Dental Emergencies
Dental Emergencies
Overview
The emergency physician is frequently faced with patients presenting with dental complaints, particularly pain and injury. The emergency physician often reluctantly assumes the role of the after-hours dentist. This paper will outline the main dental emergencies for the emergency physician, highlighting important management issues, exploring important differential diagnoses, and reviewing practical approaches and interventions.
Some important systemic disease processes may have complaints or findings related to the oral cavity. Symptoms such as jaw claudication in temporal arteritis or gingival bleeding as an initial presentation of acute leukemia can be overlooked. Failure to include systemic diseases in the differential diagnosis will result in a lost opportunity for early detection and intervention.
Dentition and Dental Terminology
The normal adult dentition consists of 32 permanent teeth: 8 incisors, 4 canines, 8 premolars, and 12 molars. When describing and documenting dental cases in the ED, it is advisable to use the standard numbering system, although an accurate description of the tooth is acceptable, e.g., maxillary right lateral incisor for tooth # 7. The emergency physician should be familiar with the numbering system, particularly when discussing cases with a consulting oral surgeon or dentist. (See Figure 1.)

Anatomy of a Tooth
The crown is the visible portion of the tooth and consists of enamel overlying dentin. Dentin is produced by pulpal odontoblast and cushions the tooth from the repetitive stress of mastication. The dentin surrounds the pulp, which is the critical neurovascular supply of the tooth. The root of the tooth extends into the alveolar bone and is covered by cementum. Together, the cementum, alveolar bone, and periodontal ligament maintain the attachment of the dento-alveolar unit. The attached gingiva adheres to the alveolar bone, providing additional stability, and the free gingiva forms the gumline along the teeth. (See Figure 2.)

Odontalgia
Pain is perhaps the most common reason for patient to seek ED evaluation for dental complaints.1,2 This is particularly true in practice settings where there is limited access to routine dental care. It is not surprising that the majority of patients present at night, when access to a general dentist is limited. Dental pain typically results from inflammation, infection, or trauma affecting the teeth or gums. Although the majority of cases do not involve life-threatening issues, some dental problems, particularly those involving infection, have the potential to cause significant morbidity and indeed mortality. It is important to remember that non-life-threatening dental problems can have long-term functional and cosmetic sequelae if not recognized and managed early in their course. The physician should recognize when the problem is beyond the scope of practice and know when to seek general dental or oral surgery expert consultation.
Local Causes of Dental Pain
Periodontal Disease. Periodontal disease represents a continuum of disease, and patients may present to the ED at any point in the spectrum of illness.3
Gingivitis. Gingivitis refers to non-specific inflammation of the gums. Patients may present to the ED with pain, bleeding, or localized swelling of the gingiva. It can result from a build-up of dental bacterial plaque, local trauma, systemic disease, or a variety of medications. In the majority of cases, saline rinses and topical or systemic analgesia are sufficient. When significant inflammation presents or local trauma is a factor, an oral antibiotic also may be necessary. Penicillin or clindamycin generally provides good oral coverage. Patients should be referred for general dental follow-up and educated about the importance of regular preventive dental care to avoid future problems.
Leukemia, ITP, SLE, HIV, or Crohn's disease can present with oral manifestations. A thorough review of the history and systematic physical exam help identify these cases, and further testing and care will be dictated by the findings. Easy bruising, splenomegaly, or generalized adenopathy, for example, may be useful clues to an underlying and more serious disease.
A variety of medications are known to affect gingival health. Phenytoin is the best known of these. Oral manifestations of an allergic or immune-mediated medication reaction present acutely. The involvement of the oral mucosa may herald Stevens-Johnson syndrome but is not the sole manifestation of the reaction.
Pericoronitis. Pericoronitis is an inflammation of the gingival tissue overlying an erupting tooth. This tissue is referred to as the operculum, and food and debris can easily become impacted, resulting in both inflammation and infection. The third molars lie close to the masticator space, and infection potentially can extend directly from the teeth to the nearby parapharyngeal spaces. ED management of pericoronitis consists of local irrigation and removal of the debris trapped under the operculum, followed by saline mouth rinses, analgesia, NSAIDs, and oral antibiotics. Penicillin or clindamycin provides adequate coverage for dental flora. A soft diet, good oral hygiene, and referral for definitive care with a general dentist or oral surgeon are appropriate.
Acute Necrotizing Ulcerative Gingivitis (ANUG). ANUG is an invasive infection of the gingiva. It results from an overgrowth of normal oral flora. It is more common in patients who are immune-suppressed. Fusobacteria and spirochetes predominate and invade non-necrotic tissue. The condition is painful, and patients often have systemic manifestations of fevers, malaise, and regional adenopathy.4
Clinically, ANUG is characterized by tender edematous interdental papillae, and the gingival margins are ulcerated and show a gray pseudomembrane.5 The pseudomembrane covers the gingival tissue and, when removed, characteristically leaves a bleeding tissue surface. Patients typically complain of pain and often report a metallic taste. Fetor also is a common finding. In its classic form, ANUG is confined to the gingiva and tends to affect the anterior incisors and posterior molars more frequently. However any part of the gingiva can be involved. If ANUG extends to involve the buccal mucosa or tongue, it is referred to as the Cancorum Oris and can even invade and erode through teeth.
