AUTHORS
Alfred C. Gitu, MD, FAAFP, Program Director and Associate Professor of Family Medicine, The Florida State University COM Family Medicine Residency Program at Lee Health, Fort Myers, FL
Hailon Wong, MD, Assistant Professor of Family Medicine, The Florida State University COM Family Medicine Residency Program at Lee Health, Fort Myers, FL
PEER REVIEWER
Harvey S. Hahn, MD, FACC, Cardiovascular Fellowship Training Program and Co-Director, KPN CV Quality, Kettering Medical Center; Associate Professor of Clinical Medicine, Wright State University Boonshoft School of Medicine, Kettering, OH, and Loma Linda, CA
EXECUTIVE SUMMARY
- Most major international guidelines define hypertension in adults as systolic blood pressure in the office or clinic as
≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg. - Although ambulatory monitoring of blood pressures is preferred for diagnosis and confirmation of office readings, this remains impractical for many patients, and office-based measurements remain the most common means of diagnosis.
- Among secondary causes, renal disease, sleep apnea, medications, and hyperaldosteronism are among the more common causes. Consider these diagnoses in patients with severe hypertension, age of onset younger than 30 years (especially in the absence of clear risk factors), or an acute rise in blood pressure after a period of good control.
- Ideally, blood pressure should be obtained using an automated oscillometric device. Multiple measurements should be obtained and averaged. Some of the newer oscillometric devices can inflate automatically, allowing the patient to be alone when the blood pressure is measured.
- Measurements obtained by averaging multiple automated measurements while the patient remains alone in the room are aligned more closely with ambulatory measurements and offer more standardized and reproducible evaluation.
- Resistant hypertension is diagnosed when a patient takes three antihypertensive agents with complementary mechanisms of action (including a diuretic) without achieving blood pressure control, or when blood pressure control is achieved but requires four or more medications.
- Although lifestyle modifications are important and a cornerstone of management, most patients diagnosed with hypertension will go on to require pharmacotherapy. Thiazide diuretics, angiotensin converting enzyme inhibitors, angiotensin receptor blockers, and calcium channel blockers are first-line options either alone or in combination.
How many patients do you see who come to the emergency department (ED) because of an elevated blood pressure but are otherwise asymptomatic? If your ED is like mine, a fair number. The numbers seem to be increasing, I suspect because of the proliferation of home blood pressure monitoring, the difficulty with primary care access, and the aging population. Ideally, after a history and physical examination to assess that they are truly asymptomatic, you would like to send them on their way with primary care follow-up. Unfortunately, that is not always realistic. My most recent patient was sent from his oral surgeon’s office because of an elevated blood pressure, and the oral surgeon would not perform the scheduled root canal procedure until the patient’s blood pressure was normal. The patient had called his primary care provider, but the office would not make an appointment because he had not seen the physician in more than a year and, therefore, was considered an inactive patient. He had called several other practices, and they were not taking on new patients either. So here he was, in my ED. Like it or not, I had to deal with his hypertension. I suspect some of you have found yourselves in similar circumstances. This issue — on the assessment and initiation of treatment of hypertension — should be useful to you in these circumstances.
— Joseph Stephan Stapczynski, MD, Editor
Definition
Most major international guidelines define hypertension in adults as systolic blood pressure (SBP) in the office or clinic as ≥ 140 mmHg and/or diastolic blood pressure (DBP) ≥ 90 mmHg.1-4 In 2017, the American College of Cardiology/American Heart Association (ACC/AHA) released guidelines defining stage 1 hypertension in adults as a systolic blood pressure of 130 mmHg to 139 mmHg or a diastolic reading of 80 mmHg to 89 mmHg. Stage 2 hypertension is defined as a blood pressure ≥ 140/90 mmHg.2 These guidelines are based largely on the results of the SPRINT trial, which found improved overall and cardiovascular mortality with targeting a systolic blood pressure of < 120 mmHg compared to < 140 mmHg. However, these recommendations are not without controversy. For example, blood pressure measurements were based on the average of three automated readings after the patient had been seated for five minutes, which is in contrast to how most measurements actually are obtained in routine clinical practice.5
Other organizations have derived their own definitions based on review and interpretation of other data sources. For example, the European Society of Cardiology and European Society of Hypertension (ESC/ESH) and the International Society of Hypertension (ISH) define hypertension as an SBP of ≥ 140 mmHg or DBP ≥ 90 mmHg when office-based measurement is used.1,3 The ISH further recommends a threshold of > 160/100 mmHg as grade 2 hypertension. The American Academy of Family Physicians continues to endorse the findings of the Eighth Joint National Committee (JNC 8), which defines hypertension as > 140/90 mmHg in the general population and > 150/90 mmHg in adults older than 60 years of age.4
More recently, there has been an attempt to use different definitions based on setting, time of day, and age. To illustrate: Although the ACC/AHA uses a threshold of 130/80 mmHg in the office setting, when 24-hour ambulatory monitoring is used, the proposed cutoff is slightly less, at 125/75 mmHg.2 Similarly, when 24-hour ambulatory monitoring is used, the ESC/ESH guidelines define hypertension as a blood pressure > 130/80 mmHg.3 (See Table 1.)
