Managing Lower Extremity Sports Injuries
June 1, 2022
Authors
Nicole Prendergast, MD, Chief Resident, Stanford University School of Medicine, Palo Alto, CA
Mia L. Karamatsu, MD, Clinical Assistant Professor of Emergency Medicine, Stanford University School of Medicine, Palo Alto, CA
Peer Reviewer
Steven M. Winograd, MD, FACEP, Attending Emergency Physician, Keller Army Community Hospital, West Point, NY
Executive Summary
- Talar osteochondral injuries are a separation of cartilage and bone that may result from acute trauma or repetitive microtrauma. Treatment is dependent on the lesion stage, I through IV, with stage IV characterized by a displaced fragment. Nonsteroidal anti-inflammatory medications (NSAIDs) should be prescribed, and activity modification, including immobilization and application of a non-weight-bearing splint, should be recommended for four to six weeks or until follow-up with orthopedics.
- Acute ankle fractures account for 12% of fractures seen in pediatric patients. Ankle fractures are affected by the presence of growth plates at the distal tibia and fibula and can be described by the Salter-Harris classification system.
- The most common ankle fracture occurs at the distal fibula from a supination-inversion mechanism. Patients will have tenderness over the distal fibular physis. Radiographs typically demonstrate acute soft tissue swelling without evidence of fracture and can be treated with a walker boot with weight bearing as tolerated for three to four weeks.
- Fifth metatarsal (MT) fractures are the most common MT fracture in children, comprising 45% of MT fractures, with 22% involving the base of the fifth MT. Patients describe a twisting or inversion of the ankle. The exam is notable for pain and swelling to the base of the fifth MT. Diagnosis can be made with AP, lateral, and oblique radiographs, but if imaging is negative and there is high clinical suspicion, additional lateral views should be considered.
- Plantar fasciitis is an overuse injury that that is most common in overweight adults but can occur in all age groups. Athletes who engage in a high frequency of jumping, hill running, and speed work, in addition to those with pes cavus and varus hindfoot, are at higher risk. In young athletes, plantar fasciitis usually coincides with calcaneal apophysitis and rarely exists in isolation. Presentation in athletes with a fused physis is notable for morning pain and stiffness worse over the medial arch or heel that may be exacerbated by climbing stairs or weight bearing on dorsiflexed toes. The examination is notable for tenderness along the medial edge of the plantar fascia or at its origin on the anterior edge of the calcaneus. Plantar fasciitis is a clinical diagnosis. Treatment includes rest, ice, NSAIDs, orthotics, Achilles tendon stretching, and heel cups.
- Patellar dislocation occurs primarily in patients aged 15 to 19 years, with a recurrence rate of 34% to 38%. Patients typically will present following direct trauma or an aggressive cutting and pivoting motion with a lateral displacement of the patella and tearing of the medial patellofemoral ligament. Many of these injuries will reduce spontaneously. The diagnosis is confirmed with a history of lateral patellar displacement. Examination findings are notable for increased patellar mobility, and tenderness of the medial femoral condyle or lateral femoral condyle. However, 20% of cases require reduction, which can be performed with gentle medial pressure along the lateral border of the patella while passively extending the knee.
- Osteochondritis dissecans (OCD) refers to subchondral bone separation usually secondary to repetitive axial loading and microtrauma. Patients present with poorly localized knee pain that worsens with exercise, particularly on inclined surfaces, and anteromedial joint line tenderness. Radiographs are notable for a cyst-like lesion on the femoral condyle. MRI is recommended for staging.
- Hip injuries can be classified as involving the bony skeleton, avulsion and physeal fractures, dislocations or soft tissue injuries, labrum tears, apophyseal insertions, and contusions. Pain location often is helpful in determining the etiology. For example, groin pain is concerning for intra-articular pathology, whereas lateral pain is more likely associated with iliotibial band syndrome or abductor fatigue syndrome.
- Legg-Calvé-Perthes disease is caused by osteonecrosis of the proximal femoral epiphysis. It is more common in males than in females, with an average patient age of 7 years. Patients present with an insidious painless limp developing over one to three months, followed by hip and ipsilateral knee pain, effusion, and decreased range of motion. Radiographs should be obtained, and early findings include a radiolucent subchondral zone in the anterolateral epiphysis known as the crescent sign.
— Ann M. Dietrich, MD, FAAP, FACEP, Editor
Introduction
Musculoskeletal injuries are the third most common chief complaint in the emergency department (ED) and account for about 2.6 million visits made by children and young adults aged 5 to 24 years, with 42% of them occurring in the lower extremity.1 According to a national survey conducted by the U.S. Department of Health and Human Services from 2018-2019, about 56.1% of children and adolescents aged 6 to 17 years participated in organized sports in the United States.2 In one study, 5- to 14-year-olds had the highest rate of injury from sports and recreational activities.3
Furthermore, increasing rates of child and adolescent sports participation, in addition to escalating levels of intensity in youth athletic training and competition, increase the risk for both acute and overuse injuries.4 Youth athletes also present with unique injuries when compared to their adult counterparts because of their skeletal immaturity and congenital or developmental differences. Because of these differences, and the relative frequency of pediatric patients presenting to EDs or urgent care centers, injuries can be easily missed. Therefore, it is imperative for emergency physicians to understand the basic anatomy, evaluation, management, and discharge planning for young athletes.
General Approach
Common lower extremity sports injuries will be discussed by joint system — ankle and foot, knee, and hip — using a standardized approach.
History
A detailed history, including the mechanism of injury and history of preceding symptoms, is essential to the diagnosis and targeted radiographic imaging. The patient’s age also is important in the development of the initial differential, given the effect skeletal maturity has on susceptibility to certain injury patterns.
Examination
A focused exam should be performed on the area of concern in comparison to the unaffected side. In addition, examine the joints above, below, and the area in between. Providers should palpate the entire area and perform passive, active, and resisted range of motion. Joint-specific physical examination maneuvers pertinent to emergency management are listed in Table 1. A neurovascular exam also should be performed. If possible, gait should be assessed.
