Pediatric Sports-Related Injuries of the Lower Extremity: Ankle
October 1, 2016
Related Articles
-
Infectious Disease Updates
-
Noninferiority of Seven vs. 14 Days of Antibiotic Therapy for Bloodstream Infections
-
Parvovirus and Increasing Danger in Pregnancy and Sickle Cell Disease
-
Oseltamivir for Adults Hospitalized with Influenza: Earlier Is Better
-
Usefulness of Pyuria to Diagnose UTI in Children
AUTHORS
Kristina Colbenson, MD, Board Certified Emergency Medicine and Sports Physician, Mayo Clinic, Rochester, MN
Erika Hoenke McMahon, MD, Resident Physician, Mayo Clinic, Rochester, MN
PEER REVIEWER
Christopher J. Haines, DO, FAAP, FACEP, Chief Medical Officer, Children’s Specialized Hospital, New Brunswick, NJ; Associate Professor of Pediatrics and Emergency Medicine, Drexel University College of Medicine, Attending Physician, St. Christopher’s Hospital for Children, Philadelphia, PA
To reveal any potential bias in this publication, and in accordance with Accreditation Council for Continuing Medical Education guidelines, we disclose that Dr. Dietrich (editor), Dr. Skrainka (CME question reviewer), Ms. Wurster (nurse planner), Dr. Colbenson (author), Dr. McMahon (author), Dr. Haines (peer reviewer), Ms. Coplin (executive editor), and Ms. Mark (executive editor) report no relationships with companies related to the field of study covered by this CME activity.
EXECUTIVE SUMMARY
- The most common ankle injury seen in the emergency department and one of the most common sports-related injuries is a lateral ankle sprain, or inversion injury, accounting for more than 85% of all ankle sprains, with syndesmotic ankle sprains and medial sprains occurring much less frequently.
- Typically, patients with lateral ankle sprains present with pain, swelling, and inability to bear weight. On exam, patients have pain over the anterior talofibular and calcaneofibular ligaments; If pain is not present in these areas, the provider should be suspicious of a potentially more serious ankle injury.
- To aid in the diagnosis of a syndesmotic ankle injury, the provocative squeeze test can be performed, compressing the tibia and fibula together midway up the leg, with a positive test being pain at the distal tibiofibular joint.
- The Ottawa Ankle Rules are a reliable tool to exclude fractures in children older than 5 years of age who present to the emergency department with ankle and midfoot injuries. Imaging of the ankle is only necessary if there is pain in the malleolar zone plus one of the following: bony tenderness along the distal 6 cm of the posterior edge of the medial or lateral malleolus or inability to bear weight for four steps immediately after the injury and in the emergency department.
- For midfoot imaging, the rules recommend imaging only with pain in the midfoot region plus one of the following: bony tenderness at the navicular bone or the base of the fifth metatarsal or inability to bear weight for four steps immediately after the injury and in the emergency department
- Even if the patient’s exam is consistent with an ankle sprain, and per clinical decision tools there is no indication for imaging, it is still important to push on six spots to guarantee to not miss a high-morbidity injury. These six spots are: 1) the proximal fibula to rule out Maisonneuve fracture; 2) talus to rule out a talar neck, dome, or lateral process fracture; 3) navicular bone to rule out navicular fracture; 4) base of the fifth metatarsal to rule out a Jones or pseudo-Jones fracture; 5) base of the first and second metatarsal to rule out a Lisfranc injury; 6) and the tibial and fibular physis to assess for Salter-Harris fracture.
Pediatric lower extremity injuries are common in the emergency department, especially with increasing sports specialization in young athletes. Acute care providers need to be familiar with common injury patterns, indications for radiographs, and more specialized imaging. Recognizing and maintaining a high degree of suspicion for high-morbidity injuries that may masquerade as an ankle sprain is critical. The authors review common injuries and also injuries that cannot be missed including Maisonneuve fracture, talar fractures, navicular fractures, Jones or pseudo-Jones fractures, Lisfranc injuries, and Salter-Harris fractures.
— Ann Dietrich, MD, FAAP, FACEP, Editor
Epidemiology
Millions of children between the ages of 6-18 years participate in organized sports each year.1 Athletic participation yields many health and wellness benefits for children, but with increased sport specialization comes an increased risk of traumatic and overuse injuries.2 Pediatric sports injuries are estimated to make up more than 2 million emergency department visits every year,3 with an incidence rate of up to 35 per 100 children annually.4 In the adolescent population, sports are the leading cause of injury, accounting for more than 30% of adolescent injuries worldwide.5 Of these injuries, 60% or more involve the lower extremity,5,6 and a high proportion of these involve the ankle. This article will emphasize how to perform a focused physical exam to empower emergency medicine physicians to accurately diagnose and manage commonly encountered and commonly missed foot and ankle injuries in the emergency department.
