Fever in the Returning Pediatric Traveler
December 1, 2020
Related Articles
-
Infectious Disease Updates
-
Noninferiority of Seven vs. 14 Days of Antibiotic Therapy for Bloodstream Infections
-
Parvovirus and Increasing Danger in Pregnancy and Sickle Cell Disease
-
Oseltamivir for Adults Hospitalized with Influenza: Earlier Is Better
-
Usefulness of Pyuria to Diagnose UTI in Children
AUTHORS
Shyam Sivasankar, MD, Clinical Assistant Professor of Emergency Medicine, Stanford University School of Medicine, Stanford, CA
N. Ewen Wang, MD, Professor of Emergency Medicine, Stanford University School of Medicine, Stanford, CA
PEER REVIEWER
Katherine Baranowski, MD, FAAP, FACEP, Chief, Division of Pediatric Emergency Medicine, Department of Emergency Medicine, New Jersey Medical School, Rutgers, The State University of New Jersey
Executive Summary
• In terms of travel history, clinicians should inquire about pre-trip planning, including prophylactic medications and vaccinations. The trip destination, length of time spent per destination, and chronology of onset of fever and associated symptoms also should be detailed. The practitioner should inquire about environmental exposures, such as accommodations, swimming in fresh water, and animal exposure. Older children and young adults should be asked confidentially about sexual activities. Additionally, clinicians should ask about potential sources of infection via food, drink, and insect bites (mosquitoes, ticks, etc.).
• Rickettsial diseases, dengue, enteric fever, chikungunya, traveler’s diarrhea, influenza, Legionella, and viral hemorrhagic fevers tend to have short incubation periods, usually less than 10 days. Diseases with fevers persisting for greater than two weeks include malaria, schistosomiasis, toxoplasmosis, brucellosis, tuberculosis, Q fever, hepatitis, and amebic liver abscesses. Rickettsial infection fever, enteric fever, and viral hemorrhagic fevers can persist for more than two weeks.
• Certain physical exam findings may point to a specific diagnosis. For example, a relative bradycardia phenomenon can be seen with enteric fever and also can be occasionally encountered with rickettsial diseases. A thorough head, eyes, ears, nose, and throat examination may reveal conjunctivitis, which can be seen in patients with exposure to fresh water, possibly indicating leptospirosis, and in patients with Zika or chikungunya (also with eyelid swelling, as noted later). Conjunctival suffusion, photophobia, ocular pain, and conjunctival hemorrhage are specific findings for leptospirosis.
• Fever presenting with jaundice should prompt consideration of life-threatening diagnoses first, such as the viral hemorrhagic fevers (including Ebola, Marburg, and Lassa fever), malaria, severe dengue, and leptospirosis. Fever and jaundice also can be seen in viral hepatitis.
• Certain populations may be at a higher risk for developing severe infections. These include infants (< 3 months of age), unvaccinated or incompletely immunized children, and children with underlying chronic health conditions (diabetes, congenital heart issues, etc.). Additionally, those with immune disorders, both acquired (such as post-transplant patients and those undergoing chemotherapy) and congenital (functional asplenia, etc.), should be evaluated more thoroughly.
• Malaria remains the main cause of hospitalization and death for returning travelers. Malaria should be actively ruled out in all travelers to endemic areas regardless of medical prophylaxis.
• Falciparum malaria should be considered in all cases of unexplained fever starting at any time between seven days after the first possible exposure to malaria and three months after the last possible exposure.
• Symptoms of severe malaria include altered mental status, shock, acidosis, hypoglycemia, anemia, or evidence of end-organ dysfunction — and can accompany any of the subtypes of Plasmodium spp. Severe anemia is most likely to develop in children younger than 2 years of age, while cerebral malaria is more likely to occur in older children, with an mean age of 3.5 years. Microscopy, through identification of trophozoites on thin and thick peripheral blood smears, is the most common method for diagnosis.
• Salmonella enterica serotype Typhi is particularly notable because it can lead to typhoid or enteric fever which has a high fatality rate in children younger than 4 years of age, but it most commonly occurs in those between 5 and 12 years of age. Typical symptoms include fever, malaise, headache, anorexia, and abdominal symptoms, including abdominal pain, gastrointestinal bleeding, diarrhea, and constipation (which can be more common than diarrhea in older children).
• A common gastrointestinal symptom that often accompanies returning travelers is diarrhea. It is aptly named traveler's diarrhea when accompanied with a fever, or dysentery when there is bloody or mucoid stool. Although most diarrheal illnesses are likely viral and self-limited, the vast majority of travel-related diarrhea is bacterial in nature. Prolonged periods of diarrhea or bloody diarrhea tend to be bacterial, with common culprits being Salmonella spp., Escherichia coli, Shigella spp., and Campylobacter spp. The highest incidence of this subset of diarrheal illnesses occurs in children younger than 5 years of age, especially in infants younger than 1 year of age. It usually starts between days 4 and 14 after foreign arrival and lasts up to five days. Traveler’s diarrhea should be treated only if patients present with severe diarrhea (more than 10 loose stools per day), bloody stool, or high fever, or if patients require hospitalization as the result of dehydration or other complications. Azithromycin is agent of choice.
Although, currently, there are travel restrictions in many countries, this will pass. Acute care physicians need to have an awareness of diseases that are prevalent in other countries to accurately diagnose, manage, and treat patients traveling to and from other parts of the world. The authors present an incredibly valuable synopsis of fever and differential of fever in returning pediatric travelers.