Table 1. Joint-Specific Physical Examination Maneuvers5-7 | ||
| Maneuver (Structure Assessed) | Description | Positive Response |
Anterior drawer test (anterior cruciate ligament) |
|
Increased tibial displacement anterior |
Posterior drawer test (posterior cruciate ligament) |
|
Increased tibial displacement posterior |
Ober’s test (iliotibial band tightness) |
|
Upper leg remains elevated |
Noble’s test (iliotibial band tightness) |
|
Pain |
Squeeze test (ankle distal syndesmosis disruption, fractures, os trigonum) |
|
Pain |
Ankle anterior drawer (anterior talofibular ligament injury) |
|
Increased forward movement of talus |
McMurray test (meniscus) |
|
Pain, click, or inability to extend knee |
Lachman test (anterior cruciate ligament) |
|
Moves anterior without a firm end point |
Posterior sag test (posterior cruciate ligament) |
|
Proximal tibia sags |
Varus stress (lateral collateral ligament) |
|
Pain or opening of lateral joint |
Valgus stress (medial collateral ligament) |
|
Pain or opening of medial joint |
Patella grind test (patellofemoral pain syndrome) |
|
Pain |
J sign (patellar maltracking) |
|
Lateral subluxation of the patella |
Wilson sign (osteochondritis dissecans) |
|
Pain |
FABER (hip or sacroiliac joint pathology, iliopsoas tightness) |
|
Pain or leg remains elevated |
Radiographs
In the setting of acute sports trauma or injury, radiographs are strongly recommended. Although many of these injuries are accompanied by normal radiographs and diagnosis is dependent on physical examination, it is important to exclude fracture prior to proceeding to magnetic resonance imaging (MRI) and computed tomography (CT). Furthermore, radiographs often can assist with follow-up of an acute injury, even when negative.8
Management
All lower extremity injuries will benefit from pain control, including nonsteroidal anti-inflammatory medications (NSAIDs) or acetaminophen. Pain control should be escalated appropriately for obvious deformities noted on the exam. Acute fractures or dislocations may require urgent reduction. However, most acute injuries, even those that ultimately are deemed operative, are managed initially with pain control as noted, with immobilization vs. application of stretching, compression, and elevation. Return to play is strongly dependent on the injury pattern. Most patients require some degree of outpatient follow-up with physical therapy (PT), sports medicine, and/or orthopedic surgery.
Foot/Ankle Injuries
The foot and ankle are the most commonly injured areas of the lower extremity in adolescent athletes and are the second most common reason for presentation to a pediatrician, accounting for 30% of sports medicine visits.9 The ankle is a hinged joint composed of the talus, medial malleolus, distal tibia plafond, and lateral malleolus with supporting ligamentous structures (including the deltoid ligament medially and the anterior and posterior talofibular ligaments and calcaneofibular ligament laterally, demonstrated in Figure 1). Accessory ossicles can be present in 20% of children around the foot and ankle and usually appear around ages 7 to 10 years.10
Figure 1. Ankle Anatomy |
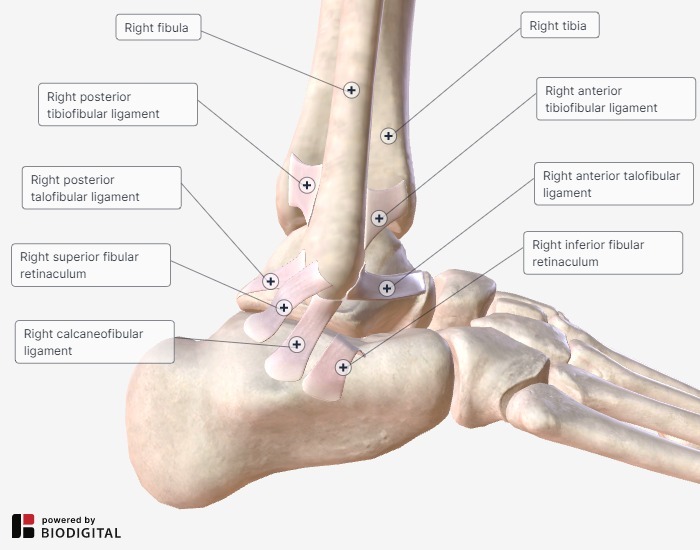 |
Talar osteochondral injuries are a separation of cartilage and bone that may result from acute trauma or repetitive microtrauma. Anterolateral lesions occur with dorsiflexion and inversion of the ankle, while posteromedial lesions occur with plantar flexion and inversion. Patients typically present with ankle pain, swelling, instability, and a clicking sensation. Diagnosis can be made with anteroposterior (AP), lateral, and mortise ankle radiographs. Treatment is dependent on the lesion stage, I through IV, with stage IV characterized by a displaced fragment. NSAIDs should be prescribed, and activity modification, including immobilization and application of a non-weight-bearing splint, should be recommended for four to six weeks or until follow-up with orthopedics. All lesions with a displaced fragment and those failing conservative management are operative.9,10
Tarsal coalition is a rare, abnormal connection between two bones of the hindfoot or midfoot that leads to limited subtalar mobility and altered biomechanics. The most common tarsal coalitions are talocalcaneal and calcaneonavicular. Symptoms often present in the second decade of life with hindfoot pain and are exacerbated by frequent athletic activities. A history of recurrent ankle sprains or distal fibular physeal fractures also may be present.9 The physical exam will be notable for limited mobility when performing range of motion. AP, lateral, and oblique ankle radiographs should be obtained and will be notable for arthritic-looking changes surrounding tarsal joints. Management largely is conservative and should include follow-up with orthopedics, orthotics, and PT. However, young athletes are at risk for persistent pain and stiffness, requiring surgical intervention with a return to play of about six to eight weeks from surgery.
Acute ankle fractures account for 12% of fractures seen in pediatric patients. Ankle fractures are affected by the presence of growth plates at the distal tibia and fibula and can be described by the Salter-Harris classification system. (See Figure 2.) The most common ankle fracture occurs at the distal fibula from a supination-inversion mechanism. Patients will have tenderness over the distal fibular physis. Radiographs usually demonstrate acute soft tissue swelling without evidence of fracture and can be treated with a walker boot with weight bearing as tolerated for three to four weeks.