Table 1. Definitions of Hypertension | ||||
|
International Society of Hypertension Practice Guidelines |
European Society of Cardiology/European Society of Hypertension |
American College of Cardiology/American Heart Association |
Eighth Joint National Committee (JNC 8) | |
|
Year of Publication |
2020 |
2018 |
2018 |
2013 |
|
Definition | ||||
|
1. Clinic BP |
SBP ≥ 140 mmHg |
SBP ≥ 140 mmHg and/or |
SBP ≥ 130 mmHg |
Age 18 to 59 years: Age 60 years and older: SBP ≥ 150 mmHg |
|
2. Self-Measured Home BP |
SBP ≥ 135 mmHg |
SBP ≥ 135 mmHg and/or |
SBP ≥ 130 mmHg |
N/A |
|
3. Average 24-Hour ABP |
SBP ≥ 130 mmHg |
SBP ≥ 130 mmHg and/or |
SBP ≥ 125 mmHg |
N/A |
|
4. Average Daytime ABP |
SBP ≥ 135 mmHg |
SBP ≥ 135 mmHg and/or |
SBP ≥ 130 mmHg |
N/A |
|
5. Average Nighttime ABP |
SBP ≥ 120 mmHg |
SBP ≥ 120 mmHg and/or |
SBP ≥ 110 mmHg |
N/A |
|
BP: blood pressure; DBP: diastolic blood pressure; SBP: systolic blood pressure; ABP: ambulatory blood pressure Adapted from: Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020;75:1334-1357. | ||||
Out-of-office blood pressure measurements are performed by patients at home using automated blood pressure monitors or ambulatory blood pressure monitoring (ABPM). According to the United States Preventive Services Task Force (USPSTF), blood pressure measurements obtained in this way are more reproducible and accurate predictors of hypertension-induced organ damage and cardiovascular events than office-based measurements.6 Although ambulatory monitoring of blood pressures is preferred for diagnosis and confirmation of office readings, this remains impractical for many patients, and office-based measurements remain the most common means of diagnosis. The different definitions are summarized in Table 1.
Epidemiology
Following the ACC/AHA definition, the prevalence of hypertension among U.S. adults would be more than 45%, with medication recommended for 36.2% of U.S. adults.7,8 The prevalence is higher in men than in women, 51% vs. 39.7%, respectively, and with increasing age. A National Center for Health Statistics (NCHS) report published by the Centers for Disease Control and Prevention (CDC) found that the prevalence was 22.4% among adults ages 18 to 39 years but rose to 74.5% among those older than 60 years of age. The age-adjusted prevalence was highest among non-Hispanic Black adults (57.1%) compared to non-Hispanic white (43.6%) and Hispanic (43.7%) adults.8 The burden of hypertension is high and becoming higher, particularly in low- and middle-income countries where access to antihypertensive medication is limited.8,9
Hypertension remains the leading cause of death and disability-adjusted life years (DALYs) globally, accounting for 10.4 million deaths per year.9 In the United States, hypertension accounts for more cardiovascular disease (CVD) deaths than any other modifiable risk factor and is second only to cigarette smoking as a preventable cause of death for any reason.2 Additionally, the risk of CVD increases in a log-linear fashion from SBP < 115 mmHg to > 180 mmHg, with each 20 mmHg increase in SBP corresponding to a doubling of the risk of death from stroke, heart disease, or other vascular disease. Furthermore, the increased risk of CVD is reported across a broad age spectrum, from 30 to 80 years of age and older.2
Etiology