Antibiotics and improved local hygiene produce dramatic results usually within 24 hours. In the ED, warm saline or dilute 3% hydrogen peroxide rinses, typically at a 1:1 ratio, can help. Topical anesthetics can produce short-term relief, but oral analgesia and antibiotics will be necessary. Penicillin, erythromycin, or tetracycline provides adequate coverage.
The majority of patients can be managed as outpatients with dental follow-up in 2-3 days. In patients who are dehydrated and unable to tolerate fluids, admission should be considered. Patients who are debilitated or systemically ill may need admission.
Dental Caries. Patients with extensive dental caries may present with pain, hypersensitivity, or a broken tooth.2 The emergency physician should evaluate for an associated abscess, which may complicate caries. When no abscess is present, symptomatic pain relief, patient education, and referral to a general dentist is indicated.
Periodontal Abscess. Untreated dental caries can progress to invade the tooth enamel. Once the enamel is violated, the underlying dentin and pulp are exposed to saliva and bacteria from which they are normally protected. This results in local inflammation followed by infection. Pus may then track from the apex of the root to the underlying alveolar bone, and a periapical abscess forms. The initial inflammatory response produces pain and, when a secondary infection is present, the examining physician will find tenderness on percussion of the tooth. If left untreated, the abscess may next spread subperiosteally, and the spreading abscess may be seen and felt along the gingival margin. If allowed to progress, the infection has the potential to spread along the fascial planes in the head and neck or face. Although rare, these infections carry with them the potential for complications, including sepsis, airway compromise, and cavernous sinus thrombosis.
A periapical abscess with local subperiosteal spread will be visible as a swelling of the gingiva adjacent to the involved tooth and will be tender and fluctuant on palpation. Incision and drainage can be performed in the ED. Two percent lidocaine with 1:100,000 epinephrine is ideal for local infiltration of the involved gingiva. A simple stab incision using a #11 blade through the most fluctuant portion allows for easy drainage. The abscess cavity should be irrigated. Packing is generally not necessary. Although antibiotics commonly are prescribed, their role following drainage of a localized abscess remains controversial. Penicillin or clindamycin are the most common choices. Adequate analgesia should be provided and dental follow-up arranged.
Ludwig's Angina. The anatomy of the floor of the mouth and the neck is complex and allows for infections in the region to potentially track and spread easily. Ludwig's angina is a progressive cellulitis of the floor of the mouth, typically from an infected or recently extracted lower second or third molar. A history of poor dental hygiene is common, although most patients are otherwise healthy. Infections typically are polymicrobial, and the most common organisms are oral anaerobes and Streptococcus species. The existing infection becomes a rapidly progressive cellulitis involving the sublingual and bilateral submandibular spaces. Symptoms include dysphagia, odynophagia, and swelling of the sublingual region. Fever, dysarthria, voice changes, and drooling also may be noted. Ludwig's angina is a clinical diagnosis.
The first priority in management is airway control. The rapidly expanding sublingual and submandibular edema associated with the disorder has the potential to compromise the airway. The elevated and posteriorly displaced tongue and neck edema make emergency airway management extremely challenging, and an emergency cricothyrotomy or tracheostomy may be necessary.6 Fiberoptic and surgical airway equipment may be necessary. Early notification of the operating room, anesthesia, and involvement of an ear, nose, and throat (ENT) or general surgeon is indicated. Blood cultures may be helpful. IV hydration and antibiotics should be started early. Appropriate antibiotic choices include high-dose penicillin plus metronidazole, expanded-spectrum penicillin such as ampicillin-sulbactam, or ticarcillin/clavulanate. Use of IV steroids remains controversial. Surgical intervention is indicated when medical treatment fails or an abscess develops. Patients should be admitted, often to an intensive care unit. With early and aggressive management, the mortality rate is now < 10%.
Painful Oral Ulcers. Painful oral ulcers are a common occurrence, and the resulting pain, appearance, or decreased oral intake may lead to an ED visit.
Herpes Virus. Both herpes simplex and herpes zoster may cause painful vesicular lesions. Fever and lymphadenopathy are common with primary herpetic gingivostomatitis. Secondary herpes simplex tends to affect the lips primarily, but palatal and gingival lesions may occur. The lesions typically are grouped vesicles that rupture after 1-2 days, leaving painful shallow ulcers, which then heal in 6-10 days. Crusting is typical in the healing phase, and secondary bacterial infection, e.g., impetigo, may occur. Symptomatic treatment with topical analgesia and attention to local hygiene generally is sufficient treatment. The patient should be instructed to maintain adequate oral hydration. This is especially true in the pediatric population, where primary herpes simplex frequently is associated with dehydration. Anti-viral therapy with oral acyclovir, valacyclovir, or famciclovir is used in adults to lessen the severity and duration of the lesions.
Herpes zoster occurs in the distribution of the trigeminal nerve in 15-20% of cases. Pain typically precedes the eruption and may present to the ED as severe toothache or facial pain prior to the appearance of the rash. The lesions of zoster are painful, unilateral, and vesicular. Isolated intraoral lesions have been reported, but oral lesions, when present, typically occur in association with cutaneous lesions. The provider should consider zoster when a dermatomal distribution of pain exists and alert the patient to seek additional medical care or return to the ED if a rash subsequently develops.