Figure 2. Salter-Harris Classification Types12 |
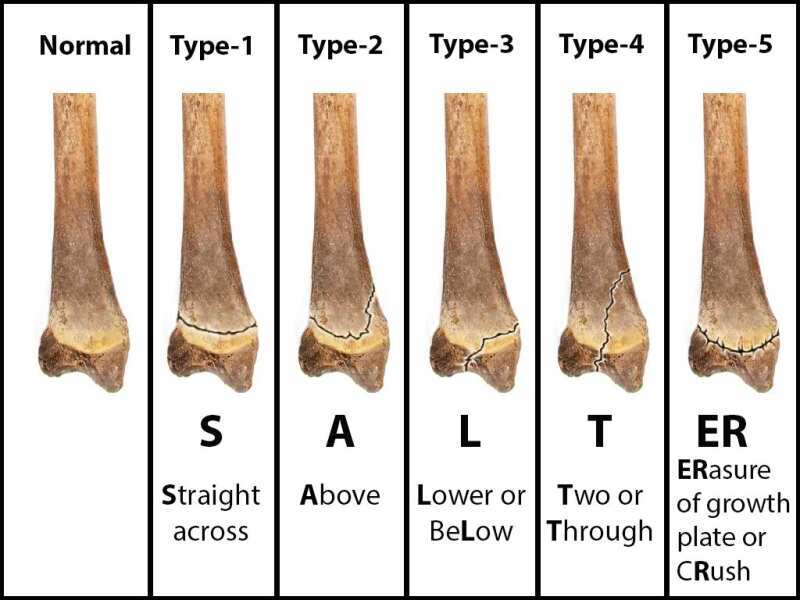 |
Levine RH, Foris LA, Nezwek TA, Waseem M. Salter Harris fractures. StatPearls [Internet]. Updated Nov. 7, 2021. https://www.ncbi.nlm.nih.gov/books/NBK430688/ |
Fractures of the tibia are less common, and the exam is notable for tenderness over both the tibial and fibular physes. Treatment is dependent on the fracture type, degree of displacement, and ability to hold reduction and alignment. In general, Salter-Harris I fractures are treated with a short-leg cast for three to four weeks. Meanwhile, Salter-Harris II fractures are treated with closed reduction and casting for four to six weeks. Salter-Harris III and IV injuries involve intra-articular extension of the fracture. If there is less than 2 mm of displacement on CT scan after reduction, the fracture can be treated with casting. Displacements of more than 2 mm after reduction require surgery.9,10 Misinterpretation of radiographs and missing a fracture can result in osteonecrosis, slowed bone growth, growth plate closure, and abnormal secondary ossification caused by traumatic disruption of the epiphyseal blood supply.11
Foot Fractures
Lisfranc injuries are fracture-dislocations of the tarsometatarsal joint complex that are rare in children and often missed.13 Common mechanisms include crush injury or forced plantar flexion and abduction on a fixed foot in sports, such as football or soccer. Patients present with pain, swelling and inability to bear weight. Plantar ecchymoses should raise suspicion for a Lisfranc injury on exam. Three-view radiographs should be obtained. Even with negative radiographs, if there is a high clinical suspicion, a CT scan should be performed for diagnosis and evaluation for intra-articular injury and comminution.
Fifth metatarsal (MT) fractures are the most common MT fracture in children, comprising 45% of MT fractures, with 22% involving the base of the fifth MT. Of these fractures, 90% of cases occur in children older than 10 years of age.14 Patients describe a twisting or inversion of the ankle. The exam is notable for pain and swelling to the base of the fifth MT. Diagnosis can be made with AP, lateral, and oblique radiographs, but if imaging is negative and there is high clinical suspicion, additional lateral views should be considered. The apophysis of the fifth MT typically is seen in children aged 7 to 16 years and are commonly misdiagnosed as fractures. Avulsion fractures at the base of the fifth MT rarely are displaced and can be treated with the application of a short-leg walking boot for six weeks. Fractures at and beyond the metaphyseal and diaphyseal junction (Jones’ fractures) can be given a trial of immobilization in a non-weight-bearing cast for six to eight weeks. However, orthopedics referral for acute fixation should be considered in athletes to facilitate more predictable healing and, ultimately, earlier return to sport.10
Plantar fasciitis is an overuse injury that that is most common in overweight adults but can occur in all age groups. Athletes who engage in a high frequency of jumping, hill running, and speed work, in addition to those with pes cavus and varus hindfoot, are at higher risk. In young athletes, plantar fasciitis usually coincides with calcaneal apophysitis and rarely exists in isolation. The calcaneus ossification center appears at 9 years of age and fuses at 16 years of age. Presentation in athletes with a fused physis is notable for morning pain and stiffness worse over the medial arch or heel that may be exacerbated by climbing stairs or weight bearing on dorsiflexed toes. The examination is notable for tenderness along the medial edge of the plantar fascia or at its origin on the anterior edge of the calcaneus. Plantar fasciitis is a clinical diagnosis. Treatment includes rest, ice, NSAIDs, orthotics, Achilles tendon stretching, and heel cups. Some patients may benefit from steroidal injections.20
Ankle sprains account for 25% to 30% of all athletic injuries and are most commonly caused by inversion and plantar flexion. However, eversion and external rotation also can occur, leading to deltoid, syndesmotic, and ankle mortise disruption.16 Peak incidence for males is ages 15 to 19 years and for females ages 10 to 14 years.17 The exam will be notable for swelling and tenderness over the anterior talofibular and calcaneofibular ligaments.9 Anterior drawer testing also should be performed. Ankle sprains can be classified into three grades of severity with examination findings and anticipated recovery times. (See Table 2.)