There is no one unifying etiology of hypertension, but it can be divided roughly into primary and secondary types, with primary being the most prevalent, accounting for 90% to 95% of cases.1,10
Among cases of primary hypertension, a number of risk factors have been identified, including age, race, obesity, and family history. Lifestyle factors, including high sodium diet, physical inactivity, stress, and tobacco and alcohol use, also are important risk factors.1
Among secondary causes, renal disease, sleep apnea, medications, and hyperaldosteronism are among the more common causes. Consider these diagnoses in patients with severe hypertension, age of onset younger than 30 years (especially in the absence of clear risk factors), or an acute rise in blood pressure after a period of good control. Table 2 summarizes potential etiologies or contributors of secondary hypertension along with diagnostic clues in the history and physical examination that would prompt additional workup.2,10
Table 2. Secondary Causes of Hypertension | |||
|
Potential Cause |
Prevalence in Patients with Hypertension |
History, Physical, or Laboratory Findings |
Diagnostic Workup |
|
Obstructive sleep apnea |
25% to 50% |
|
|
|
Primary hyperaldosteronism |
8% to 20% |
|
|
|
Renal artery stenosis |
5% to 34% |
|
|
|
Renal parenchymal disease |
1% to 2% |
|
|
|
Drugs/substances |
2% to 4% |
|
|
|
Thyroid disorders |
< 1% |
|
|
|
Pheochromocytoma |
0.1% to 0.6% |
|
|
|
Cushing syndrome |
< 0.1% |
|
|
|
Coarctation of the aorta |
0.1% |
|
|
|
ACE-I: angitotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; NSAIDs: nonsteroidal anti-inflammatory drugs; OCP: oral contraceptive pill; SSRI: selective serotonin reuptake inhibitor; MAOI: monoamine oxidase inhibitor; TCA: tricyclic antidepressant; TSH: thyroid-stimulating hormone; MR: magnetic resonance; CT: computed tomography Adapted from: Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:1269-1324 and Charles L, Triscott J, Dobbs B. Secondary hypertension: Discovering the underlying cause. Am Fam Physician 2017;96:453-461. | |||
Pathophysiology
The exact mechanism by which hypertension develops is not entirely clear, but, in most cases, hypertension in adults involves multiple causes, including genetic, environmental, neural, hormonal, and anatomic factors interacting together in what has been termed the “mosaic model.”11
In addition, a typical Western diet, high in red meat, fat, and processed foods, has been known to promote inflammation and atherosclerosis, resulting in hypertension. Alternatively, a diet rich in fruits, vegetables, and reduced saturated fat and cholesterol has been shown to reduce systolic blood pressure.12,13 Body mass index (BMI) and waist circumference also share a nearly linear relationship with hypertension.2
Clinical Features
Except for clinical features of secondary hypertension and signs and symptoms of end-organ damage from hypertensive emergency, hypertension typically is asymptomatic. It usually is brought to clinical attention when the blood pressure is assessed during a routine clinical interaction or referred to the clinic or emergency department from outside sources when it is noted to be elevated unexpectedly.
On history and physical examination, note any risk factors, such as obesity, and assess for signs of hypertensive complications and secondary etiologies. Common complications of hypertension include congestive heart failure, chronic kidney disease, sexual dysfunction, peripheral artery disease, and blindness, in addition to heart attack and stroke.1,2,14