Pathophysiology
Pediatric patients are at higher risk for sports-related injuries because of immature skeletal growth.2 Especially at risk is the physis, the cartilaginous growth plate of long bones that accounts for longitudinal growth. Injuries that cause benign strains and sprains in adults can result in serious growth plate injuries in children, as ligaments are structurally stronger than the physis until it is closed. Gradual closure of the physis occurs with puberty, and prior to closure, the physis is at particular risk for injury.7-10 Because of overuse secondary to sport specialization, subacute stress fractures and apophysitis are becoming increasingly common indications for presentation to the emergency department. An apophysis is a location where muscle tendon inserts into a secondary ossification center. Pediatric athletes are particularly vulnerable to overuse injuries because their bones are weaker than those of adults and because they still have open growth plates.10,11
Ankle Sprains — General, Epidemiology, Etiology
Of the many lower extremity injuries sustained every year by pediatric athletes, a high proportion of these are ankle injuries. In the general population, ankle sprains alone account for as many as 10% of emergency department visits8 and as many as 15-20% of all sports injuries.12 Serious ankle sprains are uncommon in the skeletally immature athlete.13 This is because the ligaments of the ankle insert on the epiphyses distal to the physeal line, placing pediatric athletes at high risk for physeal fracture with injuries that would cause a sprain in adults. The physis often gives way when significant force is applied to the ankle, as it is the weakest link in the bone-tendon-bone interface.10,13 Because some more serious injuries can mimic ankle sprains, it is important for emergency providers to recognize the normal pattern of injury in ankle sprains. This will allow the provider to identify when injury patterns deviate from the norm, thereby differentiating between a benign ankle sprain and more serious injuries that can mimic sprains. These injuries will be discussed later in the article.
Types of Sprains
The most common ankle injury seen in the emergency department and one of the most common sports-related injuries is a lateral ankle sprain, or inversion injury.14 These account for more than 85% of all ankle sprains, with syndesmotic ankle sprains and medial sprains occurring much less frequently.15 Lateral ankle sprains occur when the ankle is in a plantar flexed position and pathologically inverts and adducts, causing injury to the anterior talofibular (ATF) and calcaneofibular (CFL) ligaments,12 which are shown in Figure 1.
Figure 1. Basic Ankle Anatomy |
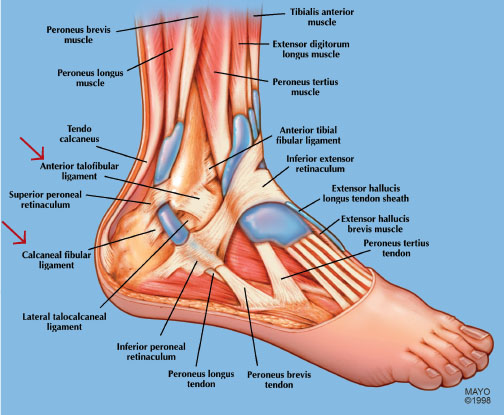 |
|
SOURCE: Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved. |
Typically, patients with lateral ankle sprains present with pain, swelling, and inability to bear weight. On exam, patients have pain over the ATF (more anterior and superior than many providers realize) ligament and pain over the CFL ligament just distal to the distal fibula. If pain is not present in these areas, the provider should suspect a potentially more serious ankle injury.
Medial ankle sprains, caused by an eversion injury when the foot is in a slight dorsiflexed position, are less common than lateral ankle sprains. This injury pattern results in injury to the deltoid ligaments on the medial aspect of the ankle. The deltoid ligaments are a primary stabilizer in the axial loaded ankle and have a superficial and deep component. On exam, patients have pain directly over the deltoid ligaments and medial ankle pain with passive eversion.