— Ann M. Dietrich, MD, FAAP, FACEP, Editor
Introduction
In our increasingly global society, travel has become ubiquitous. Travel for business, pleasure, education, and to visit relatives has brought a new age of children accompanying their parents around the globe and adolescents exploring far corners of the world. With the growing ease of long-distance travel, there is a higher exposure to various infectious agents that are endemic to certain parts of the world. Additionally, emerging infectious diseases have become a worldwide threat because of the convenience and accessibility of global travel. Urbanization and destruction of natural habitats, climate change, changing ecosystems, changes in populations of reservoir hosts or intermediate insect vectors, and microbial genetic mutation all ahve contributed to the emergence and re-emergence of various infective agents.1 It has become of utmost importance to keep up to date on these emerging infectious trends so physicians can expand their differential diagnoses appropriately for these patients.
This article will review the broad category of fever in a returning pediatric traveler. First, the article will discuss epidemiology, followed by important aspects of the history and physical exam, differential diagnosis based on symptoms in conjunction with fever, and general management. Then, the article will cover four major causes of fever in the returned pediatric traveler in depth: malaria, enteric fever, dengue, and traveler’s diarrhea. That will be followed by an overview of other causes of fever in conjunction with various body-system-specific findings.
Epidemiology
In 2015, U.S. residents took more than 32 million trips overseas and a combined 40.5 million trips to Mexico and Canada. Overseas travel included 12.5 million (17%) visitors to Europe, 10.4 million (10%) to the Caribbean, 6.6 million (6.6%) to Asia, 4.6 million (6.3%) to Central and South America, 2 million (2.8%) to the Middle East, 640,000 (0.9%) to Oceania, and 350,000 (0.5%) to Africa. Although the exact number of children is unknown, within this cohort, 2.2 million were adults traveling with children, and 3.1 million travelers reported their occupation as students.2
Two pediatric populations are of specific concern. Although the large majority of people travel for tourism purposes (~55%), a significant proportion of families with children travel for the purpose of visiting friends and relatives (~21%).3 This travel cohort presents a specific challenge to providers because, as a whole, this group travels for longer periods of time and has a longer exposure to potentially infectious contacts. Sometimes, parents travelling “home,” underappreciate the severity of endemic diseases and may not have looked into pre-travel vaccinations or prophylaxis.
Additionally, according to the World Health Organization (WHO), adolescents and young adults make up the largest cohort of travelers by age.4 This group of travelers can be at risk when traveling on a limited budget, when they use poor-standard accommodations, when their activities involve exposure to fresh water, and when their lifestyle includes risky sexual behavior and recreational drug-related actions.
The History
Obtaining a travel history is an essential aspect of history taking, but the initial focus of identifying the cause of fever in children should include indicators of community-acquired disease processes. Pneumonia, viral upper respiratory tract infections, urinary tract infections, pyelonephritis, and viral gastroenteritis are common infections encountered in many cosmopolitan destinations across the globe. The initial differential should exclude these common contenders as the infectious source before focusing on more region-specific diagnoses. In terms of travel history, clinicians should inquire about pre-trip planning, including prophylactic medications and vaccinations. The trip destination, length of time spent per destination, and chronology of onset of fever and associated symptoms should be detailed. Remembering that infectious disease does not respect country boundaries, environmental conditions, such as rural vs. urban exposure (even within the United States), altitude, and seasonal variations should be taken into consideration.
In addition to identifying travel destinations, further details regarding specifics of travel are vital to identify potential disease vectors. The practitioner should inquire about environmental exposures, such as accommodations, swimming in fresh water, and animal exposure. Older children and young adults should be asked confidentially about sexual activities. Additionally, clinicians should ask about potential sources of infection via food, drink, and insect bites (mosquitoes, ticks, etc.).
Time from exposure to manifestation of symptoms (incubation time) can be a useful tool to help narrow down causative infectious agents. Rickettsial diseases, dengue, enteric fever, chikungunya, traveler’s diarrhea, influenza, Legionella, and viral hemorrhagic fevers tend to have short incubation periods, usually less than 10 days.
Diseases with fevers persisting for greater than two weeks include malaria, schistosomiasis, toxoplasmosis, brucellosis, tuberculosis, Q fever, hepatitis, and amebic liver abscesses. Rickettsial infections, enteric fever, and viral hemorrhagic fevers can have fevers persisting for longer than two weeks.
Evaluation and Diagnostic Testing
As always, management and diagnosis go hand in hand in emergency medicine. Patients should be resuscitated according to the standard airway, breathing, circulation (ABC) algorithm. After initial stabilization, patients with suspected sepsis as the result of rickettsial disease should receive empiric doxycycline regardless of age. Other patients with septic shock should be hydrated appropriately and started on empiric broad-spectrum antimicrobials. Similarly, patients with hemorrhagic disease should be treated with appropriate fluid resuscitation and blood products, depending on the situation. In patients with altered mental status, a thorough evaluation to exclude cerebral malaria should be performed.