Hypertensive emergency may present with headache, visual changes, chest pain, dizziness, and shortness of breath among other symptoms.15 When evaluating a patient with significantly elevated blood pressure (> 180/110 mmHg), take a careful history, specifically asking for signs of end-organ damage. Severe asymptomatic hypertension — sometimes termed hypertensive urgency — which does not involve end-organ damage, generally can be managed in the outpatient setting with oral medications and close follow-up.15
Diagnostic Studies
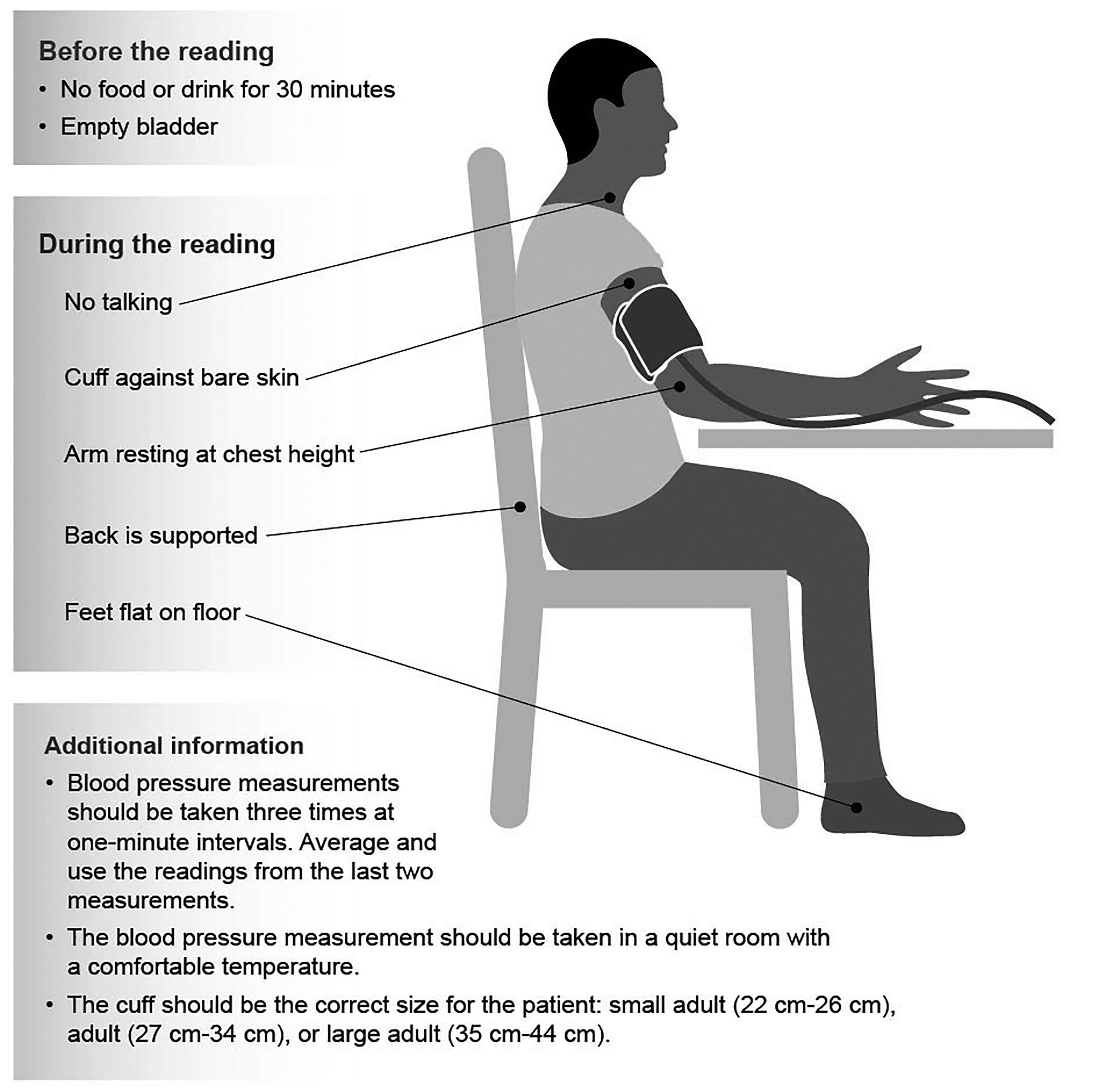
The most important next step in the diagnosis of hypertension is to ensure the blood pressure is measured accurately. (See Figure 1 and Table 3.)
Figure 1. Measuring Blood Pressure |
|
Adapted from: Centers for Disease Control and Prevention. The correct way to measure blood pressure. https://www.cdc.gov/heartdisease/images/AHM2020_BP_Infographic.jpg and Centers for Disease Control and Prevention, Effective Diagnosis, Treatment, and Monitoring of Hypertension in Primary Care, Participant Guide 2, Measurement of Blood Pressure, https://www.cdc.gov/globalhealth/healthprotection/ncd/training/files/Session2_ParticipantGuide.pdf |
Table 3. Recommendations for Taking Blood Pressure Measurements |
|
Conditions for the Measurement
Positioning the Patient
Measurement Device
Choosing the Correct Cuff
Measurement Protocol
Interpreting the Results
|
|
Adapted from: Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020;75:1334-1357. |
Measurement of blood pressure is the most common basis for diagnosis and follow-up of hypertension. It is recommended that elevated blood pressure be confirmed during two to three visits at one- to four-week intervals rather than at a single office visit unless the blood pressure is > 180/110 mmHg and/or there is evidence of cardiovascular disease.2 Whenever possible, confirm the diagnosis with out-of-office measurements, namely home blood pressure or 24-hour ambulatory blood pressure monitoring.
Ideally, blood pressure should be obtained using an automated oscillometric device. Multiple measurements should be obtained and averaged. Some of the newer oscillometric devices can inflate automatically, allowing the patient to be alone when the blood pressure is measured.1
Measurements obtained by averaging multiple automated measurements while the patient remains alone in the room are aligned more closely with ambulatory measurements and offer more standardized and reproducible evaluation.2 These readings also are often lower than those obtained through usual practice. Furthermore, rechecking the blood pressure of a patient whose initial reading was elevated can result in a lower systolic reading of a median of 8 mmHg, resulting in an increased hypertension control rate from 61% to 73%, according to one study published in the Journal of the American Medical Association (JAMA) Internal Medicine involving 38,620 primary care patients diagnosed with hypertension.16
Measure the blood pressure in both arms and, if noted to be consistently different between arms by > 10 mmHg, use the higher of the two readings. If the difference is > 20 mmHg, consider further evaluation with CT/MR angiography to evaluate for coarctation or subclavian artery obstruction.
