AUTHORS
Zahra M. Ghazi-Askar, MD, Clinical Assistant Professor; Director, Pediatric Ultrasound Education; Department of Emergency Medicine, Stanford School of Medicine, Stanford, CA
R. Conner Dixon, MD, Chief Resident Physician, Stanford School of Medicine, Stanford, CA
N. Ewen Wang, MD, Professor of Emergency Medicine, Stanford School of Medicine, Stanford, CA
PEER REVIEWER
Aaron Leetch, MD, FACEP, Associate Professor, Director Pediatric Emergency Medicine Residency, University of Arizona, Tucson
Executive Summary
• Anisotropy is the different ultrasound (US) echogenicity of normal tissue when the angle of the US beam is not perpendicular to the plane of the structure being imaged. Depending on the angle of the probe in relation to the axis of the structure, the structure can appear with a different echogenicity. This technique is helpful for following structures, such as tendons, their entire lengths and can be used to discern discontinuities and other pathologies.
• Higher frequency linear array transducers do not penetrate deep into the tissues, making them ideal for imaging superficial body structures. For most musculoskeletal imaging, an 8- to 14-MHz transducer should be used.
• The stage and the severity of infection determines the appearance of cellulitis on ultrasound. Initially, there is a thickening of the subcutaneous soft tissue, along with a loss of normal morphology. There is a diffuse increase in echogenicity of the skin and adjacent adipose tissue.
• In cellulitis, the increased echogenicity may be seen in other conditions causing soft tissue edema, such as a local allergic reaction. As the infection progresses, the inflamed and hyperechoic fat lobules are separated by fluid.
• On US, both radiolucent and radiopaque materials appear hyperechoic. There is often a surrounding hypoechoic rim, and posterior shadowing or reverberation artifact often are also detected.
Ultrasound is an incredible tool that keeps becoming more valuable. In this article, the authors show how point-of-care ultrasound of the musculoskeletal system can help clinicians identify a diversity of diseases, including soft tissue infections, abscesses, and foreign bodies! In a later issue, the authors explore the use of ultrasound to identify bone and joint issues.
— Ann M. Dietrich, MD, FAAP, FACEP
Introduction
Point-of-care ultrasound (POCUS) has become a staple in the evaluation and treatment of patients in the emergency department (ED). From focused assessment with sonography in trauma to echocardiogram, the use of POCUS to guide diagnostic tests and treatment has been adopted into the emergency physician’s broad purview.
Initially, ED POCUS was limited to the evaluation of trauma and obstetrical diseases. In the past decade, there has been not only rapid development in ultrasound (US) technology, but also evidence of the value of US in the investigation of musculoskeletal disorders in the ED and on the sidelines of sports fields.
This article reviews techniques and imaging appearances of normal musculoskeletal structures and discusses pediatric clinical applications in the evaluation and treatment of patients with common musculoskeletal complaints.
This article also will review normal tissue, starting from the skin, then moving through subcutaneous fat, muscle, tendons, and lymph nodes. Then, normal tissue will be compared to pathology: cellulitis, abscess, muscle and tendon hematoma and rupture, and lymphadenopathy/lymphadenitis.
After reviewing this article, practitioners should be able to use the steps necessary to acquire and optimize a US image; understand the different US appearances of skin, muscles, tendons, and nerves; and identify pathology for diagnostic and interventional purposes.
Indications
US can be used to identify and differentiate tendons, muscles, ligaments, nerves, and vessels with great resolution. These tissues generally are described by their echogenicity: isoechoic, hypoechoic, anechoic,
hyperechoic. Musculoskeletal US also uses the artifact of anisotropy or “the angle dependent appearance of a tissue.” (See Figure 1.)
Figure 1. Insonation of an Achilles Tendon Ultrasound |
 |
|
Long-axis view of a normal Achilles tendon comprised of fibrous connective tissue. Note how the tendon can appear both hyperechoic when the angle of insonation is at 90 degrees, or perpendicular, to the US probe (short arrows) and anechoic when the angle is different than 90 degrees (long arrows) because of anisotropy artifacts. Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Anisotropy is the different US echogenicity of normal tissue when the angle of the US beam is not perpendicular to the plane of the structure being imaged. Depending on the angle of the probe in relation to the axis of the structure, the structure can appear with a different echogenicity. This technique is helpful for following structures, such as tendons, their entire lengths and can be used to discern discontinuities and other pathologies. Anisotropy is more pronounced in tendons and is less pronounced in other soft tissues, including muscles, ligaments, and nerves.
Some structures, such as tendons, appear hyperechoic (white) when the probe is perpendicular to them. But they will look hypoechoic (black) if the angle of insonation (the US beam relative to the tissue or organ of interest) is not at 90 degrees. This property helps identify structures that manifest anisotropy.
Probe Selection
The key to obtaining useful information about most musculoskeletal pathologies is using the highest frequency linear array transducer available. Because higher frequencies do not penetrate deep into the tissues, they are ideal for imaging superficial body structures. For most musculoskeletal imaging, an 8- to 14-MHz transducer should be used. The indicator on the US transducer should be pointing to the right side of the patient in the transverse view and cephalad in the longitudinal view.
Technique
The probe should be positioned initially in the transverse and then in the longitudinal orientation on the area of interest. Copious gel allows better visualization of very superficial structures and eliminates the need for applying excessive pressure during the often-painful indications for musculoskeletal US.
Water Bath Technique
The small field of view, relative compressibility of the soft-tissue structures by the transducer, patient motion, and discomfort from contact of the transducer with the pathology often limit conventional US evaluation with direct contact of the probe over the structure to be examined. A water bath technique can overcome these limitations.
This technique is especially useful in the US imaging of shallow skin ulcers, subcutaneous masses, vascular malformations, osteomyelitis, and foreign bodies. The body part to be evaluated is immersed in a bucket or tray filled with water. The probe head then is held about 1 cm above the body part.
This technique is used most often to study the hands and feet. It does not require US gel, since the water itself is an excellent conductor of US waves. Most US probes are water resistant up to the level of the cord.
The Bladder Technique
If a risk of infection is present, or when the water bath technique cannot be utilized for other reasons, the bladder technique can be used. The bladder technique involves using a small balloon (or glove) filled with water or gel. The balloon is pressed against the area of interest, and the US transducer is pressed against the balloon. The US waves pass through the balloon and will provide the desired image.
Normal Anatomy
US provides excellent visualization and distinction between the different soft tissues because they vary substantially in water content and echogenicity. (See Figure 2.) Skin is the most echogenic tissue, while fat is the least echogenic.
