Diagnosing and Managing Pediatric Foreign Body Ingestions: Part I
AUTHORS
Ethan Gerdts, MD, Department of Emergency Medicine, University of North Carolina, Chapel Hill
Daniel Migliaccio, MD, Clinical Assistant Professor, Ultrasound Fellowship Director, Department of Emergency Medicine, University of North Carolina, Chapel Hill
PEER REVIEWER
Steven M. Winograd, MD, FACEP, Attending Emergency Physician, Keller Army Community Hospital, West Point, NY
Pediatric foreign bodies are common, with a diversity of presentations from the benign to the life-threatening. Every clinician must be prepared to recognize and manage this common reason for a visit to an acute care setting. Part I focuses on diagnosing foreign bodies, whereas Part II will tackle management strategies.
— Ann M. Dietrich, MD, FAAP, FACEP, Editor
Introduction
Pediatric foreign body ingestion comes with a dichotomous presentation to the emergency department (ED) — the child in extremis with a clear need for immediate intervention vs. the well-appearing child with unknown ingestion.1,2 This creates a challenge for the emergency medicine provider to use a combination of history, physical examination, different imaging modalities, and overall clinical picture to verify ingestion over aspiration and, furthermore, to determine whether there is any need for immediate intervention. The decision-making tree surrounding foreign body ingestion changes based on time course, type of object, location in the gastrointestinal tract, and size. Therefore, a regimented and practical approach to foreign body ingestions is warranted. Part I of this review will focus on diagnosing foreign body ingestions, and Part II will explore foreign body management in detail.
Epidemiology
Foreign body ingestion is an extremely common reason for a child to present to a pediatric ED. In a typical year, it is estimated that anywhere between 100,000 and 200,000 visits are attributed to this chief complaint.3-6 The typical demographic has a slightly male skew (54% vs. 46%) and most commonly presents in children older than 6 months but younger than 5 years of age, with the average age being 6 to 36 months.1,3,7,8
In typical cases, or around 80% of the time, foreign body ingestions are uncomplicated and do not necessitate further workup after initial imaging and examination.9 However, in approximately 10% to 20% of cases, there is a need for endoscopic removal because of the object’s location, size, or characteristics.1,6,9-12 One study even suggested that nearly 8% of all endoscopies performed over a 10-year period were attributed to foreign body ingestions and their associated removal.6,9-11 Less than 1% of cases will require surgery under general anesthesia.12 Approximately 2% to 7% of cases result in “complications,” which can include hemorrhage, infection, perforation, fistula formation, or obstruction.1,6,12-14 Death is exceedingly rare from foreign body ingestion, although it has been reported.7,9,15 As expected, the incidence of complication increases linearly with time since ingestion and also is dependent on the type of ingestion.12 Additionally, if the patient has a history of prior ingestion or has an intent of self-harm with the ingestion, the complication rate also is higher.13
Ingestion events usually are purposeful but without intent at self-harm because of the age range of the pediatric population.6,9,16,17 Foreign body ingestions occur in the 6- to 36-month-old range largely because of normal developmental stages. Children in this age range tend to explore and examine objects by using their hands and mouth, which leads to an increased risk of ingestion.8,9,16-18
Commonly ingested items include shiny or small objects, balls, toys, and magnets. Because of their lack of development, the pediatric population often is unable to distinguish between what is edible and what is not, especially with objects that may take on the appearance of food.16 Other etiologies of foreign body ingestion are physiologic, since this age group typically lacks the dentition necessary to sufficiently break up larger objects, which can lead to food boluses and ingestion of nonfood items.16,19 Lack of experience with orofacial coordination contributes to these ingestion events as well.19
Lastly, ingestions can take place because of distraction, like when a child is simultaneously eating and playing, then accidentally ingests the object they are playing with instead of the intended food item.16 Recurrent foreign body ingestion (RFBI) is a rare phenomenon in the pediatric population.2,20,21 In pediatrics, two subgroups are at a particularly high risk of RFBI: children with mental/cognitive impairment and children who have severe mental health/psychiatric issues.16,18,20,21 Outside of the normal treatment algorithm discussed in detail in this review, special inpatient and outpatient treatment is warranted for these subgroups. (See the upcoming March 2022 Pediatric Emergency Medicine Reports).