Physical Exam
Examination should include a thorough physical exam. Certain physical exam findings may point to a specific diagnosis. For example, a relative bradycardia phenomenon can be seen with enteric fever and also can be occasionally encountered with rickettsial diseases. A thorough head, eyes, ears, nose, and throat examination may reveal conjunctivitis, which can be seen in patients with exposure to fresh water, possibly indicating leptospirosis, and in patients with Zika or chikungunya (also with eyelid swelling, as noted later). Conjunctival suffusion, photophobia, ocular pain, and conjunctival hemorrhage are specific findings for leptospirosis.5 Generalized lymphadenopathy can occur with enteric fever, leptospirosis, dengue fever, rickettisal disease, tuberculosis, and brucellosis. Many respiratory tract infections are viral in nature. Seasonal variations of influenza should be considered in the differential. In addition to common viral syndromes, bacterial pneumonia can present with cough and fever and should be higher on the differential in patients with focality on pulmonary auscultation.
Splenomegaly can be associated with malaria, brucellosis, and enteric fever. Right upper quadrant tenderness can be seen in hepatitis or amebiasis.
Sometimes, dermatologic findings may be the only indicator to identify the infectious agent. Nonspecific maculopapular rashes can appear with leptospirosis, dengue, Zika, and chikungunya. Petechiae, followed by purpura, can suggest pneumococcal meningitis, dengue fever, or other viral hemorrhagic fevers. Rose spots, or clusters of macules (usually 2 mm to
3 mm) on the trunk, can be seen in patients with enteric fever. Rickettsial infections tend to have an eschar left by a tick or chigger bite.
Fever presenting with jaundice should prompt consideration of life-threatening diagnoses first, such as the viral hemorrhagic fevers (including Ebola, Marburg, and Lassa fever), malaria (which will be discussed at length in a later section), severe dengue, and leptospirosis. Fever and jaundice also can be seen in viral hepatitis. Table 1 (available online at https://bit.ly/2JNwGxe) summarizes many of these diseases, their causes, and their associated historical clues.
Testing
Initial evaluation of fever in a returning traveler should include testing for common diseases, such as pneumonia, urinary tract infections, and influenza. Once these have been excluded, further diagnostic modalities should be used.
Basic bloodwork can include a complete blood count with differential, a comprehensive metabolic panel, and blood cultures. Dengue, chikungunya, Zika, rickettsial infections, and enteric fever all can present with leukopenia. As mentioned later, dengue also can be accompanied by thrombocytopenia, in which case the hemorrhagic variant of dengue should be considered. Specific testing, stool culture or gastrointestinal (GI) polymerase chain reaction, can be tailored to suspected infections for patients with diarrhea, etc.
Table 2 summarizes the symptoms, incubation periods, historical clues, and specific diagnostic testing for 12 diseases travelers may encounter.
Table 2. Tropical Disease Symptoms and Fever |
|||||
|
Disease Process |
Incubation Period |
Typical Symptoms (Excluding Fever) |
Historical Clues/ |
Specific |
Additional |
|
Chikungunya |
Two to four days |
Rash, arthralgia, myalgia, headache, conjunctivitis |
Mosquito bite (Aedes) |
Serology (IgM or IgG), viral PCR |
CBC (can show leukopenia) |
|
Zika |
Three days to two weeks |
Rash, arthralgia, myalgia, headache, conjunctivitis |
Mosquito bite (Aedes) |
Viral PCR |
CBC (can show leukopenia) |
|
Hepatitis A |
28 to 30 days |
Fever, malaise, anorexia, nausea, abdominal pain followed by jaundice a few days later |
Contaminated food or water, raw or undercooked shellfish, exposure to blood or body fluids, person-to-person contact (via fecal-oral route) |
Hepatitis A serology (IgM) |
Liver function testing (can show a hepatitic injury pattern), elevated PT/INR |
|
Brucellosis |
Two to three weeks |
Prolonged fever arthralgia, myalgia, headache, fatigue |
Unpasteurized milk or milk products, livestock exposure (slaughterhouse employees) |
Blood culture, BMAT serology |
|
|
Leptospirosis |
Seven to 12 days |
Rash, headache, myalgia, vomiting, conjunctivitis, abdominal pain; secondary phase symptoms can include liver or kidney failure and symptoms of meningitis |
Freshwater exposure; direct contact with urine from exposed animals or contact with water, soil, or food contaminated with the urine of infected animals |
Serology (MAT or IgM); urine testing |
Urinalysis |
|
Q fever |
Two days to six weeks |
Chills, fatigue, headache, maylgia, vomiting, diarrhea, abdominal pain |
Cow, sheep, goat exposure, including unpasteurized dairy products |
Serology, blood culture |
|
|
Spotted fevers |
Five to seven days |
Headache, rash, myalgia, eschar |
Tick bites |
Serology (IgG) |
|
|
Tick bite fever |
Five to seven days |
Eschar |
Tick bite, safaris, bush treks |
||
|
Scrub typhus |
One to two weeks |
Chills, headache, eschar, lymphadenopathy, rash |
Chigger bites |
Serology via IFA assay |
|
|
Amebiasis |
Two to four weeks, but can be years |
Fever, dysentery, chronic diarrhea, abdominal pain (especially in the right upper quadrant) |
Consumption of contaminated food or water |
E. histolytica serology, liver aspirate, liver ultrasound |
|
|
Pontiac fever |
12 to 36 hours |
Mild flu-like illness |
Hot tubs, hot water heaters, large plumbing systems, decorative fountains |
BAL, urine antigen testing |
Stool O&P, liver function testing |
|
Legionnaires' disease |
Two to 10 days |
Pneumonia-like illness with dyspnea, myalgia, headaches |
Hot tubs, hot water heaters, large plumbing systems, decorative fountains |
BAL, urine antigen testing |
Chest radiographs |
|
IgM: immunoglobulin M; IgG: immunoglobulin G; PCR: polymerase chain reaction; CBC: complete blood count; IgA: immunoglobulin A; BMAT: Brucella microagglutination test; MAT: microscopic agglutination test; IFA: indirect fluorescent antibody; BAL: bronchoalveolar lavage; PT/INR: prothrombin time/international normalized ratio; O&P: ova and parasites. |
|||||
Treatment
Some travel-related infections require only supportive care, while others require a more thoughtful approach to treatment. Following is a discussion of further specifics regarding treatment with various infectious processes.