Figure 2. Echogenicity in Ultrasound Images |
 |
|
Ultrasound of the superficial abdomen demonstrating dense, hyperechoic epidermis (short arrows) and relatively hypoechoic subcutaneous fat (long arrows). Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Skin
Sonographically, the epidermis and dermis appear as thin, linear, echogenic stripes. In non-disease states, the two layers are often too thin to be distinguished from each other. (See Figure 2.)
Subcutaneous Fat
Normal subcutaneous tissue appears hypoechoic, with thin and linear echogenic structures separating the fat lobules. The linear structures are parallel to the overlying skin.1 (See Figure 2.)
Muscle
Normal muscle tissue consists of multiple muscle fascicles. These fascicles appear hypoechoic compared to the hyperechoic sheath, called the perimysium, that surrounds the muscle structure.1 (See Figure 3.)
Figure 3. Ultrasound of Muscle Tissue |
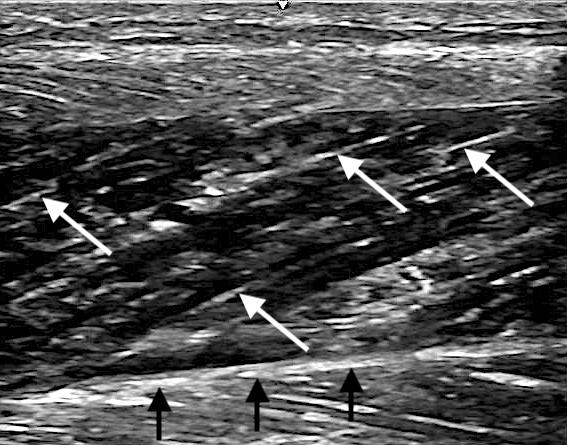 |
|
Long-axis view of forearm muscles with hypoechoic fascicles (white arrows) and hyperechoic perimysium (black arrows). Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Tendons
Tendons manifest an organized, fibrillar orientation on long-axis sonographic views. On the short axis, tendons appear oval-shaped and contain small, dot-like structures. Tendons have no vascularity on color flow imaging. Ligaments have a similar appearance to tendons, except they are more compact.1 (See Figures 4 and 5.)
Figure 4. Ultrasound of an Achilles Tendon |
 |
|
Long-axis view of Achilles tendon (arrows). Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Figure 5. Ultrasound of Patellar Tissues |
 |
|
Longitudinal gray-scale image of part of the patellar “tendon.” Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Nerve
US demonstrates nerves as “honeycomb” or “pepper pot” structures composed of hypoechoic spots embedded in a hyperechoic background. They appear distinctly different from tendons in a transverse/short-axis image. (See Figure 6.)
Figure 6. Ultrasound of Median Nerve |
 |
|
A short-axis view of the median nerve (arrow). Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Fluid
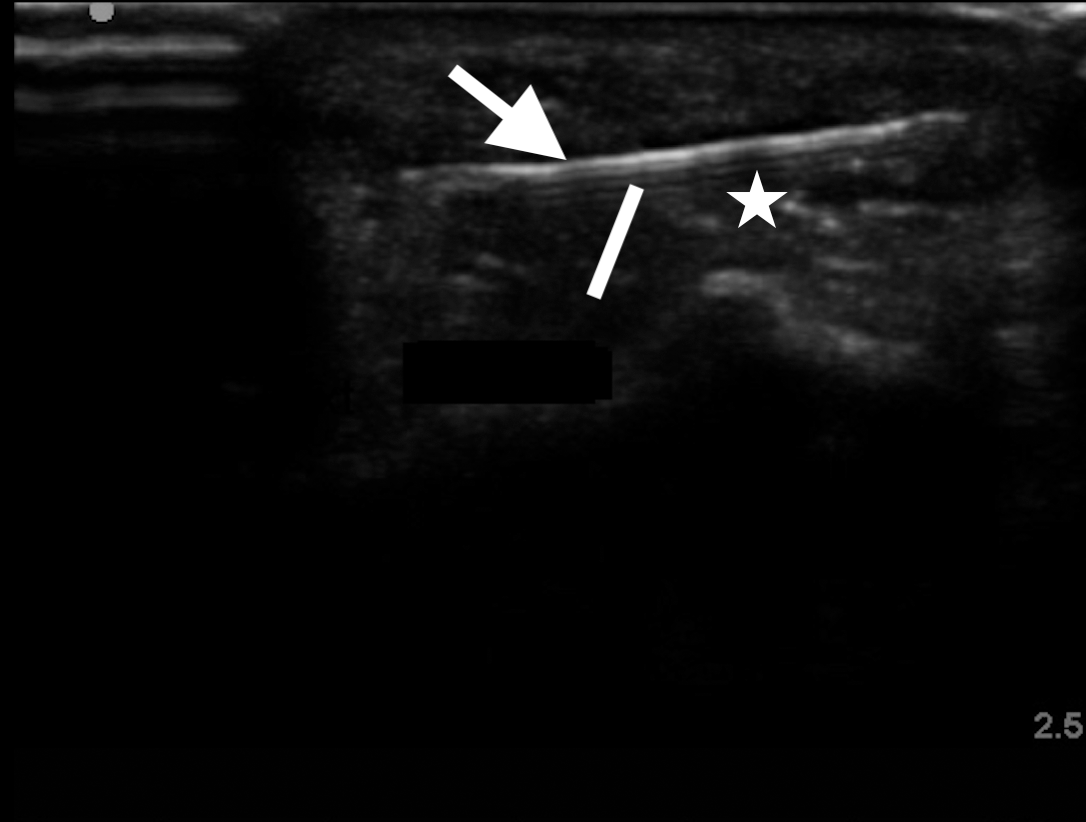
Fluid has an anechoic appearance on US and can be confirmed with dynamic interrogation, as it should respond to pressure. Figure 7 shows the anechoic or black appearance of fluid within the deep infrapatellar bursa of the knee.
Figure 7. Ultrasound of Patellar Ligament |
 |
|
A long-axis view of patellar ligament (short arrows), the patella (long arrow), and the deep infrapatellar bursa (star). Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Lymph Nodes
Normal lymph nodes have an oval shape. The central hilum appears hyperechoic, and the vascularity pattern on color flow imaging is seen on the peripheral aspect of the lymph node.1 (See Figures 8 and 9.)