Distinguishing Between Aspiration and Ingestion
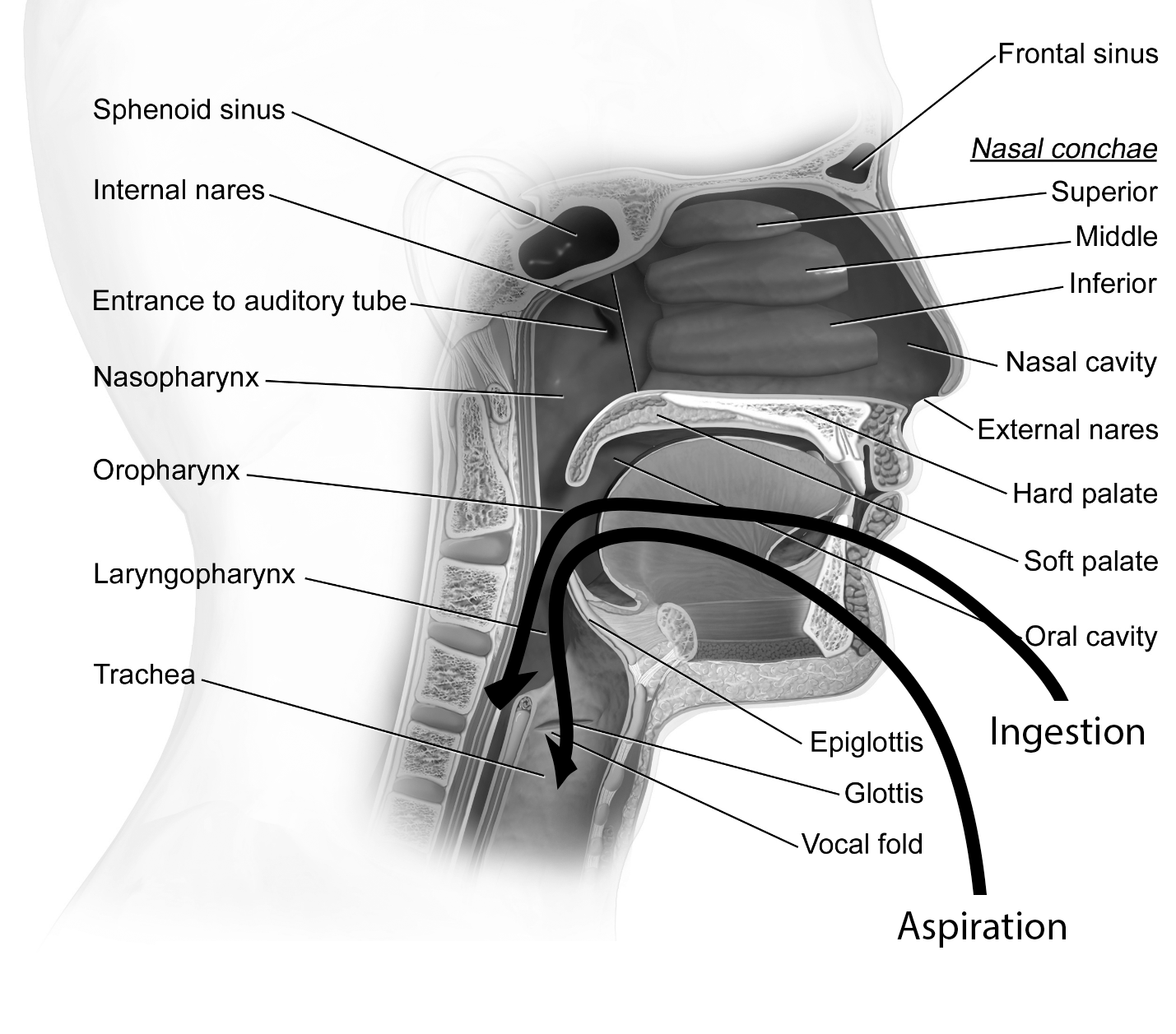
When a suspected foreign body ingestion occurs, it is of paramount importance to ensure it is an ingestion rather than an aspiration event. As detailed in Figure 1, ingestion implies passage through the oropharynx, posterior to the epiglottis and into the esophagus. Aspiration implies that the object has passed through the oropharynx, then into the larynx and anterior to the epiglottis, and has entered the trachea or other sub-tracheal structures. Foreign body aspirations are outside the scope of this review; however, it is an important branch point in overall management. Given that aspiration and ingestion both can present with overlapping symptoms, including cough, choking, or respiratory distress (symptomatology detailed later), it may be necessary to obtain imaging to ascertain where the foreign body actually is located.
Figure 1. Aspiration vs. Ingestion in the Early Gastrointestinal Tract |
Adapted from Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). doi: 10.15347/wjm/2014.010 |
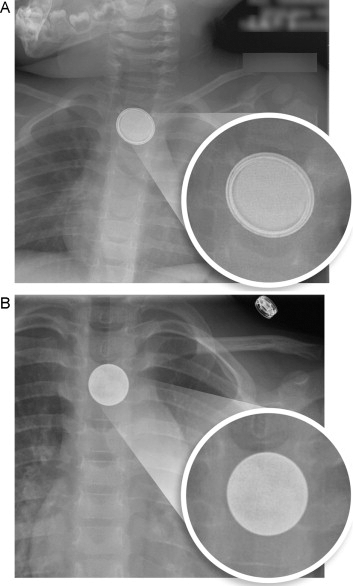
Nearly all ingestion events warrant plain radiographs to determine the location of the object. On an anteroposterior (AP) radiograph, which, ideally, includes the neck, chest, and whole abdomen, the object may be visualized either in the esophagus or the trachea. Lateral neck films also may be helpful in determining which structure the object has entered. For example, with coin ingestions, AP films will show the coin face in the AP direction, whereas, in a lateral radiograph, it will appear in a coronal plane. With coin aspirations, however, the AP film will show the coin on end, whereas the lateral radiograph will show the coin’s face. This is detailed in Figure 2.