Syndesmotic ankle sprains, also known as high ankle sprains, may occur in the adolescent athlete and rarely in the pediatric athlete. These injuries are more common in collision sports such as football, wrestling, and hockey16 and have been estimated to account for 11-17% of ankle sprains in athletes.13,17 Syndesmotic sprains involve injury to the complex of connective tissues providing stability to the mortise of the ankle joint. Structures of this complex include the tibia, fibula, interosseous membrane, and four ligaments: the anterior inferior tibiofibular ligament, the posterior inferior tibiofibular ligament, the interosseous ligament, and the transverse tibiofibular ligament.16 A significant force or load usually is required to cause a syndesmotic injury, and the most common mechanism is forceful external rotation of the foot and ankle. On exam, patients will exhibit point tenderness over the anterior or posterior inferior tibiofibular ligaments, which may extend up the leg if the interosseous membrane is involved. Tenderness also may be found over the deltoid or lateral ankle ligaments, as these structures often are injured simultaneously in a syndesmotic ankle injury. The provocative squeeze test can be performed to aid in diagnosis. The squeeze test is performed by compressing the tibia and fibula together midway up the leg causing shear strain to the distal syndesmosis ligaments. A positive test is pain at the distal tibiofibular joint.18,19
Grading of Ankle Sprains
Ankle ligament sprains classically are graded on a scale of I to III based on the degree of disability, swelling, and ligamentous injury (determined by the amount of ligamentous laxity). Grade I is the mildest, and involves stretching of the ligaments without rupture or joint instability. Grade II is moderate in severity and involves a partial rupture of the ligament resulting in moderate pain and swelling as well as mild to moderate instability, resulting in difficulty with weight-bearing. Grade III injuries are the most severe and involve a complete ligament rupture, leading to significant pain, swelling, and hematoma formation. Grade III injuries cause severe functional impairment and instability.12 Ligamentous stability can be assessed for the ATF through the anterior drawer test, and compared to the unaffected side, and CFL integrity can be assessed through a talar tilt test.19 Because most patients in the emergency department are in too much acute pain for these exams to be performed adequately, the utility of grading ankle sprains in the emergency department is limited. Ultimately, if the patient has significant swelling and loss of function (ability to bear weight), this represents a higher ankle sprain that may require more aggressive immobilization with appropriate physical therapy and primary care follow-up.
Diagnosis of Ankle Sprains
The first step in diagnosis of ankle sprains is classification of which type of ankle sprain occurred based on clinical history and a focused physical exam of the ligaments discussed above. To confidently diagnose an ankle injury as a sprain rather than a more significant injury, the pain and swelling documented on exam must coincide with the injury pattern expected. Despite only identifying fractures in up to 20% of patients,20 X-rays are obtained in 60-100% of children with ankle injuries.21 Clinical decision tools can aid in identifying injuries that require imaging while minimizing unnecessary studies. (See Table 1.) The Ottawa Ankle Rules were developed by Stiell et al as a clinical decision tool to help determine when radiologic evaluation is necessary in acute ankle and midfoot injuries.22 They have been found to be 100% sensitive in the adult population for ruling out fractures; by using this tool, emergency departments have been able to decrease X-ray use, wait times, and cost.23 A meta-analysis by Dowling et al found the Ottawa Ankle Rules to be a reliable tool to exclude fractures in children older than 5 years of age who present to the emergency department with ankle and midfoot injuries.24 The Ottawa Ankle Rules state that imaging of the ankle is only necessary if there is pain in the malleolar zone plus one of the following: bony tenderness along the distal 6 cm of the posterior edge of the medial or lateral malleolus or inability to bear weight for four steps immediately after the injury and in the emergency department. In terms of midfoot imaging, the rules recommend imaging only with pain in the midfoot region plus one of the following: bony tenderness at the navicular bone or the base of the fifth metatarsal or inability to bear weight for four steps immediately after the injury and in the emergency department. Navicular and fifth metatarsal injuries will be discussed later in this article. Based on the data by Dowling et al, application of the Ottawa Ankle Rules in pediatric patients would reduce X-ray usage by about 25%.24
Table 1. Clinical Decision Tools for Imaging Ankle Injuries |
|
|
Ottawa Ankle Rules |
Low Risk Ankle Rule |
|
Validated for pediatric patients (Dowling et al.) Only image if:
PLUS
OR
|
Developed for pediatric patients No imaging if all criteria are met:
|
|
SOURCE: Author adapted. |
|
The Low Risk Ankle Rule is a tool that was developed specifically for children to help determine when X-rays are needed. Pediatric patients are considered low risk if the injury is acute (defined as less than 3 days old), if they are not at risk for pathologic fracture (for example, children with a focal bone lesion or osteogenesis imperfecta), if they do not have a congenital anomaly of the feet or ankles, if they are able to express pain or tenderness, if pain and swelling are limited to the distal fibular or surrounding lateral ligaments distal to the anterior tibial joint line, and if no gross deformity, neurovascular compromise, or other distracting injury is present.25 In the Low Risk Ankle Rule, distal fibular avulsion fractures and nondisplaced Salter-Harris I and II fractures are considered low-risk injuries since they are managed with supportive splinting, crutches if needed, and return to activities as tolerated.