Figure 8. Ultrasound of a Lymph Node |
 |
|
The echogenic hilum characteristic of a normal lymph node (arrow). These are enlarged lymph nodes that have kept their oval structue, and have an echogenic hilum. Image courtesy of Zahra M. Ghazi-Askar, MD. |
Figure 9. Ultrasound of a Cervical Lymph Node |
 |
|
A cervical lymph node (star) and blood vessel (arrow). Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Sonographic Appearances of Musculoskeletal Pathology
Cellulitis
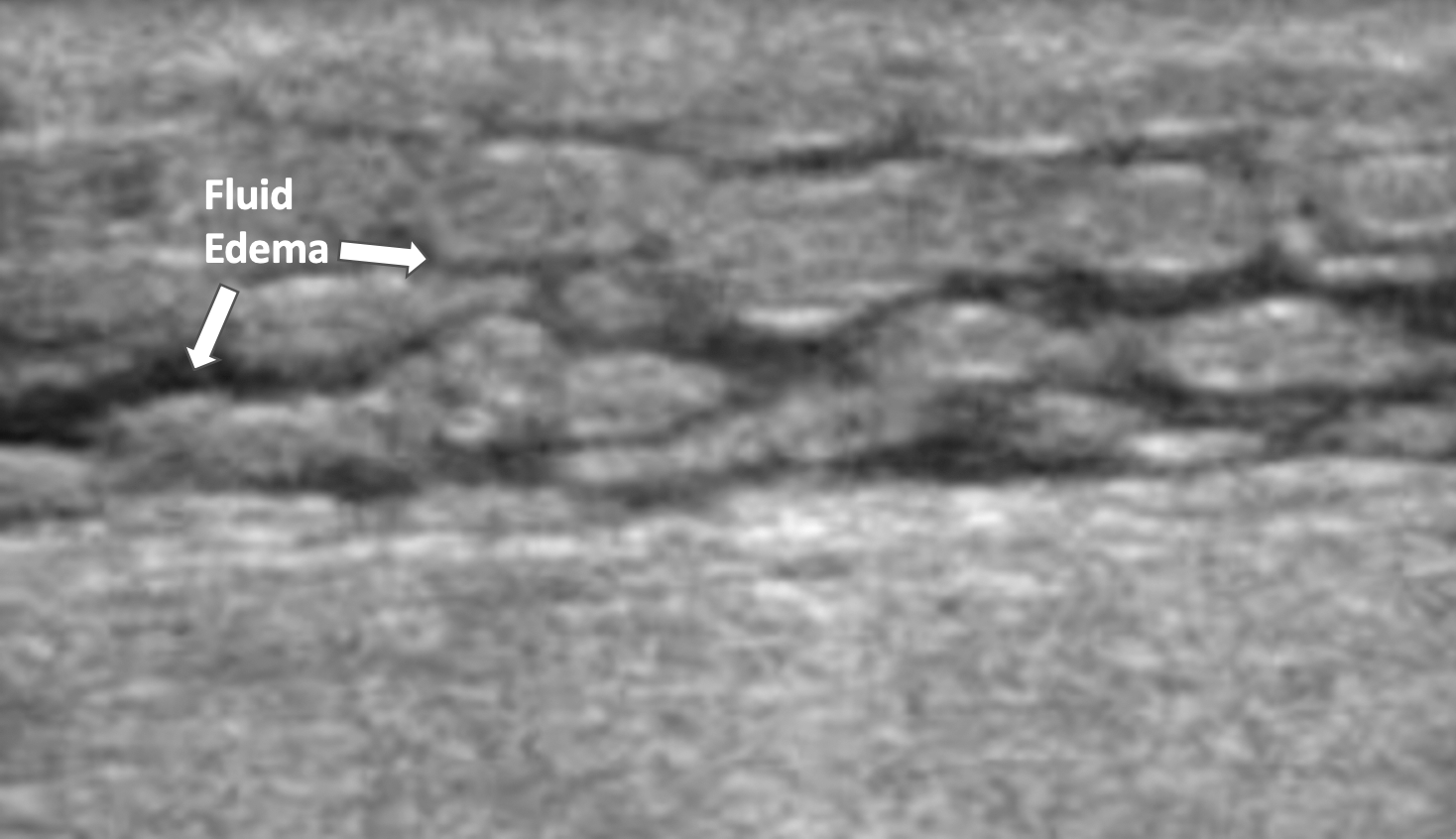
The stage and the severity of infection determines the appearance of cellulitis on ultrasound. Initially, there is a thickening of the subcutaneous soft tissue, along with a loss of normal morphology. There is a diffuse increase in echogenicity of the skin and adjacent adipose tissue. (See Figure 10.). Within the first few days of infection, there is a loss of the lines that separate the fat lobules.1.2