Figure 2. Radiograph of an Ingested Coin |
 |
Because the face of the coin is visible on anteroposterior films, this coin has been ingested. A coin visible on end on anteroposterior radiographs indicates that it has been aspirated. Samir. Foreign body aspiration. Published June 6, 2006. https://commons.wikimedia.org/wiki/File:Foreign_body_aspiration.jpg |
However, it should be noted that, although this general rule often is accurate, like most rules in medicine, it is not without exception. Aspirated foreign bodies may take on the appearance on plain film of an ingested foreign body and vice versa, which may necessitate further imaging.22,23 In fact, there even may be spontaneous reorientation of the object within its respective location.23 If aspiration is suspected, providers can obtain inspiratory/expiratory films assessing for lung hyperinflation on the ipsilateral side of ingestion or lateral decubitus films assessing for lung collapse.
For examples, visit https://bit.ly/3HFdE50. The panels show inspiratory and expiratory films showing lung hyperinflation on the ipsilateral side of foreign body aspiration. In addition, visit https://bit.ly/3n3BnUt. The left panel is a left lateral decubitus X-ray demonstrating air trapping in the left lung without physiological lung collapse. The black arrows in the image outline the lateral aspect of the lung. The right panel is a right lateral decubitus X-ray demonstrating physiological lung collapse with left-side pneumothorax. White arrows outline the lateral aspect of the lung.
One study suggested very limited utility of decubitus imaging, producing a sensitivity of 27% and a specificity of 67%, although other studies have suggested a sensitivity up to 50% and a specificity up to 70%.24,25 Reportedly, decubitus imaging adds only false positives without increasing true positives.25 Clinical suspicion and a history consistent with aspiration were more predictive of a true positive foreign body aspiration.24,25,26
Plain radiographs are useful only in cases of a radiopaque ingested object, which has been estimated to be approximately 60% to 70% of the time.6,27 Foreign bodies that are aspirated are radiolucent around 80% of the time.28 This discrepancy is intriguing — it is thought that the radiodensity difference between the aspirated and ingested foreign bodies is because of the type of object.26,28 Aspirated foreign bodies often are smaller and very likely to be food items, like nuts, which are radiolucent, whereas ingested foreign bodies are larger and more commonly toy items or household objects, which are more likely to be radiopaque.26,28
Despite the frequency of ingested radiopaque items, other commonly ingested items include wood or plastic items, meat bones, and glass objects, which are radiolucent.1,6 It is recommended that, if the object is radiolucent and a high clinical suspicion for ingested foreign body remains, the provider should proceed with endoscopy for exploration and/or removal, rather than other imaging studies like computed tomography.6,29 Magnetic resonance imaging (MRI) also is an option to visualize a radiolucent object, although availability, speed, and cost are potential barriers to its widespread use.14,29
Pathophysiology
Foreign bodies can become lodged anywhere along the gastrointestinal (GI) tract, but they tend to lodge in places of anatomical narrowing near the opening of the tract.7,30-32 The most common site, accounting for more than 60% of cases, is at the level of the thoracic inlet. On radiographs, the thoracic inlet appears to be at the level of the clavicles, which is, anatomically, at the cricopharyngeus muscle.18,30-32 Foreign bodies also can be lodged at the level of the aortic arch and at the gastroesophageal junction, which appear on radiographs at the level of the carina and just above the stomach bubble, respectively.6,18,30,33
Patients may present with foreign body ingestion that have passed into the stomach, duodenum, or further along the GI tract, which, as discussed later, greatly affects their overall disposition. Anatomically narrow sites further in the GI tract where providers might find a foreign body include the duodenal curve and the ileocecal valve.6,18,30,33 It is worth mentioning the clinical features and pathophysiology that relate to specific objects, which can help immediately determine their projected disposition.
Batteries
Batteries, particularly button batteries, necessitate immediate endoscopic removal if located in the esophagus, ideally less than two hours from the time of ingestion, to help prevent severe complications.18,34 The battery can immediately start releasing acidic compounds and cause direct caustic injury within minutes.18,34 Within two hours, widespread tissue liquefactive necrosis of the GI tract can occur, which can rapidly progress to perforation.18,34-37
The degree of injury can vary based on voltage, size, and amount of contact with the surrounding tissue. This contact closes off the electrical circuit of the battery, releasing hydroxide ions into the surrounding tissue and causing an alkaline injury, namely necrosis from tissue liquefaction.34
The most immediate concern with these ingestions is perforation secondary to necrotic mucosa, but even after the battery’s removal, long-term complications can occur, such as strictures, esophageal stenosis, mediastinitis, fistula formation (tracheoesophageal), aortoesophageal, or nerve damage, depending on how long the battery was in the esophagus prior to removal and how much damage was sustained.34 Documentation should dictate what kind of battery was ingested after removal as well as voltage, size, and metal type, since these all can affect overall prognosis.34,35,37 In particular, lithium batteries are known to have higher rates of morbidity and complication, which is thought to be because of their increased voltage.18,38 These specifics should be asked of the caregiver if the information is readily available.