Table 2. Grade Classification of Ankle Sprains | |||
| Examination | Treatment | Recovery | |
Grade I |
|
|
1-2 weeks |
Grade II |
|
|
8-12 weeks |
Grade III |
|
|
> 3 months |
Recurrent ankle sprains are rare in children before growth plate closure. Therefore, any patient describing frequent sprains should be evaluated for tarsal coalition. Therapy should focus on rest, ice, elevation, and early mobilization, with aggressive physical therapy aimed at strengthening. Radiographs should be considered in patients with deformity or high-risk injury pattern. Radiographs also can be considered if the injury and exam do not satisfy the low-risk ankle rules (LRAR)19 or Ottawa ankle rules (OAR).20
A retrospective study comparing the two rules in children ages 12 months to 18 years found the OAR had a sensitivity of 100% and a specificity of 33.1%. Use of the OAR would have reduced the number of ankle radiographs ordered by 32.1%. The LRAR had a sensitivity of 85.7% and a specificity of 64.9% and would have reduced the number of ankle radiographs ordered by 63.1%. However, the LRAR missed four high-risk fractures.18 It has been noted despite this retrospective comparison that these rules have had varied success in the pediatric population and should be applied with caution.17
Peroneal tendon subluxation is a serious injury in young athletes resulting from forced ankle dorsiflexion, eversion, and acute rupture of the superior peroneal retinaculum and eventual tendon dislocation. Patients usually have a history of recurrent sprains and may describe a snapping over the lateral aspect of the ankle. Tendon subluxation can be reproduced on exam with dorsiflexion and eversion. Because spontaneous reduction is common, ultrasound can be used to dynamically evaluate a subluxation event. Radiographs should be obtained to rule out fracture. Patients in whom suspicion is high for this injury should be referred to orthopedics. Treatment involves placement in a short-leg cast with the ankle in mild plantar flexion and inversion for six weeks. NSAIDs also may be recommended.9
Shin splints, or tightness in the anterior tibia, are the cause of 60% of all exercise-related leg pain. Shin splints are caused by medial tibial stress or chronic exertional compartment syndrome and can result in tibial stress fractures. They generally are the result of an escalation of intensity or duration of exercise in a short period of time. The exam is notable for tenderness over the anterior tibia that worsens with ankle movement. In patients with normal radiographs, management involves rest, NSAIDs, and stretching, with gradual return to play.
Knee Injuries
It is estimated that 2.5 million sports-related knee injuries occur in adolescents each year.7 Furthermore, 54% of young athletes have knee pain annually, and 60% of sports-related surgeries in high school athletes involve the knee.21 Given the increased specialization and increasing intensity of training and competition, youth athletes are subjected to both chronic, repetitive overuse and acute knee injuries. Children undergo significant growth at the knee and, therefore, have injury patterns that differ from those seen in adults. Examinations should include passive, active, and resisted range of motion and palpation of the following landmarks: tibial tuberosity; patella, medial, and lateral joint line; fibular head; distal femur; proximal tibia; patellar facet; and Gerdy’s tubercle. Although often limited by pain, valgus and varus stress tests, anterior and posterior drawer tests, or Lachman and McMurray tests also can be performed to assess for ligamentous injury. A knee effusion in an acute injury represents a hemarthrosis and, in 70% of adolescent athletes, represents severe injuries that include fracture, ligament tear, or joint dislocation, which will be discussed in further detail later. Therefore, plain radiographs and advanced imaging may be indicated.21
Patellar dislocation occurs primarily in patients aged 15 to 19 years, with a recurrence rate of 34% to 38%.22 Patients typically will present following direct trauma or an aggressive cutting and pivoting motion with a lateral displacement of the patella and tearing of the medial patellofemoral ligament. Many of these injuries will reduce spontaneously. The diagnosis is confirmed with a history of lateral patellar displacement. Examination findings are notable for increased patellar mobility, and tenderness of the medial femoral condyle or lateral femoral condyle. However, 20% of cases require reduction, which can be performed with gentle medial pressure along the lateral border of the patella while passively extending the knee. Findings also may be notable for secondary effusion.23 Patellar dislocations also are the most common cause of osteochondral knee fractures in pediatric patients with incomplete ossification of the patella and can occur following reduction. Therefore, AP, lateral, sunrise, and bent knee PA radiographs also should be performed pre- and post-reduction. A supportive brace with a lateral buttress should be applied, immediate weight-bearing with crutches should be encouraged, and patients should be prescribed a short course of NSAIDs with PT referral to focus on quadriceps strengthening. A referral to orthopedics should be placed for follow-up in one to two weeks. Athletes usually can return to play in three weeks.22 Operative management typically is for those with a superimposed fracture, chronic instability, or recurrent dislocations.7
Patellofemoral pain syndrome (PFPS) affects 7% to 20% of adolescent athletes and is the leading cause of chronic anterior knee pain in patients nearing or at skeletal maturity. It often is seen during growth spurts and is more common in female athletes. Patients typically present without an acute injury. They experience pain both during and after exercise, and after long periods of sitting. It generally is worse when ascending and descending stairs, running, jumping, and squatting. The examination may be notable for tenderness along the medial patellofemoral ligament or peripatellar area, quadriceps atrophy, positive patellar grind test, and positive J sign. Treatment involves PT, in particular strengthening of the quadriceps tendon, NSAIDs, and activity modification.22,24
Apophysitis of the knee occurs at the tibial tubercle (Osgood-Schlatter disease [OSD]) or at the distal pole of the patella (Sliding-Larsen-Johansson disease [SLJ]).24 OSD typically presents during periods of rapid growth, ages 10 to 15 years for males and ages 8 to 13 years for females. It commonly affects those who participate in sports that involve running and jumping. Patients present with gradual onset of pain at the tibial tuberosity, which is exacerbated with activity and improves with rest. In 20% to 30% of cases, it occurs bilaterally. The exam is notable for point tenderness and swelling at the tibial tubercle, and pain is reproducible with resisted extension or passive flexion of the knee. OSD generally is diagnosed clinically, but radiographs may show fragmentation of the apophysis or calcification of the distal patellar tendon. (See Figure 3.) Treatment involves activity modification, including cross-training, relative rest, ice following activity, NSAIDs, and PT. Immobilization should be considered only in severe cases. Operative intervention is rare, and most cases resolve in one to two years as the physis closes.7,12 SLJ disease shares clinical features with OSD and sometimes can occur in conjunction with OSD. The inferior pole of the patella is cartilaginous in adolescents, making it susceptible to inflammation, fragmentation, and infrapatellar bursitis. Radiographs show spurring at the inferior pole of the patella, and ultrasound is notable for swelling and thickening of the patellar tendon. The treatment and prognosis are similar to those for OSD.7
Figure 3. Knee X-Ray |
 |
Note the cortical irregularity and subtle transverse lucency at the tibial tuberosity with knee effusion consistent with a diagnosis of apophysitis. Image courtesy of Nicole Prendergast, MD |