Special Populations
Certain populations may be at a higher risk for developing severe infections. These include infants (< 3 months of age), unvaccinated or incompletely immunized children, and children with underlying chronic health conditions (diabetes, congenital heart issues, etc.). Additionally, those with immune disorders, both acquired (such as post-transplant patients and those undergoing chemotherapy) and congenital (functional asplenia, etc.), should be evaluated more thoroughly. Consultation with the patient’s subspecialists in coordination with infectious disease consultations should be strongly considered. Discussion with obstetrics should be sought in pregnant patients presenting with infectious symptoms following travel outside the country.
Major Disease Processes
Table 3 (available online at https://bit.ly/3kiOfBR) summarizes the typical symptoms, historical clues, and treatment options for four major disease processes travelers may face.
Malaria
Malaria is not only preventable, but unless caught early, it can have significant mortality implications for those infected. According to GeoSentinel, between 1996 and 2011, 3,655 cases, or 4% of those involving fever in a returned traveler, involved potentially life-threatening tropical diseases, for which falciparum malaria accounted for 77%. It still remains the main cause of hospitalization and death for returning travelers.3 Although the number of malaria cases and deaths is on a decline worldwide, the majority of deaths from malaria continue to occur in children.6 Malaria should be actively ruled out in all travelers to endemic areas regardless of medical prophylaxis. Malaria is caused by a protozoan parasite transmitted through mosquito vectors. There are five major subtypes, all with varying geographic distributions and degrees of severity.
Five major species of malaria are known to cause infection in humans: Plasmodium falciparum (highest fatality rate), Plasmodiumm vivax, Plasmodium ovale, Plasmodium knowlesi (primarily simian, but has been known to cause human transition and can be fatal), and Plasmodium malariae. P. falciparum is the dominant species in sub-Saharan Africa and the island of Hispaniola, with P. malariae being less common in the same regions. P. vivax and P. falciparum coexist in the Indian subcontinent, Central and South America, Mexico, Southeast Asia, and Oceania. P. ovale occurs mainly in Africa, and P. knowlesi is found only in Southeast Asia.6 Of these five subtypes, P. falciparum is known to cause seizures, coma, renal failure, pulmonary edema, and even death if not identified and treated early. Although most transmission is through the Anopheles mosquito, instances of bloodborne and congenital transmission have occurred.
Malaria is unusual because symptoms can present more than two weeks after initial exposure. According to the WHO, “it is important that the possibility of falciparum malaria is considered in all cases of unexplained fever starting at any time between seven days after the first possible exposure to malaria and three months after the last possible exposure.” Initial symptoms may include fever, chills, headache, muscular aching and weakness, vomiting, cough, diarrhea, and abdominal pain. Children may appear pale or jaundiced with accompanying hepatosplenomegaly. Rash and lymphadenopathy are uncommon.6 As mentioned earlier, if falciparum malaria is suspected, symptoms can progress to include acute renal failure, pulmonary edema, seizures, shock, followed by coma and death. Cerebral malaria tends to present with altered levels of consciousness with or without multiple, prolonged seizures.
Symptoms of severe malaria include altered mental status, shock, acidosis, hypoglycemia, anemia, or evidence of end-organ dysfunction — and can accompany any of the subtypes of Plasmodium spp. Severe anemia is most likely to develop in children younger than 2 years of age, while cerebral malaria is more likely to occur in older children, with an mean age of 3.5 years.6
Microscopy, through identification of trophozoites on thin and thick peripheral blood smears, is the most common method for diagnosis. Treatment for malaria should not be initiated until the diagnosis has been confirmed, unless there are signs and symptoms of severe malaria. Additionally, malaria has become increasingly difficult to treat because of rising parasitic resistance.