Aphthous Stomatitis. Aphthous ulcers affect approximately 20% of the population. The etiology is unclear but appears to involve cell-mediated immune factors. Patients typically experience painful ulcers of the labial and buccal mucosa. The ulcers begin as flat erythematous lesions and subsequently ulcerate, forming a characteristic central fibropurulent base. Aphthous stomatitis occurs in two forms: a minor form and a major form. In the minor form, the ulcers are typically 3-4 mm in size and untreated heal spontaneously in 7-10 days. Treatment rarely involves more than supportive care, including chlorhexidine mouth rinses. In aph-thous stomatitis major, the ulcers are deeper and larger and can reach up to several centimeters in size. The ulcers are slow to heal and may take up to 6 weeks to resolve. Treatment of the major form consists of analgesia, hydration, and steroids. Topical corticosteroids, e.g., fluocinonide 0.05% gel or dexamethasone elixir (0.5 mg in 5 mL) swished in the mouth, are helpful. More resistant lesions may require oral steroid therapy.
Herpangina. Outbreaks typically occur in the summer and autumn and begin with systemic symptoms of sudden high fever, malaise, sore throat, and often headache. Coxsackievirus group A is the causative agent in most cases. The initial prodrome is followed by the eruption of multiple small oral vesicles that rupture, leaving painful shallow ulcers. The oral lesions of herpangina typically involve the soft palate, uvula and posterior pharynx, sparing the buccal mucosa and gingiva. This feature is useful clinically to differentiate it from primary herpes simplex gingivostomatitis, as the two otherwise appear similar. Treatment for this condition is largely supportive with adequate pain management and emphasis on adequate oral intake. Topical mixed preparations of sucralfate, Maalox, and diphenhydramine ("magic mouthwash") may be helpful to relieve the discomfort. Coxsackie-virus causes hand, foot, and mouth disease, which primarily affects pediatric patients. The oral lesions are only one of several findings in this febrile illness. The oral lesions consist of scattered, shallow, painful vesicles on the tongue, gingiva, buccal mucosa, and soft palate. They ulcerate and typically have a surrounding red halo appearance when healing. Lesions also are found on the buttocks, palms, and soles. The illness is self-limiting and lasts 6-8 days. Treatment is supportive.

Oral Candidiasis. Many normal hosts harbor candida as part of their normal oral flora. Factors that lead to overgrowth of candida include antibiotic use, local trauma (e.g., dentures), extremes of age, diabetes, and any factors producing immune compromise, such as HIV and cancer. The provider should evaluate for an underlying cause when no known risk factors exist. Referral to a primary care provider for further evaluation is appropriate. The classic finding in oral candidiasis is a thick, white, curd-like pseudomembrane that can be wiped off easily to reveal an underlying erythematous base. Treatment with topical oral antifungal agents such as nystatin oral suspension 500,000 units qid is often adequate. More extensive involvement of the mucosa or extension to the esophagus will need systemic treatment with oral fluconazole 100-200 mg per day. Leukoplakia is a white patch or plaque that cannot be scraped off. The buccal mucosa is the most common site of occurrence. The emergency physician should be careful to refer all chronic and non-healing oral lesions for specialist follow-up, as biopsy to exclude cancer is essential.
Post-extraction Pain
Dental extraction is a painful procedure, and pain is an expected sequela for the first 24 hours due to local periostitis. Oral analgesia and a soft diet are all that is generally required. Acute alveolar osteitis presents 3-5 days after extraction. Typically the patient reports that the initial post-extraction pain subsided followed by sudden and severe pain at the extraction site. Patients commonly report a foul odor and metallic taste in the mouth. Acute alveolar osteitis is also called dry socket. It results from the premature loss of the healing clot from the socket and the resultant localized infection of the underlying alveolar bone.
ED management consists of providing adequate analgesia via systemic analgesia or a dental block. Topical analgesia and aspirin-containing products should be avoided. The emergency physician should gently irrigate the socket and pack the alveolar defect with iodoform gauze soaked with local anesthetic or eugenol. Commercially available dental paste, e.g., dry socket paste, is a useful alternative. Packing produces considerable pain relief. The patient should be discharged with adequate analgesia and NSAIDs. The use of oral antibiotics is common, although their use is not universally recommended. The packing is a temporary solution only, and the patient should be referred for dental follow-up.7
Referred Pain
Not all mouth pain is dental in origin. The complex innervation of the head and neck make referred pain an important consideration. The emergency physician should perform a systematic head and neck examination when a patient presents with dental pain and no local cause is identified.
Temporomandibular Joint (TMJ) Dysfunction and Dislocation. Chronic TMJ dysfunction may present with symptoms varying from clicking to locking or pain. While the majority of patients with chronic TMJ can be referred for definitive care, the provider should evaluate the patient for a more serious or urgent cause, e.g., occult trauma from domestic violence or child abuse.8 The examining physician also should consider systemic disorders, which may manifest as TMJ problems, e.g., the classic jaw claudication of temporal arteritis. Patients may present with TMJ dislocation or subluxation. Many cases do not involve significant trauma; a simple yawn may be the only activity involved.