Iliotibial band (IT) syndrome involves inflammation of the thick band of fascia that extends distally from the lateral iliac crest over the lateral femoral condyle to the proximal tibia at Gerdy’s tubercle.22 It is most common in activities requiring repetitive extension and flexion of the knee, such as running and cycling. A sudden increase in training or training on uneven ground without concomitant strengthening of hip abductors causes hip adduction — compression of nerve-rich tissue at the distal IT band that leads to pain. Patients generally describe lateral knee pain without instability. The examination generally is notable for tenderness along the lateral aspect of the knee (2 cm above the joint line) and positive Ober and Noble’s tests. Treatment includes rest, ice, activity modification, hip strengthening, massage, foam rolling, and a short course of NSAIDs.24
Ligamentous Tears
Anterior cruciate ligament (ACL) tears are one of the most common ligamentous injuries of the knee in young athletes. The risk of ACL injury starts at ages 12 to 13 years for girls and ages 14 to 15 years in boys.25 ACL tears commonly are associated with soccer, basketball, football, gymnastics, and lacrosse. Noncontact injuries are very common, especially in female athletes. ACL tears are two to eight times more likely in adolescent females, possibly because of anatomical, biomechanical, and hormonal reasons.26 The mechanism of injury often involves a change in direction with a simultaneous landing movement, hyperextension with a sudden deceleration, or rotational force on a fixed foot. Traumatic contact ACL injuries typically are associated with concomitant injuries to the meniscus or medial or lateral collateral ligaments, or posterolateral corner fracture. Athletes typically describe a popping sensation and generally present with a large effusion. In a relaxed patient, the Lachman test will be positive, with a sensitivity of 85% and a specificity of 94%. Providers should place an outpatient referral for MRI and orthopedic surgery for possible surgical reconstruction.21,25
Posterior cruciate ligament (PCL) tears in isolation are rare, occurring in only 3.5% to 7.5% of knee injuries.21 They occur when an athlete falls on a flexed knee with the foot in plantar flexion or with a direct blow to the anterior knee. The exam is notable for a positive posterior drawer test, sensitivity of 90% and specificity 99%, and positive sag sign.27 Isolated PCL injuries can be treated with immobilization in extension for two weeks followed by PT emphasizing quadriceps strengthening. Stress radiographs may show a sag of the tibia when taken in the sagittal plane. If there is a suspicion for complete PCL tear or concomitant ACL, medial collateral ligament (MCL), lateral collateral ligament (LCL), or meniscal injury, treatment generally is surgical; therefore, referral should be made to orthopedics.21,27
The MCL is the most commonly injured collateral ligament, and adolescent athletes are more susceptible to physeal injury. Injury usually occurs with valgus or external rotation over a slightly flexed knee and planted foot. Given the MCL is extra-articular, no effusion is present on exam. A valgus stress test will result in pain and/or laxity. Treatment is conservative and involves early weight bearing and mobility as tolerated. A hinged knee brace can be useful, and athletes can return to sports activity if laxity is not evident on examination.21 LCL injuries can occur in all ages and genders and are most common in tennis, gymnastics, and wrestling. The common mechanism is a direct blow to the anteromedial aspect of the knee and, less commonly, hyperextension plus varus stress. Patients present with medial knee pain, a feeling of instability, and a positive varus stress test. Partial tears can be managed nonoperatively. Given LCL injuries rarely occur in isolation (only 2%) providers should have a high suspicion for additional ligamentous injury or dislocation. Complete tears and injuries associated with dislocation or other ligament injuries require orthopedics referral and surgical repair.22
Radiographs should be obtained to rule out an avulsion, fracture, dislocation, osteochondral injury, and degenerative findings. Plain films sometimes can identify insidious causes of bone pain, such as a tumor. MRI is the gold standard for diagnosis of ligamentous injury, which typically is performed as an outpatient.
Meniscus injuries generally occur in sports with frequent, high-energy changes in direction and twisting, typically in athletes older than 12 years of age.28 The meniscus is located between the femoral condyles and tibial plateaus, and it protects the articular cartilage by stabilizing the knee and distributing forces across the knee joint. The medial meniscus has a stronger attachment to the joint capsule, which makes it more susceptible to injury.22 Patients often report swelling, instability, a feeling of catching or locking, and the inability to fully extend their knee. The exam is notable for an effusion, joint line tenderness, and a positive McMurray maneuver, which has a 62% sensitivity and 81% specificity for medial meniscal tears and 50% sensitivity and 89% specificity for lateral tears, respectively.28 Radiography should be performed to rule out fracture. MRI should be recommended if there is a concerning history or exam. Although MRI remains the gold standard for diagnosis, its sensitivity and specificity are significantly lower for children younger than 12 years of age. Small, nondisplaced peripheral tears may heal spontaneously, but larger tears have improved healing in children with surgical repair. Therefore, all cases require follow-up with orthopedics.21
A discoid meniscus is a congenital variant affecting 3% to 5% of the population with an abnormal composition of collagen fibers and abnormal vascularity.7,29 It generally occurs on the lateral side, associated with hypermobility and meniscal tears, with 15% to 25% of patients having bilateral involvement.28 Patients generally are younger than 10 years old and present with snapping, clicking, and knee pain, with an inability to fully extend the knee. Examination is notable for a lateral bulge. As with meniscal injuries, an MRI is required for diagnosis. Those with symptoms generally require an orthopedic referral for operative management.21,28,29
Osteochondritis dissecans (OCD) refers to subchondral bone separation, usually secondary to repetitive axial loading and microtrauma. Damage occurs at the immature articular cartilage because of disruption of local blood supply. OCD is four times more likely in boys and is bilateral in 25% of cases.7,30 It most commonly occurs at the lateral aspect of the medial femoral condyle. A positive Wilson’s test may help with the diagnosis of a medial femoral condyle lesion.31 Patients present with poorly localized knee pain that worsens with exercise, particularly on inclined surfaces, and anteromedial joint line tenderness. Radiographs are notable for a cyst-like lesion on the femoral condyle. MRI is recommended for staging and management. Conservative management generally is successful and involves activity and weight-bearing restriction, PT, and gradual return to activity over four to six weeks. Operative management involves fixation, excision, or grafting, with return to play in three to six months. Radiograph and MRI imaging are recommended before returning to play.7
Tendinitis of the quadriceps, patella, hamstring, and, less often, the popliteus tendon occurs in skeletally mature adolescent athletes engaging in repetitive running and jumping, such as a soccer player or cross-country runner. Patients often note pain at the site of the tendon that is worse with activity. Ultrasound can show fluid around the tendon and is helpful to confirm the diagnosis. Treatment involves NSAIDs, activity modification, and PT with eccentric strengthening exercises and stretching.24
Knee Fractures
Tibial spine avulsion fractures are uncommon and seen in youth ages 8 to 14 years. They account for up to 5% of all pediatric knee injuries with effusion.32 Examinations are notable for effusion and limited range of motion. Radiographs can identify the fracture. Treatment involves immobilization of the leg with a posterior long-leg splint and providing crutches. Orthopedic referral must be placed.