Figure 10. Ultrasound of Cellulitis |
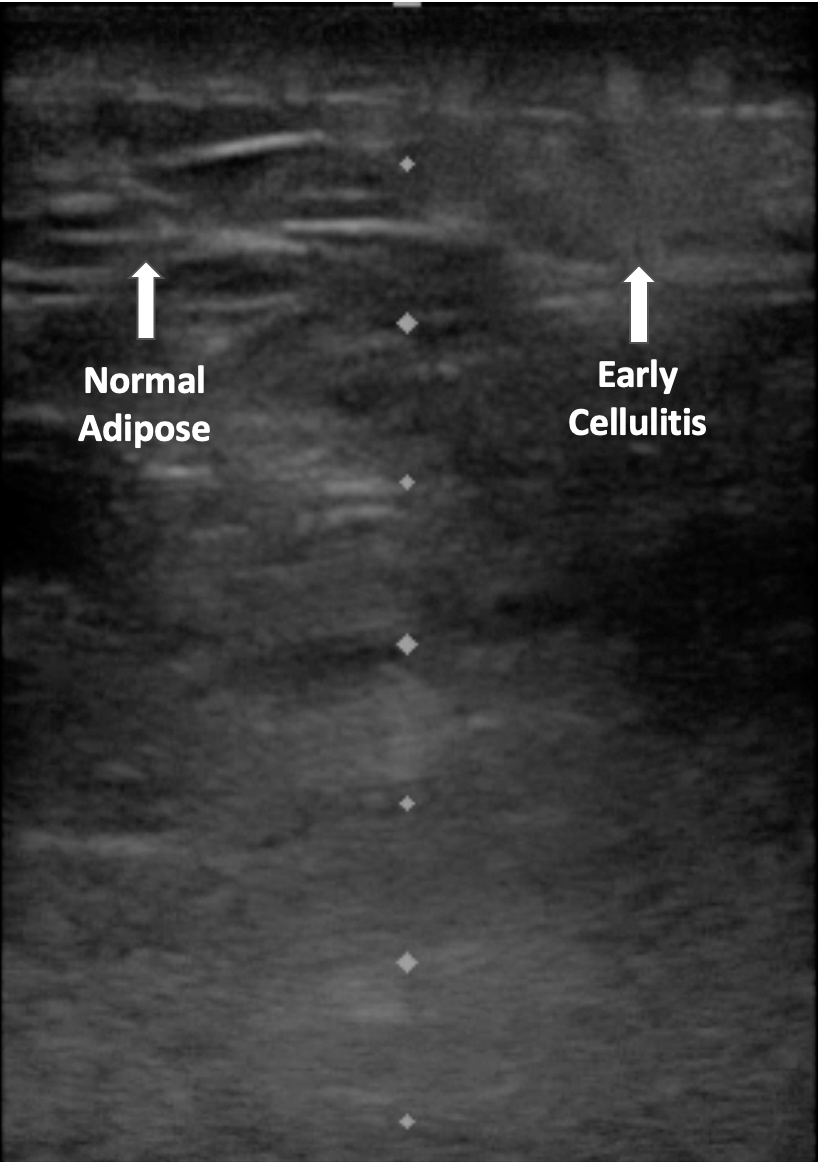 |
|
There is diffuse increase in echogenicity of the subcutaneous adipose tissue. The fat lobules are no longer distinct. Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
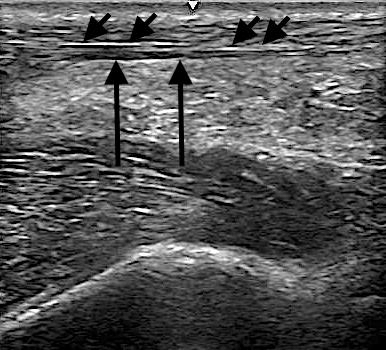
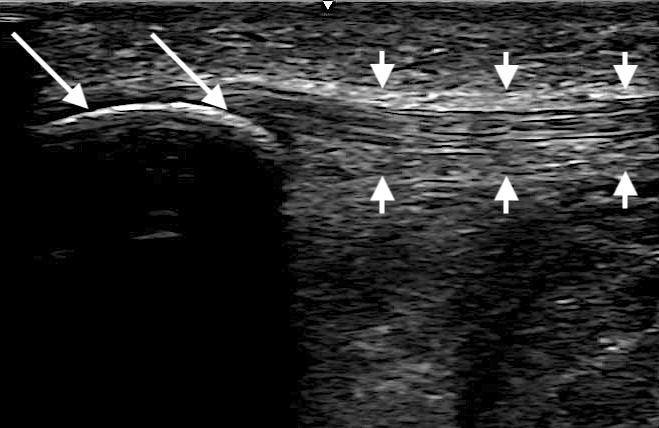
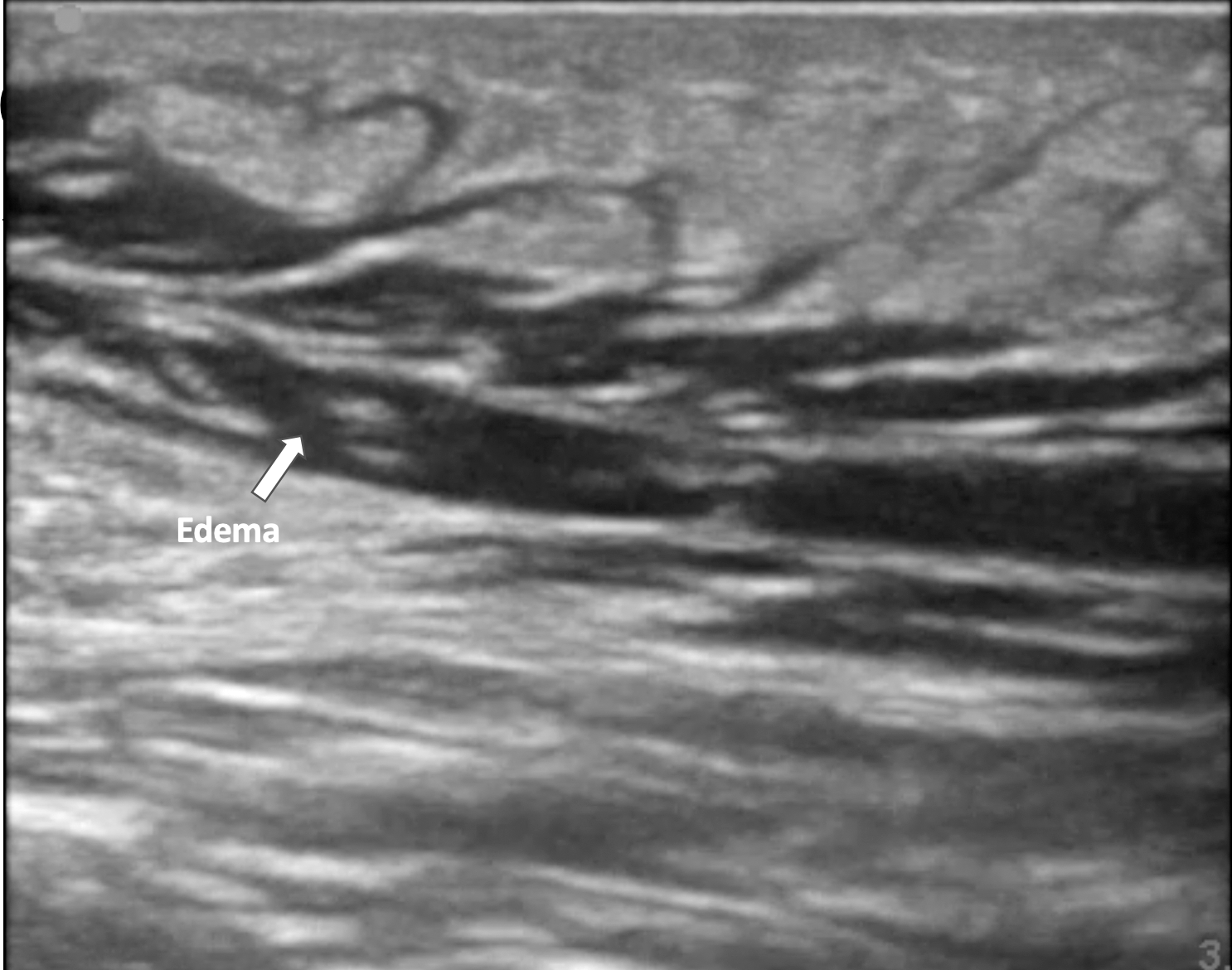
The increased echogenicity may be seen in other conditions causing soft tissue edema, such as a local allergic reaction. As the infection progresses, the inflamed and hyperechoic fat lobules are separated by fluid.2 The increasing edema and fluid accumulation between the fat labules manifest as hypoechoic or anechoic areas. The appearance of hyperechoic fat lobules separated by hypoechoic/anechoic fluid is called cobblestoning.1 (See Figures 11 and 12.)