TMJ Pain. The TMJ is a hinge joint but involves the more complex movements of mastication. The articular surfaces are separated by a meniscus or disk to allow for the smooth movement required by the joint. Opening of the jaw involves the actions of the lateral pterygoid, digastric, mylohyoid, and geniohyoid muscles. Closing of the jaw is accomplished by the combined actions of the masseter, medial pterygoid, and temporalis muscles. Chronic TMJ dysfunction may result from degenerative joint disease or from anatomical deviations from prior trauma or congenital factors. Systemic disease processes, e.g., rheumatoid arthritis, also may affect both the TMJ structure and function. History should focus on baseline function, including locking, clicking, or pain.
Examine the jaw for asymmetry. Observe the patient opening and closing the jaw and observe for clicking or locking of the joint. The mandibular condyle can be palpated by placing a finger anterior to the tragus and asking the patient to open and close the joint. A click may be audible or palpable. Observe for malocclusion of the teeth. Palpate the muscles of mastication, as they are often the area where pain is felt or referred when TMJ dysfunction exists.
In the majority of cases, there is no indication for diagnostic imaging in the ED. Exceptions are traumatic injuries. This is particularly important in cases of domestic violence or child or elder abuse.9 Mandibular X-rays or CT scans should adequately show trauma.
Chronic pain and dysfunction of the jaw are best evaluated and imaged in a non-acute care setting and should be referred to an oral maxillofacial surgeon. The emergency physician should provide appropriate pain management, and patient reassurance and education may be helpful.
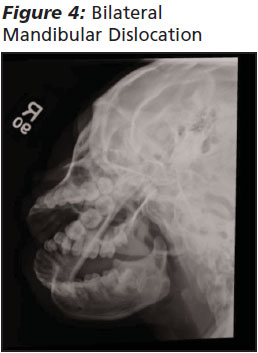
TMJ Dislocation. (See Figure 3 and 4.) When a patient presents to the ED with acute pain and malocclusion, TMJ dislocation must be considered. Many cases of anterior dislocation do not involve significant trauma, especially when chronic joint laxity exists. On presentation, patients are uncomfortable, have difficulty speaking and swallowing, and are unable to open and close their jaws normally. They have limited range of movement and malocclusion. Examination will confirm masseter spasm, and this contributes to maintaining the mandible in the dislocated position. The majority of TMJ dislocations are bilateral and anterior. In cases of TMJ dislocation where no significant acute trauma has occurred, other predisposing factors are likely to exist. These include an anatomical shallow articular fossa, connective tissue disorders, or remote trauma. They also predispose the patient to recurrent dislocation in the future. Posterior, lateral and superior, and unilateral dislocations generally occur as a result of significant trauma. The presence of a fracture in addition to a dislocation implies significant force was involved, and a thorough search for other injuries, e.g., c-spine or intracranial injury, should be undertaken. The presence of a fracture dislocation necessitates the early consultation of an oral maxillofacial surgeon, as reduction will be more complex and there is a high likelihood that internal fixation will be required.
Reduction of a closed anterior TMJ dislocation without an associated fracture is within the scope of the emergency practice.4 If trauma is involved, an X-ray should be obtained prior to reduction to exclude an associated fracture and to confirm the diagnosis. If the dislocation was spontaneous, imaging is generally not indicated and can be considered on a case-by-case basis. Entities such as TMJ hem-arthrosis and acute closed locking of the TMJ meniscus can mimic a dislocation, and their management will obviously differ.
Appropriate analgesia, either oral or IV, is essential during TMJ reductions. Procedural sedation is rarely necessary and poses its own inherent risks. Using a sterile technique, approximately 2-3 mL of 2% lidocaine can be injected into the joint space, which can be felt as a depression just anterior to the tragus.

The patient should be seated facing the examiner, with his or her head resting against a firm surface (e.g., wall or chair back). The examiner should stand and place both gloved thumbs along the occlusive surfaces of the mandibular molars. The patient should try to open the jaw as far as possible and relax the jaw muscles as much as possible. The examiner should place slow, steady pressure downward and backward to dislodge the mandible. (See Figure 5.) Successful reduction will be apparent by a sensation of a "pop," relief of pain, and return of function and mobility of the jaw. Post-reduction films are generally not necessary unless ongoing discomfort exists post-procedure. Procedural complications are rare, although iatrogenic fracture has been known to occur. Failure to reduce the mandible will require oral maxillofacial surgeon consultation in the ED.
Once successfully reduced, most patients can be discharged home with oral maxillofacial surgeon follow-up, adequate analgesia, and instructions for a soft diet and to avoid opening the mouth wide. In cases of an associated fracture, oral maxillofacial surgeon consultation is necessary.
Dento-alveolar Trauma
The teeth and gums are prone to injury from falls, accidents, and assaults. The central maxillary incisors are involved in approximately 70% of dental fractures and are often due to falls.9,10 The resulting injury can have both cosmetic and functional implications.
The Ellis Classification.(See Figures 6, 7.) Ellis I refers to fractures limited to the enamel of the tooth. No specific intervention is indicated in the ED. If a portion of the fractured enamel is particularly sharp, it may irritate the tongue or mucosa, and filing the sharp edge may be helpful.