Tibial tubercle avulsion fracture has a high incidence in patients aged 9 to 12 years. It occurs when the athlete contracts their quadriceps when jumping and then lands onto a fixed foot. Patients will present with pain with extension and tibial tubercle tenderness and swelling. A neurovascular exam also should be done to rule out compartment syndrome. Radiography of the knee can diagnose the fracture, but it should be followed by MRI to rule out intra-articular involvement. Nondisplaced fractures without involvement of the physis can be managed with a cast for four weeks, while others require orthopedics referral for operative management with screw fixation.33
Patellar sleeve fractures are characterized by an avulsion of cartilage with an associated subchondral osseous fragment from the distal or proximal pole of the patella by the patellar tendon. This injury is caused by rapid contraction of the quadriceps muscle with a flexed knee. It is most prevalent in children nearing skeletal maturity, with a peak incidence of 12.7 years, and are three times more common in boys.34 Those participating in high intensity training who have had rapid growth are at high risk. Patients report anterior knee pain with associated trauma. The exam is notable for patellar tenderness, effusion, and a palpable gap at the border of the patella. Radiography can miss the injury if there is no associated radiopaque osseous fragment; therefore, if suspicion is high, the patient will need an MRI. Nondisplaced fractures are treated with a long-leg cast, while displaced fractures require open reduction and fixation, therefore all require orthopedic follow-up.21,34
Distal femoral fractures comprise 1% of pediatric fractures; however, there is a high risk of growth arrest. The distal femur is responsible for 35% to 40% of the growth of the lower limb.35 These injuries generally occur with a direct blow to the knee, leading to hyperextension, and valgus or varus stress, and they occur most commonly in football. Patients present with tenderness over the distal femur, swelling, and inability to bear weight. Radiography can be negative in 56% of cases, therefore if there is a high clinical concern, an MRI should be obtained and an orthopedic referral placed. Nondisplaced fractures generally are treated with a long-leg cast for four to six weeks, while displaced fractures are treated operatively.
Proximal tibial fractures comprise 3% of physeal fractures in the lower extremity.36 Fracture generally occurs with a hyperextension force resulting in apex posterior angulation at the metaphysis. The exam is notable for a tense effusion. It is vital to check for pulses and sensation distal to the injury, given the potential injury to popliteal vasculature. Radiographs can show a subtle, minimally displaced fracture with widening of the physis, and MRI should be used if radiography is normal. Nondisplaced fractures can be managed with long-leg casts for four to six weeks, while displaced fractures require closed reduction or surgical fixation.21
Hip Injuries
Hip injuries occur in approximately 53 out of 100,000 adolescent- and college-age athletes and include acute trauma, overuse, and abnormal development.37 Adolescent athletes are at particular risk for apophyseal and epiphyseal injuries because their cartilaginous growth plates have not ossified, whereas older athletes generally present with tendinitis in these areas. Hip injuries are most common in sports with explosive movements, including soccer and football, as well as running sports and dancing.37,38 Hip injuries can be classified as involving the bony skeleton, avulsion and physeal fractures, dislocations or soft tissue injuries, labrum tears, apophyseal insertions, and contusions. Pain location often is helpful in determining the etiology. For example, groin pain is concerning for intra-articular pathology, whereas lateral pain is more likely associated with iliotibial band syndrome or abductor fatigue syndrome. Physical examination should include range of motion, strength testing, and gait analysis. Radiographs should start with AP, false profile, and frog leg views.
Hip dislocations are rare in the pediatric population, with less than 5% occurring in patients younger than 14 years of age, but they are a true emergency. They are most common in boys and often result from sports injuries or low-height falls in.37 The majority (90% to 95%) of dislocations are posterior, and patients present with a flexed, adducted, and internally rotated lower extremity. A neurovascular exam should be performed, given the risk for sciatic nerve injury. Radiographs can confirm the diagnosis, and CT can be useful to evaluate post-reduction for evidence of fracture fragments or acetabular fracture. Emergent reduction should be performed within six hours, given the risk of osteonecrosis, and can be done in the ED using analgesia and sedation. Failure after three reduction attempts or the presence of superimposed fracture fragments between the femoral head and acetabulum warrants surgical management. Given the risk of osteonecrosis approaching 15%, even with successful reduction, any reduction performed six or more hours after injury should include discharge instructions for MRI three to six months post-injury.38
Apophyseal avulsions result from repetitive stress during rapid acceleration and deceleration that result in muscle contraction or passive muscle lengthening across an apophysis in high-impact sports such as soccer, football, gymnastics, and track. Apophyseal avulsions are most common in 14- to 17-year-old athletes because of intrinsic weakness of the epiphyseal plates in skeletally immature adolescents.37,39 Patients will present with sudden onset pain and functional weakness and may experience or hear a “pop.” Exam is notable for swelling, ecchymosis, and pain with passive and active range of motion. The anterior inferior iliac spine (AIIS) apophysis is the most frequently affected location with eccentric contraction of the rectus femoris. (See Table 3.) Avulsions with less than 2 cm of displacement are commonly treated conservatively with rest, ice, and NSAIDs, with weight-bearing as tolerated with crutches until symptom resolution, followed by PT. Avulsions with greater than 2 cm of displacement have a high risk of symptomatic non-union, decreased mobility and chronic pain, and, therefore, require surgery.37 (See image online at https://bit.ly/3KJalus.)
