Pathophysiology. In: Pediatric Surgery. Philadelphia: Mosby. 2006.
12. Pizano LR, et al. Critical care and monitoring of the pediatric burn patient. J Craniofac Surg 2008;19:929-932.
13. Jeschke MG, et al. Blood transfusions are associated with increased risk for development of sepsis in severely burned pediatric patients. J Trauma 2007;62:676Y681.
14. Palmieri TL, et al. Effects of a restrictive blood transfusion policy on outcomes in children with burn injury. J Burn Care Res 2007;28:65Y70.
15. Cooper AB, et al. Five percent albumin for adult burn shock resuscitation: Lack of effect on daily multiple organ dysfunction score. Transfusion 2006;46:80-89.
16. Perel P, Roberts I. Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst Rev 2007;(4):CD000567.
17. ACS Surgery. Trauma. http://www.acssurgery.com/acssurgery/institutional/tableOfContent.action. Accessed Nov. 15, 2010.
18. Claudet I, et al. Risk of arrhythmia and domestic low-voltage electrical injury. Arch Pediatr 2010;17:343-349.
19. Chen EH, Sareen A. Do children require ECG evaluation and inpatient telemetry after household electrical exposures? Ann Emerg Med 2007;49:64-67.
20. Arnoldo B, et al. Practice guidelines for the management of electrical injuries. J Burn Care Res 2006;27:439-447.
21. Fidkowski CW, et al. Inhalation burn injury in children. Pediatric Anesthesia 2009;19(Suppl 1):147-154.
22. Kao LW, Nanagas KA. Carbon monoxide poisoning. Med Clin North Am 2005;89:1161-1194.
23. Demling RH. Smoke inhalation lung injury. An update. Eplasty 2008;8:e27.
24. Leybell I, et al. Toxicity, cyanide: Treatment and medication. Available at: http://emedicine.medscape.com/article/814287-treatment. Accessed Nov. 15, 2010.
Burn injuries account for half a million visits to the emergency department each year and present numerous challenges in management. The spectrum of burn injuries is immense, ranging from simple first-degree burns with no sequela to third-degree burns with hypermetabolic response. In addition, pediatric patients add unique challenges to providing optimal care.Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