Figure 11. Cobblestoning on Ultrasound |
|
|
|
Grayscale image demonstrating superficial cellulitis with inflammatory edema separating layers of the subcutaneous tissue (cobblestoning). Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
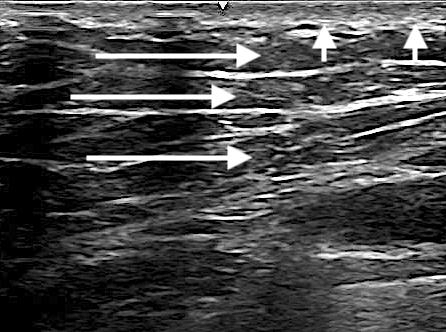
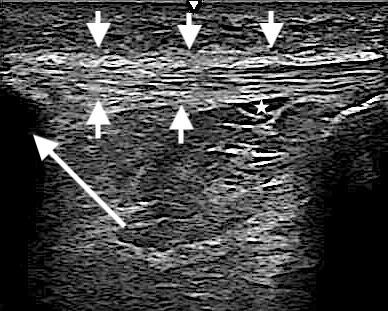
Figure 12. Severe Cellulitis on Ultrasound |
 |
|
Extensive cellulitis with a cobblestone appearance over the healthy underlying muscle tissue. Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Abscess
An abcess appears as a demarcated hypoechoic fluid collection on US. Heterogenous components, debris, and septations may be visualized in some cases.1,3 (See Figures 12, 13, and 14.)
Figure 13. Abscess with Debris |
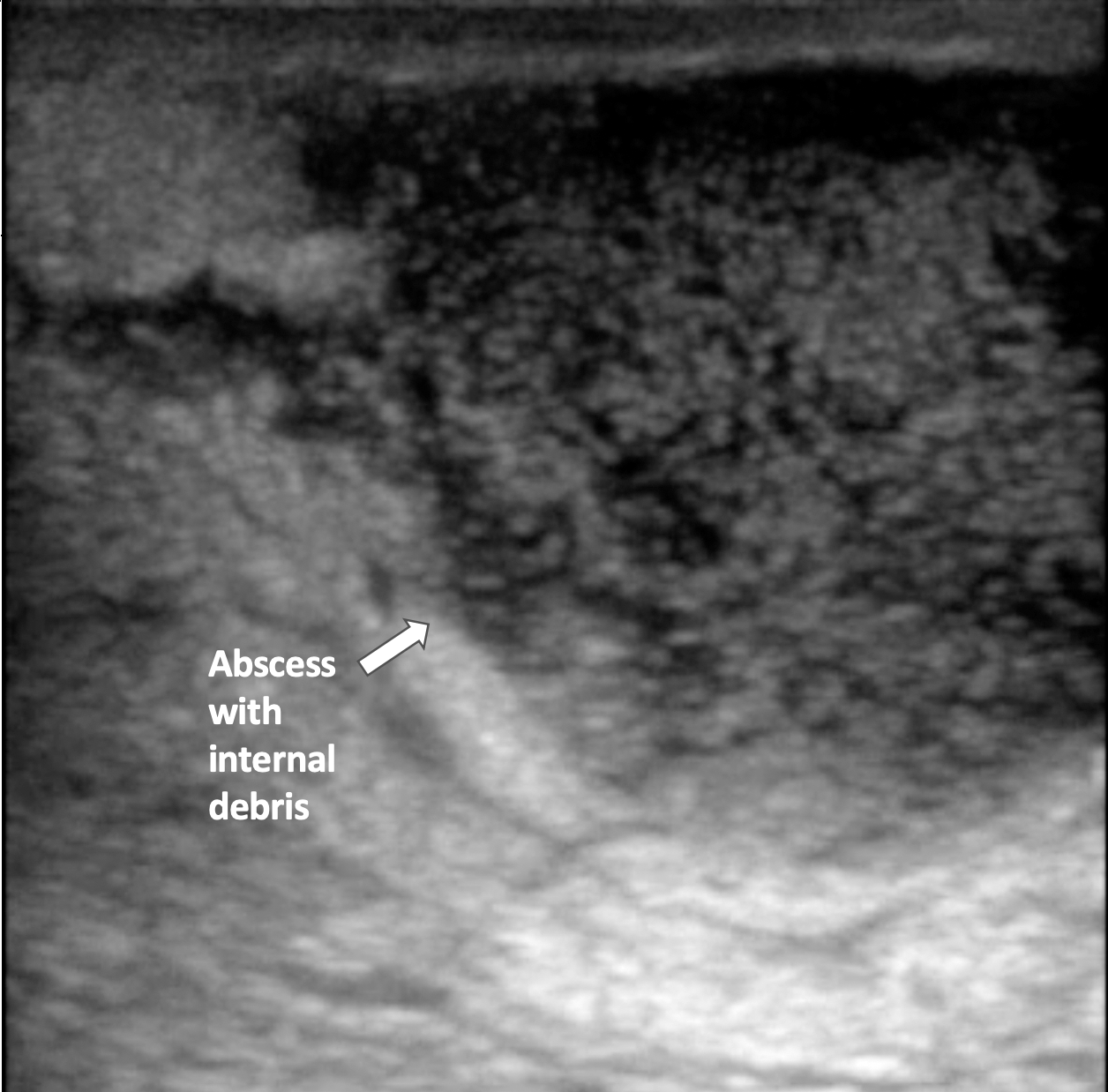 |
|
Moderately circumscribed abscess demonstrated by a collection of hypoechoic fluid with internal debris and air scattering. Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Figure 14. Abscess in Subcutaneous Fat |
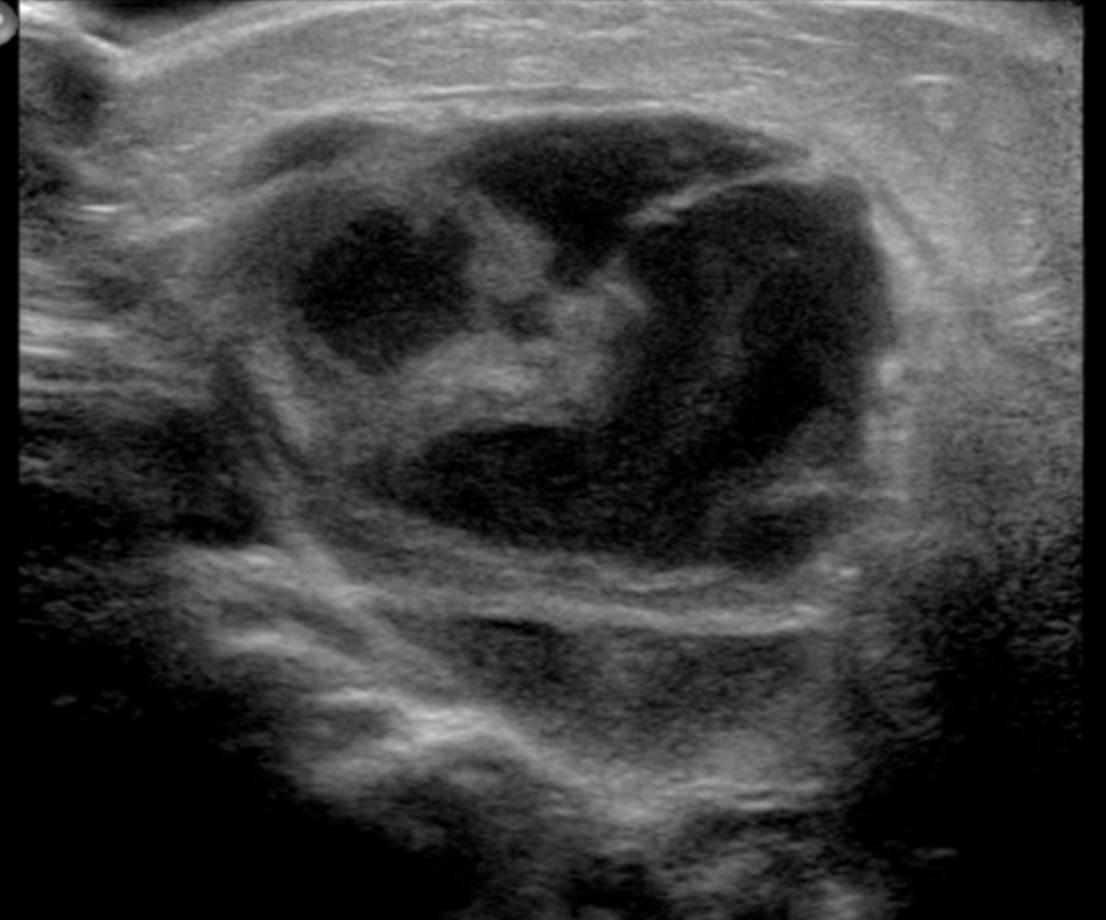 |
|
An abscess seen as a hypoechoic lesion with scattered debris. Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Abscesses often demonstrate posterior acoustic enhancement on US. Gentle, repetitive pressure placed over the abscess with the ultrasound probe produces a circular and swirling motion of the abscess contents. This is oftened lightheartedly referred to as “pustalsis” in the ultrasound world.1
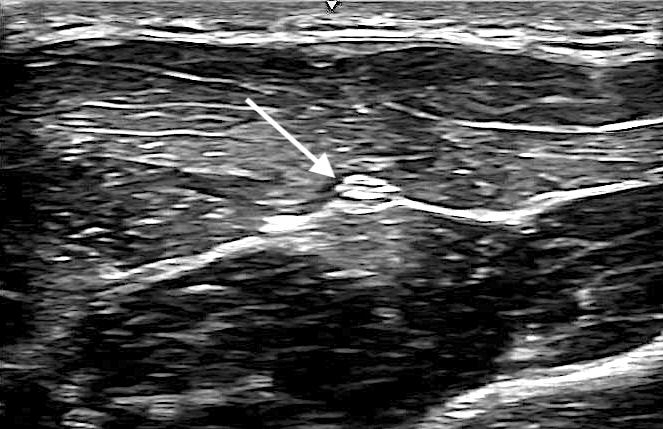
Soft Tissue Foreign Bodies