Table 3. Common Adolescent Avulsion Fractures and Associated Muscle43 | |
| Apophysis | Common Muscle Avulsion |
Anterior inferior iliac spine |
Rectus femoris |
Ischial tuberosity |
Hamstrings |
Anterior superior iliac spine |
Sartorious |
Iliac crest |
Abdominal muscles |
Lesser trochanter |
Iliopsoas |
Pubic symphysis |
Rectus abdominis |
Femoral neck fractures generally occur because of repetitive microtrauma and encompass 5% to 7% of stress fractures. Female long-distance runners are at higher risk, as are patients using steroids, who smoke, or who have metabolic syndromes.37 Patients typically present with insidious, progressive hip pain that localizes to the groin and worsens with high-impact activities. Pain initially may occur with exercise, but eventually occurs at rest. The examination is notable for pain with internal rotation of the hip and hopping on the affected extremity.37,39 Radiographs should be obtained, but they often are negative early in the disease process. A high index of suspicion should warrant a rapid-sequence MRI, which will show evidence of bony edema on T2-weighted images. Fractures to the medial (compression) side are most common and can be managed conservatively with toe-touch weight bearing, NSAIDs, and PT. Those on the lateral (tension) side require surgical fixation. Femoral neck stress fractures can progress to unstable fractures and are at risk for avascular necrosis of the femoral head, so accurate, timely diagnosis is vital. The patient’s history should evaluate for features of the female athlete triad, which includes amenorrhea and nutritional deficiencies secondary to disordered eating.
Pyriformis syndrome presents with a dull posterior hip or buttock pain that radiates down the leg and may be mistaken for radicular pain. Pyriformis syndrome is common in runners and is worse with prolonged sitting. The exam is notable for pain on active external rotation, passive internal rotation of the hip, and tenderness to palpation at the sciatic notch. Treatment involves stretching, NSAIDs, activity modification, and PT.41
Bursitis is inflammation of the small fluid-filled sacs that prevent friction of soft tissue over bony prominences during motion. The trochanteric bursa is located lateral to the greater trochanter and is the most common site for bursitis, often resulting from falls and overuse injuries in runners and dancers. Patients present with pain over the greater trochanter and pain on transitions from sitting to standing. The exam is notable for pain on palpation of the greater trochanter. Radiographs should be considered to exclude an occult fracture. Treatment involves ice, NSAIDs, iliotibial band stretching, protection from direct trauma, and consideration of steroid injections. The bursa overlying the ischial tuberosity is most commonly injured after a fall onto the buttock. The iliopsoas bursa cushions the hip flexor as it traverses the femoral head and inserts on the greater trochanter. Patients with iliopsoas bursitis present with pain and snapping over the medial thigh and groin area. The examination is notable for pain with active and passive extension and flexion of the hip. Treatment includes iliopsoas stretching and steroid injections.41
Acetabular labral tears occur with abrupt twisting or planting and cutting motions during sport activities. Patients will present with hip or groin pain and often note a catching sensation when ranging the affected hip. On exam, pain may be reproduced with internal and external rotation. Pain with flexion, adduction, and internal rotation is highly sensitive for intra-articular pathology and also will be painful in these patients. Radiographs are necessary to rule out underlying hip deformity, and, if they are negative, follow-up may include recommendations for MR arthrography.38
Legg-Calvé-Perthes disease is caused by osteonecrosis of the proximal femoral epiphysis. It is more common in males than in females, with an average patient age of 7 years.42 Patients present with an insidious painless limp developing over one to three months, followed by hip and ipsilateral knee pain, effusion, and decreased range of motion.41 Radiographs should be obtained, and early findings include a radiolucent subchondral zone in the anterolateral epiphysis known as the crescent sign. MRI can be performed to further characterize the amount of femoral head involvement, but it is unnecessary in the acute setting.37 Positive prognostic factors include age younger than 9 years and less than 50% femoral head involvement.39 Treatment involves maintaining the femoral head within the acetabulum, which involves bracing, traction, and possible surgical intervention.
Slipped capital femoral epiphysis (SCFE) is caused by weakness of the proximal femoral physis, resulting in anterior displacement of the metaphysis relative to the epiphysis, which remains in the acetabulum. It has the highest prevalence in overweight Black males aged 10 to 16 years and often correlates with the pubertal growth spurt. It typically is unilateral; however, up to 60% of patients can have bilateral involvement, especially those with underlying endocrine disorders.38 Adolescents present with hip, thigh, or knee pain that worsens with activity. The average duration of symptoms prior to presentation is around five months. The examination is notable for external rotation and hip flexion. Radiographs of the AP pelvis and frog leg lateral hip confirm the diagnosis and show a Klein line that does not intersect the epiphysis. In the setting of negative radiographs with high clinical suspicion, an MRI can show edema around the physis. Treatment is surgical management and requires prompt orthopedic surgery consultation from the ED, given the risk of developing early onset osteoarthritis.38
Conclusion
This article is inclusive of a large quantity of injuries, but a large subset described can be managed conservatively with rest, ice, NSAIDs, and will resolve with PT. Kinesiotaping also can be recommended in these cases. Radiographs frequently are helpful to exclude injuries requiring urgent orthopedic surgery consultation and guide appropriate follow-up for patients. Do not forget to consider physeal and overuse injuries and potential congenital deformities in the pediatric athlete population.
REFERENCES
- Patel DR, Yamasaki A, Brown K. Epidemiology of sports-related musculoskeletal injuries in young athletes in United States. Transl Pediatr 2017;6:160-166.
- Data Resource Center for Child & Adolescent Health. National and State-Specific Findings from the National Survey of Children's Health. Baltimore; 2007.
- Sheu Y, Chen L-H, Hedegaard H. Sports- and recreation-related injury episodes in the United States, 2011-2014. Natl Health Stat Report 2016;(99):1-12.
- Jayanthi N, Kleithermes S, Dugas L, et al. Risk of injuries associated with sport specialization and intense training patterns in young athletes: A longitudinal clinical case-control study. Orthop J Sports Med 2020;8:2325967120922764.
- Gruber L, Lee V, Singh R, Ganta D. Specialized musculoskeletal examination. PM&R Knowledge Now. Updated Sept. 23, 2021. https://now.aapmr.org/specialized-musculoskeletal-examination/
- Slaughter AJ, Reynolds KA, Jambhekar K, et al. Clinical orthopedic examination findings in the lower extremity: Correlation with imaging studies and diagnostic efficacy. Radiographics 2014;34:e41-55.
- Kuwabara A, Kraus E, Fredericson M. Narrative review — knee pain in the pediatric athlete. Curr Rev Musculoskelet Med 2021;14:239-245.
- Hwang C, Sims L, Wang NE. Common overuse injuries of the pediatric lower extremity. Pediatric Emerg Med Rep 2013;18:25-35.