Ellis II refers to fractures that involve the dentin of the tooth in addition to the enamel. Clinically the patient will have extreme sensitivity of the injured tooth and even may experience pain with airflow across the tooth. The examining physician may be able to identify an Ellis II by direct visualization of the tooth; the exposed dentin appears as a creamy substance. Loss of dentin exposes the underlying pulp to drying, oral flora, and saliva. The longer the pulpal tissue is exposed, the greater the risk of contamination and subsequent inflammation and possible necrosis. Once an Ellis II fracture is recognized, the next priority is to reduce exposure of the pulp and reduce the risk of further contamination. This is best achieved by covering the dentin with a commercially available dental cement and providing urgent dental referral within 24 hours. Calcium hydroxylate paste is widely available and easy to use. Some are pre-mixed formulations while others require mixing of the base and catalyst immediately prior to use. The tooth surface should be clean and dry to optimize adherence with the paste. The paste sets within minutes. Dental foil may be placed over the paste, although it is not essential. Successful use of 2-octyl cyanoacrylate tissue adhesive has been reported, although in case reports only.11
Ellis III refers to fractures in which the pulp is directly exposed. The patient experiences sensitivity and pain as in an Ellis II, but on direct visualization, the examiner will note bleeding from the fracture site. When the fracture site is wiped with a sterile gauze, the blood continues to accumulate. The emergency physician should cover the exposed dentin and pulp with dental cement as for an Ellis II and provide oral analgesia and urgent dental referral within 24 hours. Oral antibiotics often are prescribed, especially if tooth exposure was prolonged, although their value has not been definitively established.12 The definitive treatment for Ellis III is endodontic or root canal therapy. Topical analgesia should be avoided.10,13
Dental root fractures are rare, accounting for fewer than 5% of all dental fractures. In some cases, if enough root remains, root canal therapy still may be possible to allow for tooth restoration. In other cases, however, extraction of the residual coronal segment will be required. Only a dentist will be able to make this determination, and the patient should be told that ED determination of the prognosis is neither possible nor appropriate in most cases.
Luxations. When patients present following trauma and no fracture is noted, further evaluation for tooth tenderness or mobility should be undertaken. Tenderness to percussion is an important finding and is indicative of injury to the supporting structures of the involved tooth. The presence of mobility indicates that additional damage to the supportive structures is present.
Concussion. Tenderness without mobility is referred to as a concussion. Treatment involves analgesia, NSAIDs, a soft diet, and referral to a general dentist for further evaluation and care.
Subluxation (Loosening). Tenderness and mobility but without dislodgement of the tooth is referred to as subluxation of the tooth. Subluxed teeth generally do not require splinting, and management involves analgesia, NSAIDs, a soft diet, and referral to a general dentist for further evaluation and care.
Luxation refers to displacement of a tooth. The term extrusive luxation describes a partial avulsion or axial displacement of a tooth from the alveolar bone. When the tooth is displaced laterally with an associated alveolar fracture, it is called a lateral luxation. When the tooth is displaced into the socket itself with an associated alveolar fracture, it is called an intrusive luxation.
Extrusive luxation of a tooth requires repositioning of the tooth into its original position. This is best achieved under local anesthesia and by the application of firm but gentle pressure. Once in place, the tooth needs to be stabilized in this position to allow for healing. Ideally, stabilization is achieved with flexible wire splinting, but in cases of extrusive luxation, temporary splinting with commercially available periodontal paste (e.g., Coe-Pak) is an acceptable alternative in the emergency setting.14 Mixing the base and catalyst forms a paste that becomes firm after application. The gingiva and enamel should be dry before applying the paste, which should be applied into the inter-dental grooves and adjacent teeth to create a fitted mold. The patient should fully understand that this is a temporary solution only and that definitive care with a dentist or oral surgeon is needed within 24 hours. Patients who have limited dental follow-up can be advised to return to the ED in 24 hours for re-evaluation. The physician should emphasize, however, that definitive care can only be provided by a dentist or oral surgeon.
Management of lateral luxation is more challenging, as there is an associated alveolar fracture and repositioning of the tooth is more difficult. It is generally advisable to consult an oral surgeon or dentist in the ED for repositioning and splinting of the tooth.
Intrusive luxation is associated with significant damage to the alveolar socket and the periodontal ligament. Left untreated, the likelihood of root absorption and subsequent tooth loss is high. The tooth may erupt on its own or may require orthodontic extrusion. An oral surgeon or dentist is the best person to decide the best treatment for the patient.

Avulsion implies that the tooth has become totally displaced from its socket. (See Figure 8.) In cases of permanent teeth, re-implantation should be undertaken as soon as possible. The success rate of re-implantation is directly related to the time the tooth has been out of the socket. It is estimated that the rate of success falls by 1% for every minute the tooth is out of the socket. Preservation of the periodontal ligament fibers is critical to successful re-implantation.15 Handle the tooth by the crown only, and avoid direct contact with the root and ligament fibers. The tooth should be rinsed gently with sterile saline to remove dirt or debris prior to re-implantation. Rinsing is adequate, and the tooth should never be wiped.16
Irrigate the socket gently with saline and remove any residual clot prior to re-implantation. The damaged socket generally is very sensitive, and local anesthesia is advised. Once both the tooth and the socket have been prepared, replace the tooth in the socket, paying attention to the proper orientation and optimization of the alignment. Apply firm pressure on the tooth, and maintain it in place by placing gauze on the occlusal surface and asking the patient to bite down. If available, a dentist or oral surgeon should be consulted for stabilization. Do not delay re-implantation of the tooth for the consultant's arrival. If no dental or oral surgeon is available, temporary stabilization using commercially available molding material is acceptable. It is important to remember that primary teeth should not be re-implanted. The tooth may fuse with the alveolar bone and prevent subsequent eruption of the underlying permanent tooth.13
Storage and Transport Media. When an avulsed tooth is recovered, place it in a transport medium as soon as possible. If an avulsed tooth has been dry for less than 20 minutes, the likelihood of maintaining viable pulp is high. The ideal transport and storage medium is Hank solution. This commercially available preparation is a pH-balanced cell culture medium and maintains periodontal ligament cell viability for 2-4 hours. Acceptable alternative transport media include milk or sterile saline.