US is useful in identifying non-radiopaque foreign bodies that are not readily visualized on conventional radiographs. Examples of non-radiopaque foreign bodies include wood, plant thorns, and certain glass material. On US, both radiolucent and radiopaque materials appear hyperechoic. (See Figure 15.) There is often a surrounding hypoechoic rim, and posterior shadowing or reverberation artifact often are also detected.1
Figure 15. Ultrasound of a Foreign Body |
 |
|
The hyperechoic appearance of a wooden tooth pick (arrow). Note the reverberation (line) and the posterior shadow (star). Image courtesy of Zahra M. Ghazi-Askar, MD. |
When looking smaller (< 3 mm) foreign bodies that may not be readily visible, look for the artifacts mentioned in association with surrounding hyperemia with color Doppler imaging and loss of tissue structure. Gas in soft tissues often produces shadowing and reverberation artifacts, which may make detection of foreign bodies challenging on ultrasound.1,4,5
Tendon Injuries
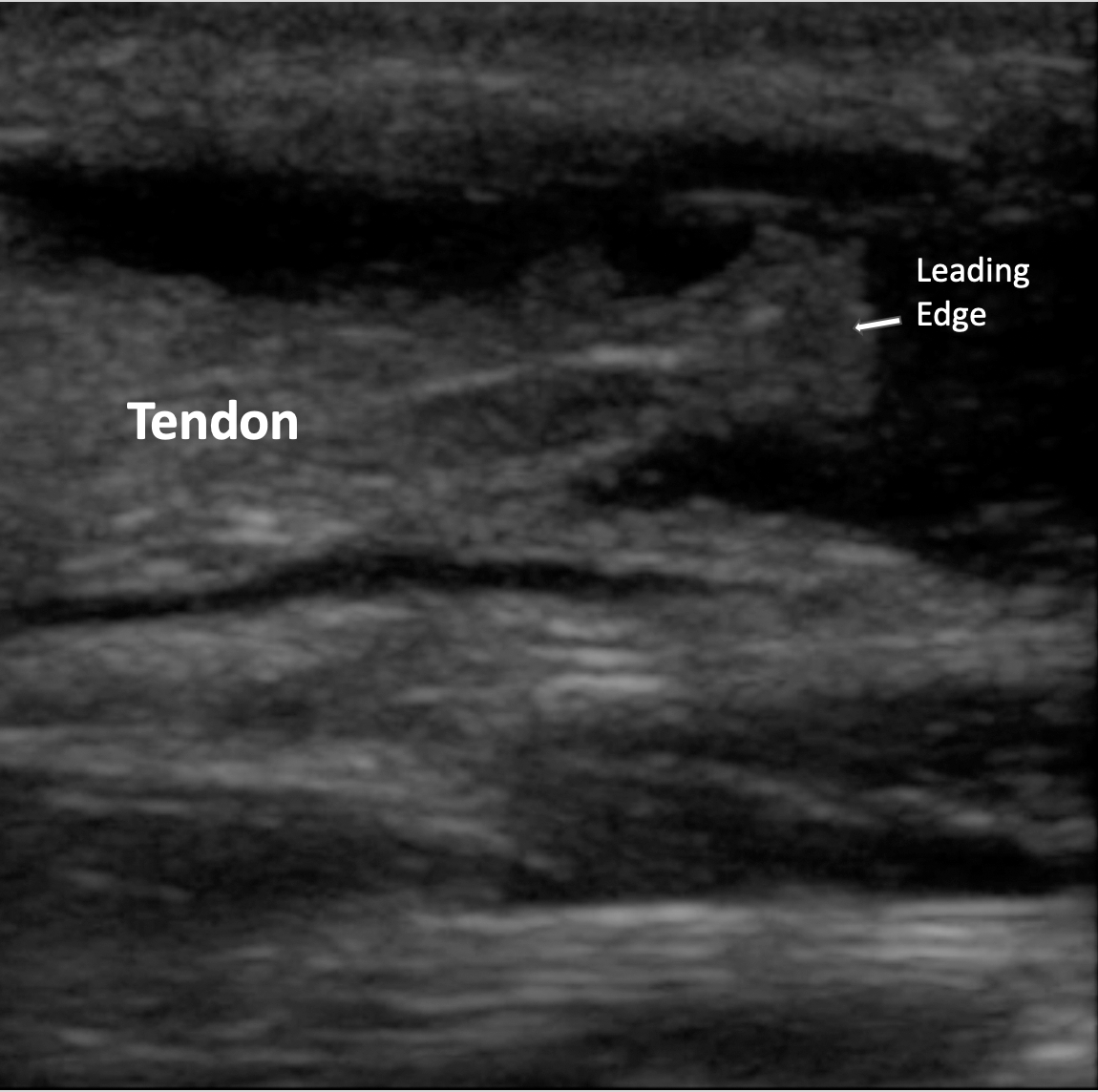
Tendons manifest with an organized, fibrillar orientation on long-axis views on sonography. Dynamic US imaging readily identifies an injured tendon as an area of hypoechoic defect within the organized structure of the tendon. In the case of a ruptured tendon, the torn end of the tendon may be retracted proximal to the site of insertion.6 (See Figure 16.) As an adjunct to a physical examination, POCUS serves as a useful tool for patients presenting to the ED with musculoskeletal complaints.1
Figure 16. Ultrasound of an Achilles Tendon Rupture |
 |
|
Long-axis image of an Achilles tendon rupture . The torn tendon is retracted, denoted by a wavy appearance. Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
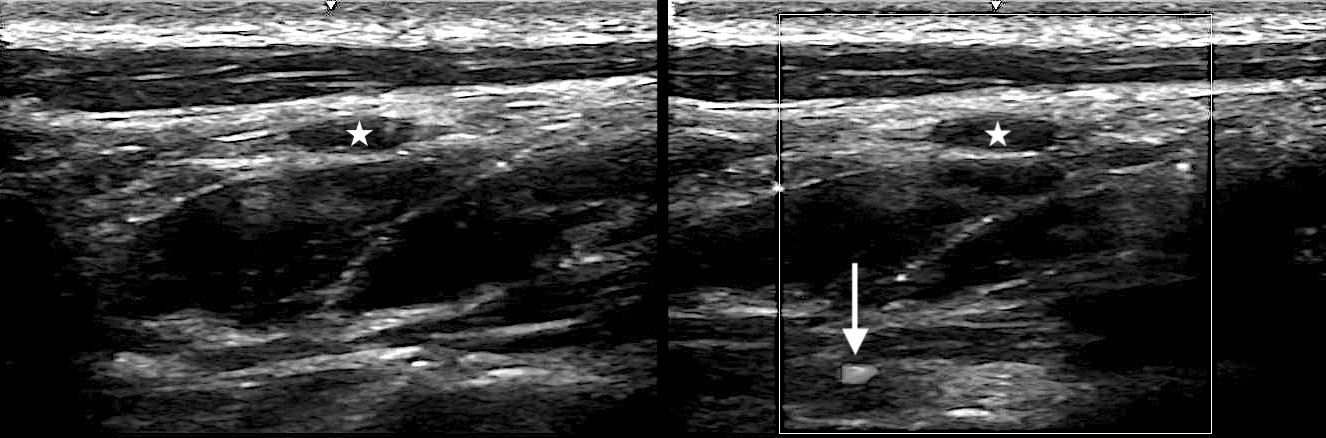
Lymphadenitis
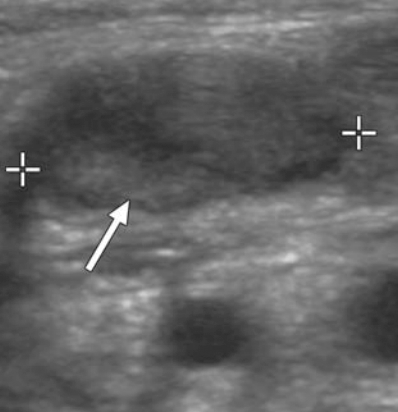
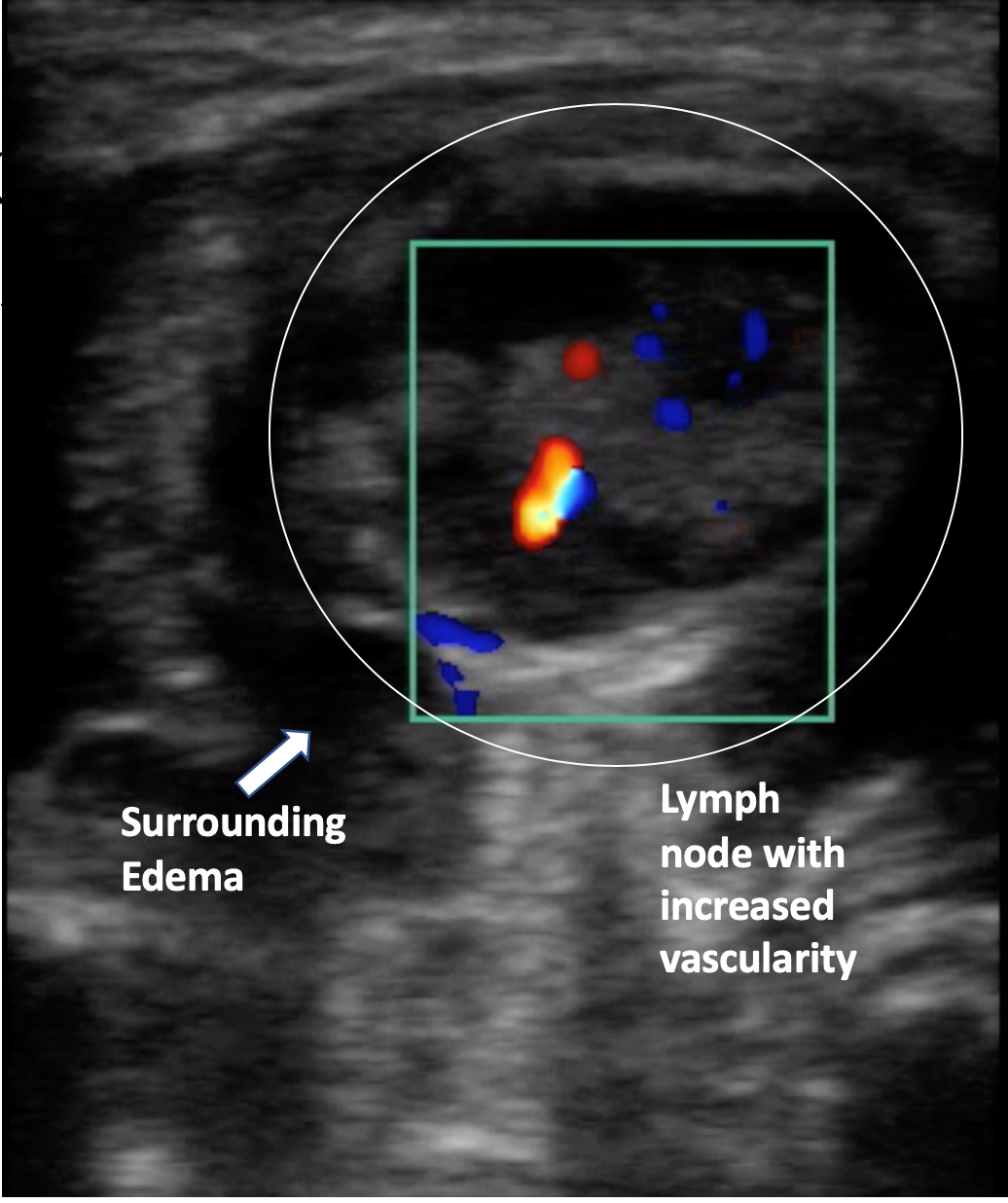