- Erickson JB, Samora WP, Klingele KE. Ankle injuries in the pediatric athlete. Sports Med Arthrosc Rev 2016;24:170-177.
- Gill LE, Klingele KE. Management of foot and ankle injuries in pediatric and adolescent athletes: A narrative review. Orthop Res Rev 2018;10:19-30.
- Woods R, Boutis K. Just the facts: Diagnosing growth plate fractures in the emergency department. CJEM 2020;22:291-294.
- Levine RH, Foris LA, Nezwek TA, Waseem M. Salter Harris fractures. StatPearls [Internet]. Updated Nov. 7, 2021. https://www.ncbi.nlm.nih.gov/books/NBK430688/
- Kushare I, Wunderlich N, Elabd A, Attia E. Pediatric and adolescent Lisfranc injuries — presentation, treatment and outcomes. Foot (Edinb) 2021;46:101737.
- Herrera-Soto JA, Scherb M, Duffy MF, Albright JC. Fractures of the fifth metatarsal in children and adolescents. J Pediatr Orthop 2007;27:427-431.
- Daniels CJ, Morrell AP. Chiropractic management of pediatric plantar fasciitis: A case report. J Chiropr Med 2012;11:58-63.
- Swischuk LE, Jadhav SP. Ankle and foot. In: Swischuk LE, Jadhav SP, eds. Emergency Musculoskeletal Imaging in Children. Springer;2014:183-216.
- Solove M, Turcotte Benedict F. Ankle injuries in the pediatric emergency department. Pediatr Emerg Care 2020;36:248-254.
- Ellenbogen AL, Rice AL, Vyas P. Retrospective comparison of the Low Risk Ankle Rules and the Ottawa Ankle Rules in a pediatric population. Am J Emerg Med 2017;35:1262-1265.
- Boutis K, Komar L, Jaramillo D, et al. Sensitivity of a clinical examination to predict need for radiography in children with ankle injuries: A prospective study. Lancet 2001;358:2118-2121.
- Stiell I, Wells G, Laupacis A, et al. Multicentre trial to introduce the Ottawa ankle rules for use of radiography in acute ankle injuries. Multicentre Ankle Rule Study Group. BMJ 1995;311:594-597.
- MacDonald J, Rodenberg R, Sweeney E. Acute knee injuries in children and adolescents: A review. JAMA Pediatr 2021;175:624-630.
- Coleman N. Common Pediatric Knee Injuries: Best Practices in Evaluation and Management. Springer Nature; 2020.
- Duthon VB. Acute traumatic patellar dislocation. Orthop Traumatol Surg Res 2015;101(Suppl):S59-67.
- Sweeney E, Rodenberg R, MacDonald J. Overuse knee pain in the pediatric and adolescent athlete. Curr Sports Med Rep 2020;19:479-485.
- Shea KG, Musahl V, Stavinoha TJ. Editorial commentary: Anterolateral ligament-anatomy, evaluation, and future applications to knee stability. Arthroscopy 2019;35:2143-2145.
- Fabricant PD, Kocher MS. Management of ACL injuries in children and adolescents. J Bone Joint Surg Am 2017;99:600-612.
- Pache S, Aman ZS, Kennedy M, et al. Posterior cruciate ligament: Current concepts review. Arch Bone Jt Surg 2018;6:8-18.
- Bellisari G, Samora W, Klingele K. Meniscus tears in children. Sports Med Arthrosc Rev 2011;19:50-55.
- Kocher MS, Logan CA, Kramer DE. Discoid lateral meniscus in children: Diagnosis, management, and outcomes. J Am Acad Orthop Surg 2017;25:736-743.
- Kessler JI, Jacobs JC, Cannamela PC, et al. Childhood obesity is associated with osteochondritis dissecans of the knee, ankle, and elbow in children and adolescents. J Pediatr Orthop 2018;38:e296-e299.
- Conrad JM, Stanitski CL. Osteochondritis dissecans: Wilson’s sign revisited. Am J Sports Med 2003;31:777-778.
- Gans I, Baldwin KD, Ganley TJ. Treatment and management outcomes of tibial eminence fractures in pediatric patients: A systematic review. Am J Sports Med 2014;42:1743-1750.
- Sessions WC, Herring M, Truong WH. Extensor mechanism injury in the pediatric population — a clinical review. J Knee Surg 2018;31:490-497.
- Hunt DM, Somashekar N. A review of sleeve fractures of the patella in children. Knee 2005;12:3-7.
- Basener CJ, Mehlman CT, DiPasquale TG. Growth disturbance after distal femoral growth plate fractures in children: A meta-analysis. J Orthop Trauma 2009;23:663-667.
- Siow HM, Cameron DB, Ganley TJ. Acute knee injuries in skeletally immature athletes. Phys Med Rehabil Clin N Am 2008;19:319-345, ix.
- Schroeder PB, Nicholes MA, Schmitz MR. Hip injuries in the adolescent athlete. Clin Sports Med 2021;40:385-398.
- Kovacevic D, Mariscalco M, Goodwin RC. Injuries about the hip in the adolescent athlete. Sports Med Arthrosc Rev 2011;19:64-74.
- Jacoby L, Yi-Meng Y, Kocher MS. Hip problems and arthroscopy: Adolescent hip as it relates to sports. Clin Sports Med 2011;30:435-541.
- Eberbach H, Hohloch L, Feucht MJ, et al. Operative versus conservative treatment of apophyseal avulsion fractures of the pelvis in the adolescents: A systematical review with meta-analysis of clinical outcome and return to sports. BMC Musculoskelet Disord 2017;18:162.
- Adkins 3rd SB, Figler RA. Hip pain in athletes. Am Fam Physician 2000;61:2109-2118.
- Kocher MS, Tucker R. Pediatric athlete hip disorders. Clin Sports Med 2006;25:241-253, viii.
- Rebich EJ, Lee SS, Schlechter JA. The S sign: A new radiographic tool to aid in the diagnosis of slipped capital femoral epiphysis. J Emerg Med 2018;54:835-843.
Musculoskeletal injuries are common in pediatric patients. It is important to recognize the difference between pediatric and adult injury patterns to optimize management. The authors focus on the diagnostic evaluation and treatment of acute pediatric sports-related lower extremity injuries in the emergency department.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