Severe malaria treatment of presumed falciparum malaria should begin with parenteral artesunate. As of May 2020, intravenous artesunate is now available without Centers for Disease Control and Prevention (CDC) consultation for treatment of severe malaria. Other options for treatment include intravenous quinidine gluconate in addition to either clindamycin or doxycycline. Patients taking quinidine need to be monitored on telemetry to watch for ventricular arrhythmias and QT prolongation. Exchange transfusion is no longer thought to be beneficial in patients with severe malaria.7
Options for treatment of milder falciparum or knowlesi malaria depend on the region of travel. Central America west of the Panama Canal, Haiti, the Dominican Republic, and most of the Middle East are chloroquine-sensitive areas. However, because of the increasing resistance of falciparum malaria, the CDC now recommends treating all presumed falciparum malaria as “chloroquine-resistant.” The final treatment regimen should be made in consultation with your local infectious diseases specialist. Knowlesi malaria is fully susceptible to chloroquine. In those who can tolerate oral regimens, and who are without severe disease, options include chloroquine or hydroxychloroquine.7
Chloroquine-resistant areas include Southeast Asia, Oceania, South America, Oman, Iran, Saudi Arabia, and Yemen. For those with travel to chloroquine-resistant areas and in those with milder disease, options for treatment include oral artemether/lumefantrine or atavaquone/proguanil. Alternative treatment regimens include various combinations of quinine, doxycycline, tetracycline, and clindamycin.7
Uncomplicated Plasmodium malariae infections can be treated with chloroquine or hydroxychloroquine. In children younger than 5 years of age, mortality as the result of immune complex-mediated nephropathy has been noted in those with chronic P. malariae infections.8
All P. ovale is sensitive to chloroquine, so options for treatment are chloroquine or hydroxychloroquine, followed by primaquine phosphate or tafenoquine. Chloroquine-resistant P. vivax specimens are found in Papua New Guinea and Indonesia, and treatments for travel to these regions include atavaquone/proguanil, artemether/lumefantrine, or combinations of quinine sulfate and doxycycline or tetracycline — the latter to be used in children > 8 years of age — followed by primaquine phosphate or tafenoquine.7
A caveat for treatment with primaquine phosphate or tafenoquine is to ensure that patients do not have glucose-6-phosphate dehydrogenase deficiency, since this medication can cause an acute hemolytic crisis at higher doses. Treatment of infections caused by both P. vivax and P. ovale requires eradication of liver hypnozoites to prevent a relapse of infection, which is the reason primaquine phosphate or tafenoquine is added to these regimens.7
Dengue
Dengue, Zika, and chikungunya all can present with similar symptoms and tend to be found in overlapping regions. All three of these infectious diseases are spread by Aedes spp. mosquitoes. None of these diseases has direct person-to-person transmission, and it is advisable to avoid mosquito-infested areas in the early mornings and late afternoons, when Aedes mosquitoes are most active. All three infections present with fever, arthralgia, headache, and rash. Of these three, dengue can lead to the most severe complications. Dengue is found in South and Southeast Asia, South and Central America, the Caribbean, Africa, and in tropical Asian countries. It is one of the 10 leading infectious causes of death in children ages 1 to 15 years worldwide.9
Although most cases of dengue tend to be mild, there are severe versions of dengue that should be excluded if dengue is suspected. The first and mildest form of dengue is characterized by an acute febrile illness associated with severe muscle, joint, and bone pain. The accompanying rash with dengue fever is a blanching maculopapular or confluent rash over the face, thorax, and flexor surfaces, typically beginning on day 3 of symptoms and persisting for two to three days. It should be noted that petechiae and a positive tourniquet test also are common features of dengue. After defervescence, a generalized morbilliform rash lasting one to five days can appear, with sparing of the palms and soles.9 Retro-orbital pain and gustatory anomalies are other symptoms that can be seen in patients with dengue.
The more extreme forms of dengue include a viral hemorrhagic variant and dengue shock syndrome. Warning signs for these severe variants include persistent vomiting, severe abdominal pain, rising hematocrit, and worsening thrombocytopenia. The hemorrhagic form of dengue is characterized by its hallmark thrombocytopenia and bleeding complications, such as mucosal or gastrointestinal bleeds. Dengue shock syndrome is accompanied by significant hypotension that requires aggressive fluid resuscitation to correct. Findings of increased vascular permeability, such as pleural effusions or ascites, often are noted. Nonsteroidal anti-inflammatory drugs (NSAIDs) should be avoided in the treatment of dengue. In those with severe dengue, volume repletion with intravenous fluid followed by blood products should be considered if there is concern for hemorrhage or hypotension. In those with volume overload, judicious use of diuretics can be considered.
Enteric Fever
Salmonella enterica serotype Typhi is particularly notable because it can lead to typhoid or enteric fever. Enteric fever has a high fatality rate in children younger than 4 years of age, but it most commonly occurs in those between 5 and 12 years of age.10 Typical symptoms include fever, malaise, headache, anorexia, and abdominal symptoms, including abdominal pain, gastrointestinal bleeding, diarrhea, and constipation (which can be more common than diarrhea in older children). Specific countries associated with the highest number of pediatric cases are Mexico, India, the Philippines, Pakistan, El Salvador, and Haiti.10
High fatality from this disease process results from complications such as sepsis, gastrointestinal bleeding, intestinal perforation, and typhoid encephalopathy. These findings usually are present in the second to third week of symptoms. Because this is commonly thought to be a typical viral syndrome, delaying antibiotics is a significant contributor to mortality.11
Notably, enteric fever has two unique findings. The first is bradycardia, even in the setting of fever or dehydration. This is referred to as relative bradycardia, but some studies have suggested this phenomenon may not be seen in the pediatric population.12 The other finding, rose spots, is a dermatologic finding that includes blanching, erythematous, slightly raised lesions on the skin of the trunk. These lesions are noted during the second week of illness and fade after three days.10 Infection occurs after eating raw fruit and vegetables fertilized by human feces. This particular disease process can have devastating sequelae for those with congenital or acquired neutropenia, chronic granulomatous disease, acquired immunodeficiency syndrome, immune system disorders, a history of organ transplantation and prior gastrectomy, as well as in newborns and sickle cell patients.10
Treatment for enteric fever depends on the travel destination and the severity of the disease. Those with severe disease (shock, altered mental status, prolonged fevers, evidence of organ dysfunction, or other indications for hospitalization) should be treated with parenteral antibiotics. If infection was acquired outside of Pakistan, ceftriaxone or cefotaxime should be used. If there has been recent travel to Pakistan, a carbapenem such as meropenem should be the antimicrobial of choice. In those with uncomplicated disease, fluoroquinolones are preferred if the infection is thought to be from Sub-Saharan Africa (fluoroquinolone use in children is acceptable for severe infections, such as enteric fever). Azithromycin is the treatment of choice if the infection was acquired in South Asia. The response to antibiotics may be slow.10
Traveler’s Diarrhea
A common GI symptom that often accompanies returning travelers is diarrhea. It is aptly named traveler's diarrhea when accompanied with a fever, or dysentery when there is bloody or mucoid stool. Although most diarrheal illnesses are likely viral and self-limited, the vast majority of travel-related diarrhea is bacterial in nature.13 Additionally, although treatment for travel-related diarrhea in adults is common, the same cannot be said for children.