The sonographic appearances of normal lymph nodes differ from those of abnormal nodes. Sonographic features that help to identify abnormal nodes include shape (round), absent hilus, intranodal necrosis, reticulation, calcification, matting, soft-tissue edema, and peripheral vascularity (rather than the central vascularity of a normal node).
Inflamed lymph nodes in reactive lymphadenopathy, while larger in size, maintain their shape and architecture. The length of the lymph node does not exceed 1 cm.7 As the inflammatory reaction progresses or infection sets in, the structural integrity of the lymph node is lost, the hilum becomes more hypoechoic, and the vascularity and hyperemia is seen throughout the structure.1 (See Figures 17 and 18.)
Figure 17. Lymph Node on Ultrasound |
 |
|
Grayscale ultrasound showing increased cortical echogenicity (arrow) and a lack of echogenic hilum consistent with a reactive lymph node. Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Figure 18. Infected Lymph Node |
 |
|
Grayscale and color-flow ultrasound images of an infected lymph node with a developing central abscess. The shape is no longer maintained. The size is increased and the hilum appears hypoechoic. Image courtesy of Zahra M. Ghazi-Askar, MD; Vinson Vong, MD; and R. Conner Dixon, MD. |
Conclusion
The superficial location and ease of access to the structures of the musculoskeletal system, in combination with the quick, focused, portable, real-time, and dynamic quality of US exams, makes POCUS a practical tool for providing limited, focused studies to answer specific questions in the busy ED setting. Learning to identify pathology in musculoskeletal structures is simple when the comparison to the contralateral normal side is available on patients. Caution must be exercised to understand the limitations of musculoskeletal US and set realistic expectations to keep diagnostic errors to a minimum.