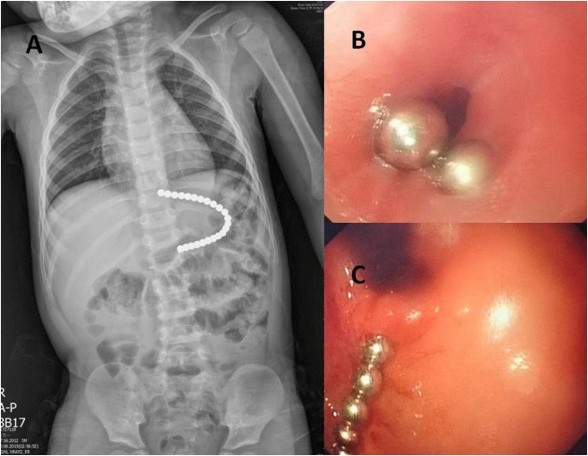
Unfortunately, ingestion of button batteries is quite common, accounting for approximately 11% of all ingested objects.9 The first step of workup should be determining the battery’s anatomical location through a radiograph or radiographs, keeping in mind that button batteries can easily be confused for coins on plain-film imaging. They can be distinguished from coins by the presence of the “double halo” around the rim of the circular foreign body (see Figure 3), although there are exceptions to this rule.34,39
Figure 3. Battery Halo Sign on Radiograph |
Anteroposterior radiograph demonstrating the difference in appearance between a button battery (panel A, with “halo sign”) and a coin (panel B, no “halo sign”), both in the esophagus. Reprinted with permission from Jatana KR, Litovitz T, Reilly JS, et al. Pediatric button battery injuries: 2013 task force update. Int J Pediatr Otorhinolaryngol 2013;77:1392-1399. |
If clinical suspicion is high enough, the absence of the double halo sign does not definitively rule out button battery ingestion.39 Some sources suggest that, on initial imaging, if button batteries have already passed the esophagus and are in the stomach or intestines, these patients can be observed rather than whisked to the endoscopy suite, although there is no widely accepted guideline.34,39,40 If the patient is stable after observation, repeat imaging to ensure advancement in addition to exploration of the child’s excrement to ensure passage are necessary given the toxic nature of the battery.
For assistance in managing button battery ingestions and reporting of the incident, the provider or family should contact the National Button Battery Ingestion Hotline (National Capital Poison Center, Washington, D.C.) at 800-498-8666 at any time of day or see their contact information on their website, found at www.poison.org/battery.18,34
Magnets
Magnets, especially with ingestion of multiple magnets, have become increasingly common in the last decade because of more advanced toys and household equipment.9,40,41 The magnets that have the highest incidence of morbidity are neodymium magnets, also known as rare-earth magnets, which are present in toys, puzzles, fidget spinners, cordless household tools, and hard drives.40-42 These are fairly new in discovery, with the U.S. Consumer Product Safety Commission issuing their first warning about harm from this specific type of magnet ingestion in 2007.41
The primary cause of morbidity with these ingestions usually occurs when more than one magnet is ingested, which can result in direct pressure necrosis. The magnets are attracted to one another in different parts of the gastrointestinal tract, then pinch the mucosal surfaces between the two magnets, causing ischemia, pressure necrosis, or bowel perforation.40,41,43,44 Other potential consequences include fistula formation, obstruction, or volvulus.40,41,44
Unlike with batteries, the location of the magnets within in the GI tract once they have passed the esophagus does not change management. Generally, single magnet ingestions are allowed to pass spontaneously and can proceed with regular radiographs to document progression. It has been estimated that when patients present with magnetic foreign body, they have ingested multiple magnets 20% of the time.43
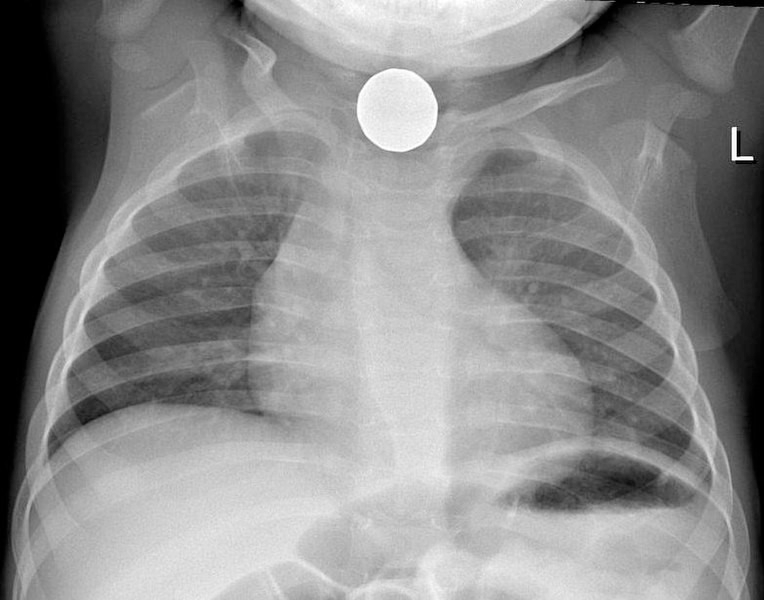
If multiple magnets (or a co-ingestion of a magnet with a metal object) are discovered, then an emergent consult for immediate removal by pediatric gastroenterology and/or pediatric surgery is warranted regardless of where they are located within the GI tract.41,43 Figure 4 shows multiple ingested neodymium magnets that necessitated removal — note their attraction to one another.