Because hypertension is a major cardiovascular risk factor, obtain a thorough history and physical examination and assess the hypertensive patient for overall cardiovascular risk and signs of organ dysfunction. Additional cardiovascular risk factors are found in more than half of all patients with hypertension.2 These confer increased risk of coronary, cerebrovascular, and renal disease in hypertensive patients. The most common additional risk factors include obesity (49.5%), diabetes (27.2%), dyslipidemia (63.2%), and chronic kidney disease (15.8%).2
The ISH recommends obtaining a serum sodium, potassium, creatinine, fasting glucose, and lipid profile, in addition to a urinalysis and electrocardiogram, in all adults with a new diagnosis of hypertension.1 The ACC/AHA recommends these in addition to a complete blood count, calcium, and thyroid-stimulating hormone.2 The American College of Emergency Physicians Clinical Policy from 2013 issued a level C recommendation that ED patients with asymptomatic markedly elevated blood pressure do not require routine screening for organ injury, e.g., serum creatinine, urinalysis, or electrocardiogram. In patients with poor follow-up, screening for an elevated serum creatinine may be considered to identify renal injury that could affect disposition.17 These recommendations are summarized in Table 4.
Table 4. ISH, ACC/AHA, and ACEP Initiation Testing Screening Recommendations | ||
|
ISH |
ACC/AHA |
ACEP |
|
|
No routine screening for acute target organ injury (e.g., serum creatinine, urinalysis, ECG) is required. In select patient populations (e.g., poor follow-up), screening for an elevated serum creatinine level may identify kidney injury that affects disposition (e.g., hospital admission). |
|
ISH: International Society of Hypertension; ACC: American College of Cardiology; AHA: American Heart Association; ACEP: American College of Emergency Physicians; ECG: electrocardiogram | ||
The USPSTF recommends using the Pooled Cohort Equations from the American College of Cardiology to assess 10-year risk of a cardiovascular event. For asymptomatic adults with low risk, defined as 7.5% or less, it also recommends against screening with resting or exercise electrocardiography to prevent cardiovascular disease, citing lack of benefit and potential for harm.18 Additional studies, such as echocardiography, renal artery imaging, carotid ultrasound, and sleep study, are not indicated routinely but may be reasonable, depending on the history and physical exam. For example, a 67-year-old with a smoking history and symptoms of claudication should be screened additionally for abdominal aortic aneurysm and vascular studies, such as ankle-brachial index.
Differential Diagnosis
White Coat Hypertension
This refers to individuals who have elevated blood pressure only in the clinic or ED, with normal ambulatory or home blood pressure. When untreated, this category of patients has been associated with cardiovascular risk intermediate between those with normal blood pressure and those with hypertension.1 If the overall cardiovascular risk, calculated using a validated tool, is low and there is no evidence of hypertension-mediated end organ damage, pharmacological treatment may be deferred. Lifestyle modifications should be recommended, and the patient should be followed closely for development of sustained hypertension requiring pharmacological treatment. The ACC/AHA 2017 guidelines recommend screening adults with untreated blood pressure > 130/80 mmHg but < 180/100 mmHg for white coat hypertension using am-bulatory or home blood pressure monitoring before making the diagnosis of hypertension.2
Masked Hypertension
This refers to individuals whose blood pressure readings in the office are normal, but who have elevated ambulatory or home blood pressure. When untreated, these patients have a similar risk for cardiovascular events as those with overt, sustained hypertension and may be offered drug treatment with the goal of normalizing their out-of-office blood pressure.1
Resistant Hypertension
Resistant hypertension is diagnosed when a patient takes three antihypertensive agents with complementary mechanisms of action (including a diuretic) without achieving blood pressure control, or when blood pressure control is achieved but requires four or more medications. On the basis of a 140/90 mmHg cutoff, the prevalence of resistant hypertension in the adult population is 13%.19 Risk factors for resistant hypertension include older age, obesity, chronic kidney disease, Black race, and diabetes.19 The risk of stroke, myocardial infarction, and death with resistant hypertension was significantly higher than in hypertensive patients without resistant hypertension.20
Do not confuse resistant hypertension with secondary hypertension. Secondary hypertension refers to hypertension caused by a specific separate etiology. Furthermore, neither term should be confused with uncontrolled hypertension, which is an umbrella term for hypertension that is not at goal and includes cases related to a suboptimal treatment regimen or medication nonadherence.1
Management
The approach to management should include both blood pressure control to normal range and the effective treatment of other known risk factors. Use a validated tool to calculate overall cardiovascular risk with the aim to simultaneously address modifiable risk factors, such as obesity, smoking, and diabetes. Statin medications, when indicated, should be prescribed. This strategy reduces the rate of cardiovascular disease beyond what can be achieved with blood pressure control alone.1,2
Lifestyle Modifications
Lifestyle modification is the first-line antihypertensive treatment and also can enhance the efficacy of other therapies for hypertension. Healthy lifestyle choices can reverse, delay, or prevent the onset of elevated blood pressure and, additionally, attenuate cardiovascular risk.2 However, it is important to note that lifestyle modifications alone should not be used if a patient is determined to be at high risk for CVD, the blood pressure is ≥ 160/100 mmHg, or if appropriate reduction is not achieved within three to six months.1 A summary of lifestyle modifications and their expected effect on SBP is presented in Table 5.