REFERENCES
- Connell MJ, Wu TS. Bedside musculoskeletal ultrasonography. Crit Care Clin 2014;30:243-273.
- Gottlieb M, Avila J, Chottiner M, Peksa GD. Point-of-care ultrasonography for the diagnosis of skin and soft tissue abscesses: A systematic review and meta-analysis. Ann Emerg Med 2020;76:67-77.
- Marin JR, Dean AJ, Bilker WB, et al. Emergency ultrasound-assisted examination of skin and soft tissue infections in the pediatric emergency department. Acad Emerg Med 2013;20:545-553.
- Mohammadi A, Ghasemi-Rad M, Khodabakhsh M. Non-opaque soft tissue foreign body sonographic findings. BMC Med Imaging 2011;11:9.
- Varshney T, Kwan C, Fischer JW, Abo A. Emergency point-of-care ultrasound diagnosis of retained soft tissue foreign bodies in the pediatric emergency department. Pediatr Emerg Care 2017;33:434-436.
- Simard R. Ultrasound imaging of orthopedic injuries. Emerg Med Clin North Am 2020;38:243-265.
- Friedman N, Tseng F, Savic R, et al. Reliability of neck mass point-of-care ultrasound by pediatric emergency physicians. J Ultrasound Med 2019;38:2893-2900.
Ultrasound is an incredible tool that keeps becoming more valuable. In this article, the authors show how point-of-care ultrasound of the musculoskeletal system can help clinicians identify a diversity of diseases, including soft tissue infections, abscesses, and foreign bodies! In a later issue, the authors explore the use of ultrasound to identify bone and joint issues.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.