Cautions. When the tooth is not recovered at the scene, it is important to establish that the tooth has not been impacted into the socket (intrusive luxation). Careful inspection and palpation of the socket often is adequate, but in cases of doubt, an X-ray may be necessary.
When the tooth is not retrieved and the possibility of aspiration of the tooth exists (e.g., small child or a patient with altered mental status), a chest X-ray should be obtained to evaluate further.17
Avulsion or luxation of primary teeth is treated very differently from that of permanent teeth. Avulsed primary teeth are never re-implanted, and inappropriate re-implantation may damage the underlying permanent tooth and prevent its later successful eruption. Significant luxation of primary teeth generally requires extraction of the tooth. The decision of whether to remove an intruded primary tooth should be left to a dentist, but the caregiver should be aware that it is essential to seek definitive care by a dentist or oral surgeon within 24-48 hours following the ED encounter.
Management of Dental Pain
Topical anesthetics can be used but play a limited role due to their short duration of action and limited effectiveness. They may play a role for topical anesthesia of the mucosa prior to dental blocks, particularly in the pediatric population.
Oral analgesia is a reasonable first-line approach to pain relief in many cases. NSAIDs are both effective and provide both anti-inflammatory effects and analgesia.18,19 In some cases, the addition of a narcotic agent is needed. When additional pain relief is needed or a painful procedure is necessary, the choice rests between parenteral medications (an NSAID such as ketorolac or a narcotic such as morphine) or a dental block. Dental blocks generally are very effective and well tolerated by the patient.1 Depending on the agents used, they offer the additional benefit of prolonged analgesia following discharge and provide pain relief until definitive care can be obtained.
Orofacial Innervation. The innervation of the face and oral cavity is complex, involving cranial nerves V and VII. The trigeminal nerve (V) divides into three main branches: the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3). V1 and V2 are entirely sensory nerves, while V3 contains both sensory and motor fibers. The sensory dermatomes of the trigeminal nerve have relatively sharp borders and very little overlap in contrast to the rest of the body. The facial nerve (CN VII) is the second cranial nerve involved in orofacial innervations and has three major components. In addition to motor and sensory function, this nerve also supplies some parasympathetic fibers to head and neck ganglia.
Dental Anesthesia
Supra-periosteal Infiltration. The simplest technique for intraoral local anesthesia of a tooth is supra-periosteal infiltration. It is ideally suited for anesthesia of a single tooth. It is best performed with the patient seated in a chair with the occiput firmly against a headrest. A topical anesthetic can be applied prior to the procedure to alleviate the pain of the first injection. The patient should close the jaw slightly to relax the facial musculature. The lip should be pulled gently, and the mucobuccal fold should be penetrated with the bevel facing the bone. Direct the needle toward the apex of the specific tooth in question. If the bone is contacted, withdraw the needle by approximately 2 mm to avoid inadvertent subperiosteal injection. Once in position and after aspiration, inject 1-2 mL of the anesthetic toward the apex of the involved tooth. Complete anesthesia may take 5-10 minutes.
Dental Blocks. Dental blocks are very effective in the ED for therapeutic and procedural relief of pain.20 They may even play a diagnostic role at times. Contraindications to dental blocks are mostly limited to allergy to local anesthetics; however, vascular, liver, and heart disease may all increase the risk of complications.
Pretreatment of the mucosa with a topical anesthetic may be useful. The injectable anesthetic agents most commonly used in the ED include lidocaine, bupivacaine, and mepivacaine. The choice of anesthetic agent depends primarily on the physician's experience and preference. The addition of a vasoconstrictor is common and assists in reducing bleeding and increasing the duration of action of the anesthetic.1 Two percent lidocaine with 1:100,000 or 1:50,000 epinephrine; 3% mepivacaine plain or mepivacaine 2% with 1:20,000 levonordefrin; and 0.5% bupivacaine with 1:200,000 epinephrine are most commonly used in the ED. All three are amides and have a similar side effect profile. Adverse effects include CNS excitability and cardiovascular toxicity and are related primarily to inadvertent intravascular injection. Lidocaine is an amide and has a half-life of 1.5 to 2 hours. It is metabolized by the liver and its actions may be prolonged in patients with significant hepatic impairment or congestive heart failure. Mepivacaine is a tertiary amide and commonly is used for dental blocks. Lidocaine and mepivacaine have been found to have similar efficacy and safety profiles.21 Bupivacaine has the advantage of a longer duration of action. It has been associated with more significant cardiotoxicity, however, when inadvertent systemic absorption has occurred. Most adverse events and fatalities relate to inadvertent IV injection during epidural anesthetic.22
The following points should be kept in mind when performing an intraoral injection for a dental block:
Ask about allergies prior to choosing a specific agent.