Figure 4. Neodymium Magnet Ingestion as Seen During Endoscopy |
Neodymium magnet ingestion as seen during endoscopy. Note their linear appearance secondary to their strong attraction to one another. Reprinted with permission from Chao H-C, Chang C-H, Chan O-W. Multiple magnets trapped at the esophagogastric junction of a child. Pediatr Neonatol 2018;59:205-207. |
Sharp Objects
Sharp objects (nails, pins, tacks, sharp bones, etc.) are considered high-risk ingestions because of the significant complications associated with them, including up to a 35% rate of perforation if found distal to the stomach.2,34,36,45 Bowel perforation, foreign body migration with subsequent damage to other organs, fistula formation, abscess, and peritonitis are possible complications depending on the composition, size, and orientation of the sharp object.2,45 Many sources abide by “Jackson’s axiom,” first mentioned in a 1937 study of more than 3,000 patients, in which Jackson and Jackson published the oft-mentioned “advancing points puncture, trailing do not.”46 However, in present-day clinical practice, determining which direction the sharp object is facing is not only difficult, it should not be used as a reliable method of guiding the management of the patient’s ingestion, since objects can change orientation within the GI tract.
As with other ingestions, plain radiographs should be obtained and, if it is radiopaque, the object needs to be removed unless in the distal small bowel or if the object has a known heavier blunt end that would assist in passage.2,6 If the object is radiolucent on plain radiograph but the ingestion was witnessed or self-reported, endoscopy is warranted.2,6 If radiolucent and unwitnessed, advanced imaging can be considered if the patient is asymptomatic for a trial of conservative/expectant management.2 The American Society for Gastrointestinal Endoscopy guidelines recommends removal of sharp objects if found at or proximal to the duodenum.18,47 If distal to the duodenum, they recommend daily radiographs with surgical consultation if any abdominal symptoms develop or if three days have passed since ingestion without expulsion of the object.18,47
Toxidromes and Pharmaceutical Foreign Body Ingestion
Foreign body ingestion also includes both accidental and purposeful ingestion of toxic substances, including medications, household items, and nonpharmacologic oils. Ingestion of these substances has myriad clinical presentations depending on what substance was ingested, which is largely out of the scope of this review. However, common household and “one-pill” toxic ingestions are paramount to consider during initial evaluation of a patient where the object ingested is unknown, particularly if the patient is unstable or in distress. This type of injury represents a significant proportion of foreign body ingestion, outnumbering the rate of nonpharmaceutical consumer product poisonings.48,49 In addition, it has been estimated that around 70,000 annual visits are made for pediatric medication overdose, although it remains unclear how many of those ingestions overlap with the diagnosis of “foreign body ingestion” as mentioned above.48
“One-pill” or “one-sip” ingestions refer to a group of common medications that may be present within any given household that can be fatal when ingested by children.48-50 The list of such medications continues to grow, having doubled since 2004, with the rise of new medication classes like direct oral anticoagulants (DOACs), newer antiepileptic drugs, phosphodiesterase-5 inhibitors (PDE-5), and new antipsychotic drugs.50,51 This growing list of medications, seen in detail in Table 1 (available online at https://bit.ly/3qjXTdF), was created because of the high morbidity/mortality associated with their ingestion. Some antidotes for these exist and are mentioned in the table, and if clinical suspicion is high given the patient’s presentation, antidotes should be given to mitigate or reverse the toxic effects of the ingestion.
Body Packing and Body Stuffing as Foreign Body Ingestion
Although quite rare and likely limited to the older end of the pediatric scale, body packing and body stuffing also can present as foreign body ingestion. Body packing is defined as the premeditated intra-abdominal transport of usually large quantities of drugs, most commonly heroin or cocaine.52 Body stuffing involves either rapid ingestion or placement of drugs within body orifices, such as the rectum or vagina, to conceal them out of concern for the patient’s arrest if they were to be discovered.52,53 Stuffing is not premeditated, so the substance often is not wrapped appropriately and may carry a higher risk of incidental systemic intoxication. Systemic opioid intoxication manifests as respiratory depression, miosis, and central nervous system depression, whereas systemic cocaine intoxication manifests as a sympathomimetic toxidrome that may include tachycardia, diaphoresis, mydriasis, agitation, and hallucinations. Systemic symptoms may only be apparent if the container the illicit substance is in has ruptured. Otherwise, the patient may be completely asymptomatic.
Body packing and stuffing are so concerning because there may be extreme doses of the illicit substance, leading to uncommon complications. For opioid derivatives, this would include coma, apnea, and death, whereas for sympathomimetics, this can include seizures, myocardial infarction, hemorrhagic stroke, severe renal impairment, and rhabdomyolysis.52-55 Management of this niche complaint varies from traditional foreign body ingestion because patients usually are admitted to monitor for systemic toxicity secondary to packet rupture, but rarely require invasive removal.52,53 Complications are rare, necessitating operative intervention in around 2% of cases.52
Clinical Features and Common Complaints
Ingestion-related clinical features and projected clinical course are directly related to the type of object ingested and time since the ingestion, which is directly related to the location of the object within the GI tract, as previously mentioned. The type of object ingested can be divided into high-risk and low-risk objects. High-risk ingestions include batteries, multiple magnets, sharp objects, items containing toxic compounds, and ingestions of any sort when the patient has undergone previous GI surgery.3,7,9,10,15,33,38 Low-risk ingestions include small coins, small plastic toys without sharp edges, other inert objects, and food boluses as long as the patient is tolerating secretions.3,7,18,38 As seen in Table 2, the patient’s clinical course may change based on the risk stratification of the ingested object.