Table 5. Lifestyle Modifications for Hypertension | ||
|
Intervention |
Notes |
Approximate Effect in mmHg on SBP (Hypertensive Patients) |
|
Healthy (DASH) diet |
-11 | |
|
Reduced dietary sodium |
|
-5 to -6 |
|
Moderation of
|
|
-4 |
|
Increased intake of dietary potassium |
|
-4 to -5 |
|
Regular physical activity |
|
- 5 to -8 -5 |
|
Weight reduction |
|
-5 |
|
SBP: systolic blood pressure Adapted from: Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:1269-1324. | ||
Pharmacologic Treatment
A difference in blood pressure of 20/10 mmHg is associated with more than a 50% reduction in cardiovascular risk in hypertensive patients 40 to 69 years of age.21 As such, all patients who are candidates for pharmacologic treatment of hypertension should receive adequate and efficacious antihypertensive medications with a goal to reduce blood pressure to < 140/90 mmHg within three to six months in most cases. Additionally, if coronary artery disease, prior stroke, diabetes, chronic kidney disease, or congestive heart failure is noted, treat to a target of < 130/80 mmHg unless the patient is elderly, in which case a target of < 140/90 mmHg should be used.1
Recommendations for the initial antihypertensive agents of choice have differed over the years. The ACC/AHA guidelines recommend initiation of therapy with any agent from the first-line classes of antihypertensive agents, namely thiazide diuretics, angiotensin converting enzyme inhibitors (ACE-I), angiotensin receptor blockers (ARB), or calcium channel blockers (CCB). Dosage titration and sequential addition of other first-line agents to achieve the blood pressure target also are recommended.2
However, based on data finding that most patients will require combination therapy, the ESC/ESH and ISH guidelines both recommend starting with combination therapy of two first-line agents, preferably as an affordable, single, once-daily combination pill. If blood pressure is not at goal with the maximum dose of two first-line agents, a third first-line agent should be added and titrated as appropriate.1,3 This largely is in line with the ACC/AHA recommendations, which recommend consideration of starting with two agents of different classes for patients with blood pressure ≥ 140/90 mmHg, which they define as stage 2 hypertension.2 Patients with blood pressure unresponsive to three first-line agents are considered to have resistant hypertension, and another agent, such as spironolactone, may be added. These patients also should be evaluated for secondary hypertension or medication and/or lifestyle nonadherence.1,2
The ACC/AHA guidelines also state that in Black adults with hypertension but without heart failure or chronic kidney disease, including those with diabetes, initial antihypertensive therapy should include a thiazide diuretic or CCB unless there is a compelling reason to use an ACE-I or ARB, such as microalbuminuria or heart failure with reduced ejection fraction (HFrEF).2
Beta-adrenergic blocking agents are not included among first-line agents for hypertension and should not be used for control of blood pressure unless there is another compelling reason for their use (e.g., thoracic aortic disease, recent myocardial infarction, or HFrEF).
The American College of Emergency Physicians Clinical Policy from 2013 issued a level C recommendation that ED patients with asymptomatic markedly elevated blood pressure do not require routine medical intervention. In patients with poor follow-up, emergency physicians may treat markedly elevated blood pressure in the ED and/or initiate therapy for long-term control.17 Medications commonly used for the treatment of hypertension are summarized in Table 6.