Prolonged periods of diarrhea or bloody diarrhea tend to be bacterial, with common culprits being Salmonella spp., Escherichia coli, Shigella spp., and Campylobacter spp. The highest incidence of this subset of diarrheal illnesses occurs in children younger than 5 years of age, especially in infants younger then 1 year of age.10 Diarrhea usually starts between days 4 and 14 after foreign arrival and lasts between one and five days.13 Traveler’s diarrhea should be treated only if patients present with severe diarrhea (more than 10 loose stools per day), bloody stool, or high fever, or if patients require hospitalization as the result of dehydration or other complications. Otherwise, this self-resolves in approximately one week. Immunocompromised patients, such as patients with sickle cell disease, should always be treated.
Because of increasing worldwide antibiotic resistance, the preferred initial agent of choice should be azithromycin. Further antibiotic choices can be guided by sensitivities from stool culture. Usually, there is concern for treating bloody diarrhea in children with antibiotics because of the possibility of enterohemorrhagic E. coli, for which antibiotic treatment has been associated with an increased risk of hemolytic-uremic syndrome. However, enterohemorrhagic E. coli tends to be a less likely culprit of traveler’s diarrhea.
Other Global Infectious Diseases
As mentioned, dengue, chikungunya, and Zika all present with fever, arthralgia, headache, and rash, but in chikungunya, the arthralgia is more pronounced in the hands, wrists, ankles, and feet. The rash with chikungunya occurs in about 40% to 50% of cases. It is described as a generalized maculopapular rash and presents two to five days following the onset of symptoms with accompanying lymphadenopathy. Conjunctival injection, eyelid swelling, and pharyngitis also can be seen. Younger children may present with febrile seizures. Chikungunya was a disease seen originally in South Asia, but it is becoming more common in Southeast Asia, East and Central Sub-Saharan Africa, and the Caribbean. Chikungunya is distinguished from dengue by its abrupt onset of symptoms, early severity, and shorter-duration fever (12 hours vs. 72 hours).14
Zika typically presents with a milder flu-like illness with or without an accompanying rash. Both Zika and chikungunya can cause conjunctivitis and arthritis or arthralgias. However, the arthritis with Zika tends to be milder in comparison to chikungunya’s. Fever is present in less than a third of affected patients, with infections lasting two to seven days.15 Zika symptoms are similar for both adults and children, but children tend to experience a milder disease course.15 Rarely, Zika has been associated with a post-infectious Guillain-Barré syndrome, and recent epidemics have been noted in Latin America, the Caribbean, and the Pacific Islands.
Chikungunya is treated with supportive measures, including fluids, acetaminophen, and NSAIDs. Although there are no specific treatments for dengue and Zika, they differ from chikungunya in that NSAIDs are not recommended as part of routine supportive care because of the risk of thrombocytopenia. Pregnant patients with Zika need to follow up with a maternal-fetal obstetric specialist because of the risk of congenital malformations. Adolescents with Zika also should be counseled on safe-sex practices, since this virus can be sexually transmitted. Precautions for at least two months with partners of infected women and at least six months for partners of infected men are recommended.
Viral hemorrhagic fevers have multiple vectors of transmission, including mosquitoes, ticks, rodents, and bats. Most of these infections have a high fatality rate, some greater than 50%. Symptoms include fever, headache, or myalgia, followed by vomiting/hematemesis, diarrhea/hematochezia/melena, and other hemorrhagic manifestations. Ebola, Marburg, and Lassa fever all are found in Sub-Saharan Africa and are extremely rare.
Hepatitis A virus (HAV) is one of the most common and vaccine-preventable forms of viral hepatitis. Children receive their first dose of hepatitis A vaccine after 12 months of age, with a booster at least six months after the initial dose. Eighty-five percent of travel-related HAV is linked with travel to Mexico, Central America, and South America. In early childhood, infection usually is asymptomatic, whereas infection in adulthood generally is accompanied by symptoms.16 Acute viral hepatitis presents with fever, nausea, and abdominal pain, followed by jaundice a few days after initial symptom onset. Jaundice is rare in children under 6 years of age.16
Interestingly, younger patients may have diarrhea or even upper respiratory tract symptoms, which makes this a challenging diagnosis. Symptoms can last for several weeks, but they usually resolve within two months.16 This virus is spread by fecal-oral transmission and tends to be caused by consuming contaminated food or water.