Table 2. Risk Stratification of Ingestions3,7,9,10,18,38 | ||
High-Risk Ingestions |
Low-Risk Ingestions | |
Object |
Potential Complication |
|
Batteries (especially button/disc) |
Erosion, perforation | |
Multiple or neodymium magnets |
Obstruction | |
Sharp objects |
Perforation | |
Lead paint/imported toys |
Lead toxicity | |
Animal bones |
Erosion/fistula | |
Blunt objects > 5 cm |
Obstruction | |
Laundry detergent pods/caustic materials |
Erosion, mucosal injury | |
Time since ingestion, which helps determine the location within the GI tract, needs to be obtained early, since it is the most important factor that governs the patient’s clinical course. The location within the GI tract also can yield a different group of symptoms. For example, an object found within the esophagus can present with globus sensation and cough, but an object found within the stomach can simply present with abdominal pain. Chief complaint, however, is not a reliable indicator of the foreign object’s exact location within the GI tract. The wide array of presenting clinical features makes these patients clinically complex.
Patients with foreign body ingestion often will be completely asymptomatic. Some studies have estimated that asymptomatic patients account for 40% to 50% of all patients who have ingested something.5,27 Symptomatic patients can have nonspecific complaints, such as cough, sore throat, vomiting, or wheezing, which easily can be confused for primary intrapulmonary pathology.5,15,27 A high clinical suspicion for foreign body ingestions, especially when the patient likely is too young to provide an accurate history, is necessary to ensure that these ingestions are not missed.
There are more specific findings for foreign body ingestion that patients can present with, although they are less common. These signs/symptoms include pain (specifically in the neck), globus sensation, stridor, and drooling. It should be noted that, in patients who are preverbal, irritability, fussiness, food refusal, weight loss, and postprandial emesis always should prompt consideration of foreign body ingestion on the differential diagnosis.5,9,15,18,27,35,36 These symptoms are summarized in Table 3 (available online at https://bit.ly/33p9vDk).
Differential Diagnosis
Although the differential can vary based on the patient’s chief symptom, common themes emerge in constructing a differential diagnosis. If the patient presents with respiratory symptoms like cough, wheezing, or fever, primary intrapulmonary pathology, including upper respiratory infection, pneumonia, or obstructive lung disease like asthma, foreign body should be added to the differential.
A patient’s previous medical history and pertinent family history become quite important, especially regarding wheezing and coughing, since a strong family history of asthma or atopy can favor a non-ingestion-related cause to their symptoms. Any fever present should prompt an infectious workup (or at least pertinent positive and negative history-taking to rule in or out an infectious explanation of the patient’s symptoms).
GI symptoms tend to be more specific for foreign body ingestion, including globus sensation, abdominal pain, odynophagia, or dysphagia. A common mimic for foreign body ingestion is mucosal irritation within the esophageal lining. This can be caused by direct mucosal trauma by an ingestion event when the object in question has already passed into the lower GI tract but has caused damage in the more proximal GI tract, resulting in the patient’s symptoms. Often, the workup for mucosal damage is identical, since the two presentations are quite difficult to distinguish, and direct visualization of the mucosa or advanced imaging is warranted. Despite their increased specificity, these symptoms also could be consistent with pharyngitis or laryngitis, which should remain on the differential.
Preverbal patients are more undifferentiated because they cannot assist in the history. Fussiness, decreased sleep, weight loss, postprandial emesis, or food refusal is concerning in the young pediatric patient or neonate and should be taken seriously by all providers. The differential often can include more serious etiologies, such as serious bacterial infection, congenital malformation (obstruction, volvulus, or pyloric stenosis), or inborn disorder of the metabolism. This differential varies widely based on the patient’s age and is outside the scope of this review. Drooling and stridor are concerning symptoms in a patient and prompt immediate evaluation of the patient’s ability to protect the airway. Drooling also can be associated with altered mental status, intoxication, or dysregulation of a patient’s hormones (such as excess catecholamines or hypersalivation from toxidrome), although these may be less acute presentations. Additionally, stridor can indicate severe upper respiratory infection, airway edema, or recent trauma to the neck or upper airway structures and may necessitate placing a definitive airway depending on the patient’s vital signs and overall appearance.
Conclusion
Although management will be discussed in Part II, pediatric foreign body ingestion has been demonstrated throughout this review to be a common problem that easily can be overlooked. High-risk objects can cause devastating complications, including hollow viscus perforation, obstruction, or fistula formation, if they are not detected early. Object size, sharpness, and composition, in addition to early identification of the object’s location within the GI tract, are vital components to determine the trajectory of the patient’s workup and management. A high clinical suspicion and a comprehensive history-taking by the provider is necessary to minimize the risk of complication.