Table 6. Antihypertensive Medications | ||
|
Class |
Drugs and Usual Starting Dose/Day |
Notes |
|
Primary Agents | ||
|
Thiazide diuretics |
Chlorthalidone 12.5 mg; indapamide 1.25 mg; hydrochlorothiazide 25 mg; metolazone 2.5 mg |
Chlorthalidone preferred because of longer half-life and proven reduction of cardiovascular disease |
|
Angiotensin converting enzyme inhibitors (ACE-I) |
Lisinopril 5 mg to 10 mg; enalapril 5 mg; captopril 25 mg (12.5 mg 2-3 times daily); ramipril 2.5 mg; benazepril 5 mg to |
Should not be used in combination with ARB or direct renin inhibitor; avoid in pregnancy |
|
Angiotensin receptor blockers (ARBs) |
Candesartan 8 mg; irbesartan 150 mg; losartan 25 mg; olmesartan 20 mg; valsartan 80 mg |
Should not be used in combination with ACE-I or direct renin inhibitor; avoid in pregnancy |
|
Calcium channel blockers: dihydropyridines |
Amlodipine 2.5 mg to 5 mg; felodipine |
Caution in HFrEF; dose-related pedal edema is more common in women |
|
Calcium channel blockers: nondihyrdropyridines |
Diltiazem ER 120 mg; verapamil SR 120 mg |
Caution in combination with beta blockers or in patients with HFrEF |
|
Secondary Agents | ||
|
Diuretics: aldosterone antagonists |
Eplerenone 50 mg, spironolactone 25 mg |
Preferred agents in primary aldosteronism and resistant hypertension |
|
Diuretics: loop |
Bumetanide 0.5 mg, furosemide 20 mg, torsemide 5 mg |
Preferred diuretics in patients with symptomatic heart failure; preferred over thiazides in patients with GFR < 30 mL/min |
|
Diuretics: potassium-sparing |
Amiloride 5 mg, triamterene 50 mg |
Minimally effective for BP reduction |
|
Beta blockers: cardioselective |
Atenolol 25 mg, betaxolol 5 mg, bisoprolol |
Not recommended for hypertension unless patient has heart failure or ischemic heart disease. Use this category if beta blocker needed in patient with reactive airway disease. Nebivolol is also vasodilatory. Caution with abrupt cessation of all beta blockers |
|
Beta blockers: noncardioselective |
Nadolol 40 mg, propranolol 80 mg |
Caution in patients with reactive airway disease |
|
Beta blockers: combined alpha and beta receptor action |
Carvedilol IR 625 mg, carvedilol ER 20 mg, labetalol 200 mg |
Carvedilol is preferred in patients with HFrEF. Avoid abrupt cessation of all beta blockers |
|
Alpha-1 blockers |
Doxazosin 1 mg, prazosin 2 mg, terazosin 1 mg |
Orthostatic hypotension; may be considered second-line agents in patients with BPH |
|
Central alpha-2 agonists and other centrally acting agents |
Clonidine (oral and patch) 0.1 mg, methyldopa 250 mg, guanfacine 0.5 mg |
Agents of last resort because of central nervous system side effects; abrupt discontinuation of clonidine may induce hypertensive crisis |
|
Direct vasodilators |
Hydralazine 40 mg, minoxidil 5 mg |
Associated with water and sodium retention and reflex tachycardia; use with a diuretic and beta blocker; minoxidil associated with pericardial effusion and hirsutism and requires a loop diuretic |
|
LA: long acting; HFrEF: heart failure with reduced ejection fraction; ER: extended release; SR: sustained release; BP: blood pressure; IR: immediate release; GFR: glomerular filtration rate; BPH: benign prostatic hyperplasia | ||
To enhance adherence to therapy, the following strategies are suggested:
1. Physicians should assess for adherence as appropriate at each visit and, most importantly, prior to escalation of antihypertensive therapy.
2. Reduce polypharmacy by using single pill combinations.
3. Use once-daily dosing.
4. Advise home BP monitoring.
5. Use a multidisciplinary team approach (including pharmacists).
Clinicians should employ effective behavioral and motivational approaches to help patients achieve a healthy lifestyle. Team-based care for hypertension has been shown to improve blood pressure control and medication adherence. Such teams include the patient, their family, the primary care provider, and other professionals, such as cardiologists, nurses, pharmacists, social workers, community health workers, and dietitians. Use of the electronic health record and patient registries to identify patients with undiagnosed or undertreated hypertension also is recommended.1
Special Populations and Considerations
Pregnancy
Women with hypertension who become pregnant, or who are planning to become pregnant, should be transitioned to methyldopa, nifedipine, and/or labetalol during pregnancy. Because of the risk of fetal and neonatal morbidity and mortality, drugs that act directly on the renin-angiotensin system (ACE-Is, ARBs, and direct renin inhibitors) should not be used in pregnancy and should not be prescribed to women of child-bearing age who may become pregnant.2
Seasonal Blood Pressure Variation
Blood pressure changes have been noted with lower levels at higher temperatures and higher levels at lower temperatures. This occurs seasonally, as well as in people traveling from areas with cold to hot temperatures or vice versa. Studies have demonstrated an average change of 5/3 mmHg, with more marked fluctuations in patients on treatment for hypertension. This should be considered when symptoms of hypotension occur with increased temperature, or when blood pressure is below goal during cold weather in a person who previously was well controlled.1
Special Treatment Considerations
Consider therapeutic strategies that are effective both for hypertension as well as any comorbidities or cardiovascular risk factors. For example, in patients with hyperuricemia, in addition to dietary changes, medications that influence serum urate levels, such as losartan and atorvastatin, should be added to urate-lowering therapy.1 In addition, for patients with both diabetes and hypertension, first-line pharmacotherapy should include either an ACE-I or ARB if possible.3
Because peripheral edema is a common side effect of CCBs, such as amlodipine, use caution when prescribing these agents for patients with additional risk factors for peripheral edema, such as those with a diagnosis of congestive heart failure. Furthermore, for patients with both HFrEF and hypertension, a preference for agents with a proven mortality benefit (certain beta blockers and ACE-I/ARB) should be considered.2
Disposition
Adults initiating or adjusting to a new drug regimen for hypertension should have a follow-up evaluation for adherence and response to treatment at monthly intervals until control is achieved. At each follow-up visit, also monitor for adverse effects of medications and address any additional pertinent cardiovascular risk enhancers. After blood pressure control is achieved, office visits may be spaced to every three to six months, depending on additional comorbidities. Systematic strategies to help improve blood pressure control, including home blood pressure monitoring, team-based care (especially including pharmacists), and telehealth, should be employed after initiation of therapy as appropriate.1-3
Summary
Hypertension, defined by most major societies as > 140/90 mmHg, is common and the prevalence is increasing. Although the clinic remains the most common setting for diagnosis, out of clinic and 24-hour ambulatory monitoring should be used increasingly if possible. Hypertension is a major modifiable risk factor for cardiovascular disease and, after diagnosis, it is important to screen for additional modifiable risk factors and calculate the overall cardiovascular risk.