HAV infection tends to be self-limited and requires supportive care. Post-exposure prophylaxis in children
< 12 months of age is achieved using the HAV immune globulin. In unvaccinated children >12 months, a single dose of the hepatitis A vaccine should suffice for post-exposure prophylaxis.
Once bacterial causes have been excluded, chronic diarrhea (lasting for
> 10 days), especially in the setting of right upper quadrant pain, should prompt the consideration of amebiasis. Weight loss, fatigue, and fever are common associated symptoms. Entamoeba histolytica is the protozoan responsible for liver abscesses and amoebic dysentery.
Although it has a worldwide distribution, it frequently is seen in Asian, Sub-Saharan African, and Central and South American countries, especially those with poor sanitation. If there is concern for a liver abscess, ultrasound is the modality of choice for diagnosis. Children tend to be asymptomatic carriers with lower frequencies of liver abscesses.17 Amoebic dysentery and amoebic liver abscesses should be treated with metronidazole.
Rickettsial infections are a family of infections spread by ticks, lice, and chiggers. All rickettsial infections are characterized by the bite-mark site, which develops into an eschar — a scab-like region at the bite site.
While eschars in adults tend to be located on the trunk, in children, they are seen commonly in moist intertriginous areas, such as the genitalia and perineum.18
Scrub typhus is present in Southeast Asia, China, Japan, India, and Northern Australia and is transmitted by chigger bites. Symptoms include fever, chills, headache, and myalgia. Less common symptoms include hepatomegaly, respiratory distress, and lymphadenopathy.
Tick-bite fever is encountered commonly in southern Africa, especially in patients who are on safari or are trekking. Spotted fevers, including Rocky Mountain spotted fever, also are rickettsial illnesses that present with headache, fever, and a rash that consists of small red spots or blotches.
Q fever is a rare form of a rickettsial infection. It can present with headaches, rigors, fevers lasting five to 10 days, myalgia, upper respiratory symptoms, or findings consistent with atypical pneumonia. Infection occurs through handling mammalian tissues/hides, inhalation of aerosolized particles, or through tick bites. Symptomatic Q fever is rare in children.18
If a rickettsial infection is suspected, treatment should be started immediately without delay for confirmatory testing. Doxycycline is the preferred agent in children of all ages. One notable exception is Q fever, which is generally self-resolving.
In patients presenting with fever and cough, once viral upper respiratory tract infections, influenza, and pneumonia have been excluded, Legionella is an additional consideration. Legionella can present either as a milder flu-like illness (Pontiac fever) or a more aggressive pneumonia-type illness (Legionnaires’ disease). Although it is seen more commonly in immunocompromised children, infection results from inhalation of contaminated water sprays — there is no human-to-human transmission. Legionella has a worldwide distribution. Generally, travelers are at low risk, and infection usually presents as an outbreak from a contaminated water source, such as air conditioning systems or hot tubs.4 Legionnaires’ disease initially presents with chills, abdominal pain, myalgia, headache, and other nonspecific symptoms for a few days before the onset of a high fever, followed by dyspnea, cough, and pleuritic chest pain.19
While Pontiac fever (caused by Legionella) will self-resolve over a two- to seven-day period without antimicrobial therapy, Legionella pneumonia or Legionnaires’ disease will require treatment.19 Macrolides (e.g., azithromycin) are preferred in younger children, although fluoroquinolones (e.g., levofloxacin) can also be considered for older children.
Leptospirosis is characterized by a biphasic illness caused by a spirochete. Similar to legionellosis, it can manifest in either a milder or more symptomatic entity. Initial symptoms can include sudden-onset fever, chills, myalgia and headache, and abdominal pain lasting for four to seven days. Once the spirochetes are cleared from the bloodstream, a secondary phase of infection occurs as the result of an immune complex-mediated reaction. This secondary phase tends to be more severe and can present with meningitis, uveitis, rash, and fever in the milder form of the disease. In Weil’s disease — the more severe form of the disease — jaundice, hemorrhage, renal failure, and myocarditis are possible. The secondary stage of the disease lasts between four and 30 days, and 90% of cases are mild.5 Although it has a worldwide distribution, it commonly occurs in tropical countries. Because infection occurs through contact with skin or mucous membranes and water contaminated by (usually) rat urine, it is advisable to avoid swimming in canals, ponds, rivers, streams, and swamps.4,5,20
For those with milder forms of leptospirosis, doxycycline or azithromycin are preferred oral agents. For those with severe disease (liver or renal issues), intravenous penicillin, doxycycline, ceftriaxone, or cefotaxime should be considered. Certain infectious agents can also present with fever alone or with incredibly vague symptoms. These include, but are not limited to, tuberculosis, malaria, enteric fever, Q fever, and brucellosis. Brucellosis can be caused by exposure to various animals, including cattle, sheep, dogs, pigs, and goats, or by consumption of unpasteurized or raw milk and cheeses. In fact, at the United States-Mexico border, brucellosis occurs eight times more frequently than the national average because of the frequent consumption of unpasteurized goat milk.21
Hallmark symptoms are intermittent fever and malaise, which can last for months before a diagnosis is made because of the nonspecific nature of symptoms. Occasionally, symptoms can be localized, with osteoarticular complications being the most common. Typically, joint involvement is monoarticular, predominantly in the hips, knees, ankles, and sacroiliac joints.21 Brucella is found worldwide but commonly causes disease in developing countries. In children who are younger than 8 years old, treatment for brucellosis consists of trimethoprim-sulfamethoxazole and rifampin for six weeks. In children older than 8 years of age, oral doxycycline plus rifampin are recommended for six weeks.