REFERENCES
- Chen MK, Beierle EA. Gastrointestinal foreign bodies. Pediatr Ann 2001;30:736-742.
- Kramer RE, Lerner DG, Lin T, et al; North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition Endoscopy Committee. Management of ingested foreign bodies in children: A clinical report of the NASPGHAN Endoscopy Committee. J Pediatr Gastroenterol Nutr 2015;60:562-574.
- Orsagh-Yentis D, McAdams RJ, Roberts KJ, McKenzie LB. Foreign-body ingestions of young children treated in U.S. emergency departments: 1995-2015. Pediatrics 2019;143:e20181988.
- Bronstein AC, Spyker DA, Cantilena LR Jr, et al. 2011 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 29th Annual Report. Clin Toxicol (Phila) 2012;50:911-1164. [Erratum in Clin Toxicol (Phila) 2014;52:1286-1287].
- Fung BM, Sweetser S, Wong Kee Song LM, Tabibian JH. Foreign object ingestion and esophageal food impaction: An update and review on endoscopic management. World J Gastrointest Endosc 2019;11:174-192.
- Uyemura MC. Foreign body ingestion in children. Am Fam Physician 2005;72:287-291. [Erratum in: Am Fam Physician 2006;73:1332].
- Conners GP, Mohseni M. Pediatric foreign body ingestion. In: StatPearls [Internet]. StatPearls Publishing; 2021.
- Gilger MA, Jain AK. Foreign bodies of the esophagus and gastrointestinal tract in children. UpToDate. Updated Dec. 10, 2020. https://www.uptodate.com/contents/foreign-bodies-of-the-esophagus-and-gastrointestinal-tract-in-children
- Khorana J, Tantivit Y, Phiuphong C, et al. Foreign body ingestion in pediatrics: Distribution, management, and complications. Medicina (Kaunas) 2019;55:686.
- Wyllie R. Foreign bodies in the gastrointestinal tract. Curr Opin Pediatr 2006;18:563-564.
- Denney W, Ahmad N, Dillard B, Nowicki MJ. Children will eat the strangest things: A 10-year retrospective analysis of foreign body and caustic ingestions from a single academic center. Pediatr Emerg Care 2012;28:731-734.
- Yuan J, Ma M, Guo Y, et al. Delayed endoscopic removal of sharp foreign body in the esophagus increased clinical complications: An experience from multiple centers in China. Medicine (Baltimore) 2019;98:e16146.
- Palta R, Sahota A, Bemarki A, et al. Foreign-body ingestion: Characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc 2009;69(3 Pt 1):426-433.
- Dahshan A. Management of ingested foreign bodies in children. J Okla State Med Assoc 2001;94:183-186.
- Gurevich Y, Sahn B, Weinstein T. Foreign body ingestion in pediatric patients. Curr Opin Pediatr 2018;30:677-682.
- Passali D, Gregori D, Lorenzoni G, et al. Foreign body injuries in children: A review. Acta Otorhinolaryngol Ital 2015;35:265-271.
- Jaan A, Mulita F. Gastrointestinal foreign body. In: StatPearls [Internet]. StatPearls Publishing; 2021.
- Bono MJ. Esophageal emergencies. In: Tintinalli JE, Ma O, Yealy DM, et al, eds. Tintinalli's Emergency Medicine: A Comprehensive Study Guide. 9th ed. McGraw Hill;2020:500-504.
- Kim SI, Lee KM, Choi YH, Lee DH. Predictive parameters of retained foreign body presence after foreign body swallowing. Am J Emerg Med 2017;35:1090-1094.
- Kapalu CL, Lantos J, Booser A, et al. Preventing self-harm from repeat foreign-body ingestion. Pediatrics 2020;145:e20191515.
- Low Kapalu CM, Ibrahimi N, Mentrikoski JM, Attard T. Pediatric recurrent intentional foreign body ingestion: Case series and review of the literature. J Pediatr Gastroenterol Nutr 2020;71:232-236.
- Tiedeken SD, Shaffer SE. Worrisome chronic cough in a 3-year-old. Contemp Pediatr 2014;31;23,39-40.
- @Roshcast. In what orientation do coins typically appear on a lateral X-ray when in the trachea? Why? Twitter. Published Dec. 20, 2017. https://twitter.com/roshcast/status/943479877738606594?lang=en
- Lin CH, Chen AC, Tsai JD, et al. Endoscopic removal of foreign bodies in children. Kaohsiung J Med Sci 2007;23:447-452.
- Schlesinger AE, Crowe JE. Sagittal orientation of ingested coins in the esophagus in children. AJR Am J Roentgenol 2011;196:670-672.
- Ruiz FE. Airway foreign bodies in children. UpToDate. Updated May 19, 2010. https://somepomed.org/articulos/contents/mobipreview.htm?23/51/24368
- Newby MD, Thomas D, Mullett CJ, et al. Foreign body aspiration presenting as pneumothorax in a child. Cureus 2020;12:e8161.
- Assefa D, Amin N, Stringel G, Dozor AJ. Use of decubitus radiographs in the diagnosis of foreign body aspiration in young children. Pediatr Emerg Care 2007;23:154-157.