Never insert the needle all the way to its hub. Breakage of the needle is rare but can occur, making retrieval extremely difficult.
Avoid changing the direction of the needle while it is deep in the tissue, to reduce unnecessary trauma.
Always aspirate prior to injection to minimize the risk intravascular injection.
Avoid injecting directly into infected tissue.

Inferior Alveolar Block. This block provides anesthesia to all teeth on the ipsilateral side of the mandible, the lower lip, and chin via block of the mental nerve. As with the other blocks, the patient should be seated so the open mandible is parallel to the floor. The gloved thumb of the non-injecting hand is placed along the anterior border of the ramus of the mandible in the coronoid notch. The retromolar fossa should be palpated with the thumb or index finger. The landmark for the inferior alveolar nerve block injection site is the medial surface of the mandibular ramus posterior to and 1 cm above the occlusal surface of the third molar. A 25- or 27-gauge needle ideally is used and should be directed from the opposite side of the mouth, typically between the first and second premolars to the injection site. Advance the needle until the bone is contacted, withdraw slightly, aspirate, and inject 1-3 mL of anesthetic. It is important during this block to contact the bone, as failure to contact the bone could result in injection into the parotid gland, causing an inadvertent paralysis of the facial nerve. This complication is unusual and generally is self-limited. (See Figure 9.)
Infra-orbital Nerve Block. Palpate for the midpoint of the lower margin of the orbit. The inferior oribital nerve exits its foramen approximately 1 cm inferior to this point. Place a finger over the foramen site to serve as a landmark. Retract the cheek and direct the 25- or 27-gauge needle with syringe superiorly through the mucosa parallel to the long axis of the ipsilateral upper premolar. Advance the needle approximately 2 cm until it is palpated near the foramen. Follow-ing aspiration, approximately 2 mL of local anaesthetic is infiltrated. Epin-ephrine is best avoided due to the proximity of the facial artery. (See Figure 10.)

Post-extraction Bleeding
Applying local pressure with a sterile gauze is usually sufficient. Patients on anticoagulants or with underlying bleeding disorders may present an additional challenge. Post-extraction bleeding should be managed by saline or peroxide rinses or gentle irrigation of the socket followed by direct pressure with a sterile gauze. Pressure should be maintained for at least 15 minutes, and the patient can assist by directly biting down on the gauze. Soaking the gauze with a topical vasoconstrictor such as epinephrine can be helpful. Dental roll gauze is ideal as it fits more easily between teeth. If bleeding persists, use of coagulating agents such as Gelfoam or Surgicel can be helpful. Once placed in the socket, it can be loosely sutured in placed and gauze packed over it. Again, the patient should bite down for approximately 15 minutes. Electrocautery devices designed for dental use are available and may be considered if simple pressure fails. If bleeding continues despite these simple measures, the emergency physician should consider the possibility of an underlying bleeding disorder.
Intraoral Lesions
Although rarely an acute or emergency issue, patients may present to the ED for evaluation after the discovery of a lump or tumor in their mouth. The lump generally is related to the salivary glands and requires little more than reassurance and referral to an oral surgeon.
Mucoceles and mucus retention cysts arise from minor salivary glands in the oral cavity and can be found anywhere in the oral cavity. A ranula is a retention cyst of the sublingual gland and can be identified by its location under the tongue. It typically presents as a smooth, round, non-tender swelling that develops slowly and is generally long-standing when encountered by the emergency physician. No ED intervention is indicated and definitive care with excision or marsupialization can be undertaken by a dental or oral surgeon at a later date if needed.
Pyogenic granulomas result from the benign proliferation of immature capillaries at the site of local minor trauma. They typically occur on the gingiva. The resulting local overgrowth is visible as a smooth, red, non-tender swelling. Their appearance and rapid growth frequently is a cause of concern to the patient and may prompt a visit to the ED. These lesions generally regress spontaneously. ED management is limited to recognition of the condition, reassurance to the patient, and referral for follow-up. There is no indication to remove pyogenic granulomas in the ED, and due to their vascular nature, they are likely to bleed if inappropriately incised in the ED.
Salivary Gland Disorders
The parotid, submandibular, and sublingual glands comprise the three major groups of salivary glands. In addition, there are innumerable minor salivary glands throughout the mucosa of the oral cavity. Patients may present to the ED with pain or swelling related to the salivary glands.
Sialolithiasis, or salivary duct stone, occurs most commonly in men during the third to sixth decade of life. The majority affect the submandibular gland, followed by the parotid. The stones typically are calcium phosphate or calcium carbonate in nature. The most common presenting symptoms are pain, swelling, and tenderness in the involved glands, and symptoms generally are exacerbated by eating.
The diagnosis of sialolithiasis is made by history, although a stone may be palpable on examination. Calcium-based stones also may be seen on radiographs. The ED management is primarily symptomatic and includes analgesia, application of local heat, massage and sialologues. If the stone is visualized at the duct orifice, it often can be removed by gentle massage. If the stone is not visualized or cannot be removed easily, the patient should follow up with an oral surgeon or ENT specialist as soon as possible for removal. Retention of a stone predisposes the patient to secondary infection and stricture formation. If secondary bacterial infection is suspected, oral antibiotic therapy is indicated. Staphylococcus, Streptococcus viridans, S. pneumoniae, and H. influenza are the predominant organisms. Amoxicillin-clavulanate or clindamycin provides adequate coverage.