Suspect secondary causes if blood pressure is difficult to control or as otherwise guided by the clinical evaluation. Lifestyle modifications are important and are a cornerstone of management. However, most patients diagnosed with hypertension will go on to require pharmacotherapy. Thiazide diuretics, ACE-I, ARBs, and CCBs are first-line options either alone or in combination.
Monitor monthly and escalate therapy until blood pressure is controlled to < 140/90 mmHg or < 130/80 mmHg if certain comorbidities, such as coronary artery disease, congestive heart failure, diabetes, or chronic kidney disease, exist. A multidisciplinary approach, including physicians, nurses, pharmacists, and the use of technology, such as telehealth and electronic health record registries, also can improve adherence and achievement of control.
REFERENCES
- Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020;75:1334-1357.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:1269-1324.
- Williams B, Mancia G, Spiering W, et al; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the Management of Arterial Hypertension. Eur Heart J 2018;39:3021-3104.
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507-520.
- SPRINT Research Group; Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015;373:2103-2116.
- Guirguis-Blake JM, Evans CV, Webber EM, et al. Screening for hypertension in adults: Updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 2021;325:1657-1669.
- Muntner P, Carey RM, Gidding S, et al. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation 2018;137:109-118.
- Ostchega Y, Fryar CD, Nwankwo T, Nguyen DT. Hypertension prevalence among adults aged 18 and over: United States, 2017-2018. NCHS Data Brief 2020 Apr;(364):1-8.
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1923-1994.
- Charles L, Triscott J, Dobbs B. Secondary hypertension: Discovering the underlying cause. Am Fam Physician 2017;96:453-461.
- Harrison DG. The mosaic theory revisited: Common molecular mechanisms coordinating diverse organ and cellular events in hypertension. J Am Soc Hypertens 2013;7:68-74.
- Ruan Y, Huang Y, Zhang Q, et al. Association between dietary patterns and hypertension among Han and multi-ethnic population in southwest China. BMC Public Health 2018;18:1106.
- Juraschek SP, Miller ER 3rd, Weaver CM, Appel LJ. Effects of sodium reduction and the DASH diet in relation to baseline blood pressure. J Am Coll Cardiol 2017;70:2841-2848.
- U.S. Department of Health and Human Services. The Surgeon General’s Call to Action to Control Hypertension. https://www.hhs.gov/sites/default/files/call-to-action-to-control-hypertension.pdf
- Peixoto AJ. Acute severe hypertension. N Engl J Med 2019;381:1843-1852.
- Einstadter D, Bolen SD, Misak JE, et al. Association of repeated measurements with blood pressure control in primary care. JAMA Intern Med 2018;178:858-860.
- Wolf SJ, Lo B, Shih RD, et al. Clinical policy: Critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med 2013;62:59.
- U.S. Preventive Services Task Force. Final recommendation statement. Cardiovascular disease risk: Screening with electrocardiography. Published June 12, 2018. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/cardiovascular-disease-risk-screening-with-electrocardiography
- Persell SD. Prevalence of resistant hypertension in the United States, 2003-2008. Hypertension 2011;57:1076-1080.
- Smith SM, Gong Y, Handberg E, et al. Predictors and outcomes of resistant hypertension among patients with coronary artery disease and hypertension.J Hypertens 2014;32:635-643.
- Lewington S, Clarke R, Qizilbash N, et al; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903-1913.
Hypertension, defined by most major societies as > 140/90 mmHg, is common and the prevalence is increasing.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.