- Brown JC, Chapman T, Klein EJ, et al. The utility of adding expiratory or decubitus chest radiographs to the radiographic evaluation of suspected pediatric airway foreign bodies. Ann Emerg Med 2013;61:19-26.
- Arana A, Hauser B, Hachimi-Idrissi S, Vandenplas Y. Management of ingested foreign bodies in childhood and review of the literature. Eur J Pediatr 2001;160:468-472.
- Mu LC, Sun DQ, He P. Radiological diagnosis of aspirated foreign bodies in children: Review of 343 cases. J Laryngol Otol 1990;104:778-782.
- Eisen GM, Baron TH, Dominitz JA; American Society for Gastrointestinal Endoscopy, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc 2002;55:802-806.
- Joyamaha D, Conners GP. Managing pediatric foreign body ingestions. Mo Med 2015;112:181-186.
- Hesham A-Kader H. Foreign body ingestion: Children like to put objects in their mouth. World J Pediatr 2010;6:301-310.
- Kay M, Wyllie R. Pediatric foreign bodies and their management. Curr Gastroenterol Rep 2005;7:212-218.
- Rybojad B, Niedzielska G, Niedzielski A, et al. Esophageal foreign bodies in pediatric patients: A thirteen-year retrospective study. ScientificWorldJournal 2012;2012:102642.
- Jatana KR, Litovitz T, Reilly JS, et al. Pediatric button battery injuries: 2013 task force update. Int J Pediatr Otorhinolaryngol 2013;77:1392-1399.
- Swaminathan A. Button battery ingestion. REBEL EM. Published Sept. 4, 2017. https://rebelem.com/button-battery-ingestion/
- WikEM. Ingested foreign body. Updated Nov. 1, 2021. http://www.wikem.org/wiki/ingested_foreign_body
- National Capital Poison Control. National Capital Poison Center button battery ingestion triage and treatment guideline. Updated June 2018. https://www.poison.org/battery/guideline
- Jayachandra S, Eslick GD. A systematic review of paediatric foreign body ingestion: Presentation, complications, and management. Int J Pediatr Otorhinolaryngol 2013;77:311-317.
- Shaker L, Santos C. TOXcard: Button battery ingestions. emDocs. Published Sept. 26, 2018. http://www.emdocs.net/toxcard-button-battery-ingestions/
- Tenenbein M. Foreign bodies. In: Tenenbein M, Macias CG, Sharieff GQ, et al, eds. Strange and Schafermeyer's Pediatric Emergency Medicine. 5th ed. McGraw Hill;2018:47-54.
- Hussain SZ, Bousvaros A, Gilger M, et al. Management of ingested magnets in children. J Pediatr Gastroenterol Nutr 2012;55:239-242.
- Agbo C, Lee L, Chiang V, et al. Magnet-related injury rates in children: A single hospital experience. J Pediatr Gastroenterol Nutr 2013;57:14-17.
- Tavarez MM, Saladino RA, Gaines BA, Manole MD. Prevalence, clinical features and management of pediatric magnetic foreign body ingestions. J Emerg Med 2013;44:261-268.
- Strickland M, Rosenfield D, Fecteau A. Magnetic foreign body injuries: A large pediatric hospital experience. J Pediatr 2014;165:332-335.
- Chao H-C, Chang CH, Chan OW. Multiple magnets trapped at the esophagogastric junction of a child. Pediatr Neonatol 2018;59:205-207.
- ASGE Standards of Practice Committee; Ikenberry SO, Jue TL, Anderson MA, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc 2011;73:1085-1091.
- Jackson C, Jackson CL. Disease of the air and food passages of foreign body origin. Laryngoscope 1936;46:814.
- Anderson KL, Dean AJ. Foreign bodies in the gastrointestinal tract and anorectal emergencies. Emerg Med Clin North Am 2011;29:369-400, ix.
- Schillie SF, Shehab N, Thomas KE, Budnitz DS. Medication overdoses leading to emergency department visits among children. Am J Prev Med 2009;37:181-187.
- Farrell NM, Hamilton S, Gendron BJ, et al. Presence of “one pill can kill” medications in medication organizers: Implications for child safety. J Pharm Pract 2021:8971900211017491. [Online ahead of print].
- Koren G, Nachmani A. Drugs that can kill a toddler with one tablet or teaspoonful: A 2018 updated list. Clin Drug Investig 2019;39:217-220.
- Bar-Oz B, Levichek Z, Koren G. Medications that can be fatal for a toddler with one tablet or teaspoonful: A 2004 update. Paediatr Drug 2004;6:123-126.
Pediatric foreign body ingestion comes with a dichotomous presentation to the ED — the child in extremis with a clear need for immediate intervention vs. the well-appearing child with unknown ingestion. This creates a challenge for the emergency medicine provider to use a combination of history, physical examination, different imaging modalities, and overall clinical picture to verify ingestion over aspiration and, furthermore, to determine whether there is any need for immediate intervention. The decision-making tree surrounding foreign body ingestion changes based on time course, type of object, location in the gastrointestinal tract, and size. Therefore, a regimented and practical approach to foreign body ingestions is warranted.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.