Suppurative parotitis is a potentially serious bacterial infection. It is due to retrograde movement of oral bacteria into the salivary ducts and paren-chyma. Stones may predispose patients to infection, and affected patients often are elderly or debilitated. The onset of symptoms usually is rapid, with pain, swelling, and fever. The skin over the gland is characteristically red and tender. Trismus is common. Pus may be expressed from the Stensen duct if the parotid gland is involved. Amylase typically is normal, and there typically is a neutrophilic leukocytosis. The most common pathogen involved is S. aureus. Other organisms include H. influenza, S. pneumonia, S. pyogenes, and anaerobes such as Bacteroides, peptostreptococci, and fusobacteria.
ED management includes analgesia, IV hydration, and IV antibiotics effective against both staph. and anaerobes. Ampicillin-sulbactam is a good choice. Clindamycin may be used if penicillin allergy exists. Vancomycin is appropriate if MRSA is suspected. Patients who are discharged from the ED can be given amoxicillin-clavulanate or clindamycin.
Dental Procedures in the ED
Emergency departments vary considerably in their access to dental and oral surgery services. In academic centers, the ED physician may have 24/7 access to in-house consultation services and may have little opportunity or need to perform dental procedures in the ED. In contrast, emergency physicians in rural settings may have no immediate access and may be the only providers available to deal with minor dental emergencies and procedures. Regardless of the ED setting, every practicing emergency physician should be familiar with basic ED dental procedures and equipment.4,16

Recommended supplies that should be available in the ED are listed in Table 1.
Summary
Many people do not have easy access to other health care or preventive dental care, and emergency physicians frequently may encounter these cases as a result.23 Familiarity with the most common dental emergencies and their ED management and access to the necessary equipment to manage these cases will improve the lives of the patients.
References
1. Yagiela JA. Anesthesia and pain management. Emerg Med Clin North Am 2000;18:449-470.
2. Dunn WJ. Dental emergency rates at an expeditionary medical support facility supporting Operation Enduring Freedom. Mil Med 2004;169:349-353.
3. Douglass AB, Douglass JM. Common dental emergencies. Am Fam Physician 2003;67:511-516.
4. Amsterdam JT. Emergency dental procedures. In: Roberts JR, Hedges J, eds. Clinical Procedures in Emergency Medicine, 5th ed. Philadelphia:WB Saunders; 2009.
5. Horning GM. Necrotizing gingivostomatitis: NUG to noma. Compend Contin Educ Dent 1996;17:951.
6. Shockley WW. Ludwig's angina: A review of current airway management. Arch Otolaryngol Head Neck Surg 1999;125:600.
7. Garibaldi JA. Dentoalveolar surgical sequelae. Compend Contin Educ Dent 1998;19;407.
8. Welbury R, Murphy J. The dental practitioners role in protecting children from abuse. The orofacial signs of abuse. Br Dent 1998;184:62.
9. Dale RA. Dentoalveolar trauma. Emerg Med Clin North Am 2000;18:521-538.
10. Rauschenberger CR, Hovland EJ. Clinical management of crown fractures. Dent Clin North Am 1995;39;25-51.
11. Hile LM, Linklater DR. Use of 2-octyl cyanoacrylate for the repair of a fractured molar tooth. Ann of Emerg Med 2006;47:424-426.
12. Klokkevold P. Common dental emergencies. Evaluation and management for emergency physicians. Emerg Med Clin NorthAm 1989;7:29-63.
13. Dumsha TC. Luxation injuries. Dent Clin North Am 1995;39;79-91.
14. Medford HM. Temporary stabilization of avulsed teeth. Ann Emerg Med 1982;11:490.
15. Barrett EJ, Kenny DJ. Avulsed permanent teeth: A review of the literature and treatment guidelines. Endod Dent Traumatol 1997;13:153-162.
16. Krasner P. Modern treatment of avulsed teeth by emergency physicians. Am J Emerg Med 1994;12:241-246.
17. Trope M. Clinical management of the avulsed tooth. Dent Clin North Am 1995;39:93.
18. Dionne RD, Gordon SM. Non-steroidal anti-inflammatory drugs for acute pain control. Dent Clin North Am 1994;38:645-667.
19. Cooper SD. The relative efficacy of ibuprofen in dental pain. Compend Contin Educ Dent 1986;7;584-588.
20. Jastak JT, Yaglela JA, Donaldson D. Local anesthesia of the oral cavity. Philadelphia: WB Saunders; 1995.
21. Porto GG, Vasconcelos BCE, Gomes ACA, et al. Evaluation of lidocaine and mepivacaine for inferior third molar surgery. Med Oral Parol Oral Cir Bucal 2007;12: E60-E64.
22. Rosenblatt MA, Abel, M, Fischer GW, et al. Successful use of 20% lipid emulsion ot resuscitate a patient after presumed bupivacaine related cardiac arrest. Anesthesiology 2006;105:217-218.
23. Waldrop RD, Ho B. Increasing frequency of dental patients in the urban ED. Am J Emerg Med 2000;18:687-689.
The emergency physician is frequently faced with patients presenting with dental complaints, particularly pain and injury.Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