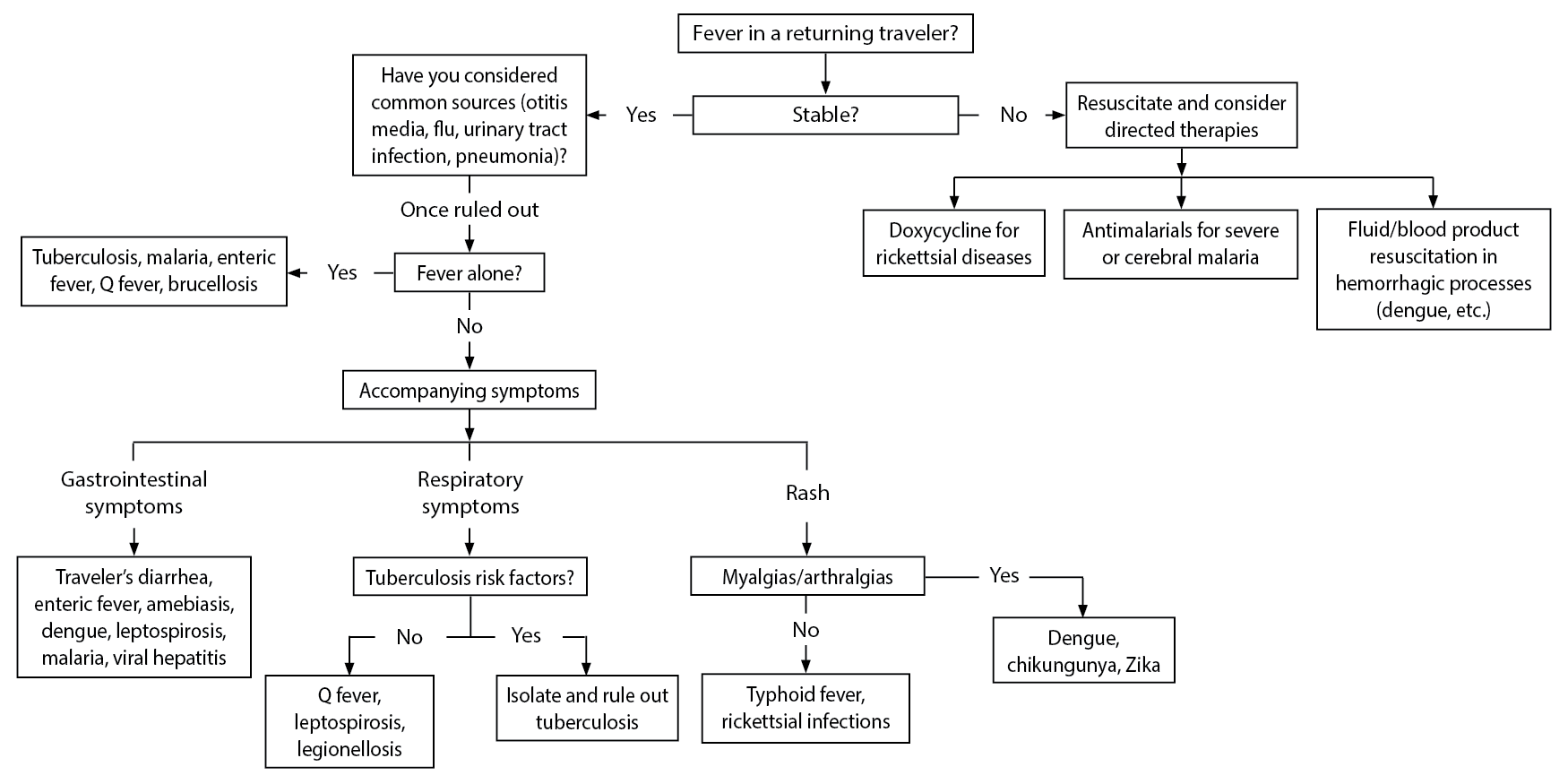
Figure 1 is an algorithm designed to determine which disease a patient may have. Table 4 (available at https://bit.ly/3e8Wqzr) summarizes the diseases mentioned as well as appropriate treatments. Table 5 (available at https://bit.ly/2HHNPYK) gives a summary of likely causes of fever based on geographic region.
(Clicking the image of the algorithm will open a larger version in a new tab.)
Resources for Clinicians
There are many resources that can provide information, for both travelers and clinicians alike, regarding current recommendations and treatment options for returning travelers. For those residing in the United States, the CDC website (http://wwwnc.cdc.gov/travel/) offers destination-specific advice, health advisories, and outbreak notices. The WHO Yellow Book (http://www.who.int/ith/en/) is a resource for clinicians that provides travel health recommendations and specific treatment options for various disease processes in addition to the Red Book.2
References
A complete list of references can be found online at https://bit.ly/3kewBzp.
Although, currently, there are travel restrictions in many countries, this will pass. Acute care physicians need to have an awareness of diseases that are prevalent in other countries to accurately diagnose, manage, and treat patients traveling to and from other parts of the world. The authors present an incredibly valuable synopsis of fever and differential of fever in returning pediatric travelers
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.