The Low Risk Ankle Rule has been shown to have a sensitivity of 98-100% for clinically important ankle fractures as well as to reduce the number of X-rays and, thus, cost in the emergency department.26,27
Even if the patient’s exam is consistent with an ankle sprain, and per clinical decision tools there is no indication for imaging, it is still important to push on six spots to guarantee not to miss a high-morbidity injury. These six spots are: 1) the proximal fibula to rule out Maisonneuve fracture; 2) talus to rule out a talar neck, dome, or lateral process fracture; 3) navicular bone to rule out navicular fracture; 4) base of the fifth metatarsal to rule out a Jones or pseudo-Jones fracture; 5) base of the first and second metatarsal to rule out a Lisfranc injury; 6) and the tibial and fibular physes to assess for Salter-Harris fracture. The mechanics and management of these injuries will be discussed later in the article. To avoid missing high-morbidity injuries in the ankle, a simple ankle sprain can be diagnosed only if three criteria are met: 1) there is no pain over these six locations, 2) the exam is consistent with ligamentous injury, and 3) there is no indication for imaging per Ottawa Ankle Rules.
Management of Ankle Sprains
Although management of ankle sprains depends on the type of sprain as well as the severity, the overall goals of management for ankle sprains in the emergency department are to control pain, reduce post-injury edema, and functionally support the ankle to allow early mobilization. Minor ankle sprains caused from inversion strain can be managed conservatively with rest, ice, elevation, and immobilization.13 Options include bracing, Aircast, Ace bandage, and a walker boot. Recent studies suggest bracing, Aircast, and Ace bandage allow more rapid return to function by allowing early mobilization. The overall consensus is that if a patient has a mild or moderate ankle sprain, an Ace bandage28 or Aircast should be used.29 If an Aircast is provided, an Ace bandage also should be used to prevent dependent anterior edema that can limit plantar and dorsiflexion. If the patient has considerable swelling, loss of function, and instability, a walker boot will immobilize the injury more aggressively and will allow functional return to activities of daily living. With the exception of syndesmotic ankle sprains, numerous studies show that early weightbearing and mobilization more rapidly improve functional return after an ankle sprain.28,29,30 Syndesmotic ankle sprains are more severe and require more aggressive management with a walker boot and crutches.14 The prolonged course of this injury, as well as the importance of following up with a specialist, should be discussed with the patient.
All ankle sprain patients should be advised of the importance of physical therapy in follow-up. Therapy that emphasizes ankle strength and proprioception can be effective for the prevention of ankle sprains in athletes with previous sprains.12,32 Inappropriate follow-up can lead to chronic ankle instability, impingement, and early osteoarthritis.
What if It’s Not an Ankle Sprain? Injuries Not to Miss in the ED
For emergency medicine physicians, ankle sprains are ultimately a diagnosis of exclusion. The emergency provider first must consider injuries that can mimic ankle sprains but are associated with a high morbidity. (See Table 2.) These include Maisonneuve fracture, talar fractures, navicular fractures, Jones or pseudo Jones fractures, Lisfranc injuries, and Salter-Harris fractures.
Table 2. Six Foot/Ankle Injuries Not to Miss in the Emergency Department |
||
|
Injury |
Exam |
Management |
|
Maisonneuve fractures |
Pain over the proximal fibula |
Long-leg posterior splint Urgent orthopedic follow-up |
|
Talar fractures |
Pain over the talar dome/neck/lateral process |
Non-weightbearing in walker boot or posterior splint Specialist follow-up in one week |
|
Navicular fractures |
Pain over the dorsal or medial navicular |
Non-weightbearing in walker boot Specialist follow-up in one week |
|
Fifth metatarsal fractures |
Pain over the fifth metatarsal |
Pseudo-Jones: Ortho shoe or walker boot Jones: Non-weightbearing in posterior splint Specialist follow-up in one week |
|
Lisfranc injuries |
Pain/bruising/swelling over the |
Non-weightbearing in posterior splint Specialist follow-up in one week |
|
Salter-Harris fractures |
Pain over the tibial/fibial growth plate |
Salter-Harris I & II: Non-weightbearing in posterior splint Specialist follow-up in one week Salter-Harris III & IV: Long-leg splint, urgent orthopedic follow-up |
Can’t-miss Injury #1: Maisonneuve Fractures
Proximal fibular fractures, or Maisonneuve fractures, are caused by external rotation of the ankle joint with force transmitted through the tibiofibular syndesmosis. Although proximal fibula fractures alone do not require surgical intervention, they do suggest an injury from a high degree of force and may be associated with a medial malleolus fracture or a rupture of the deltoid ligament, anterior talofibular ligament, or interosseous ligament.33 Injuries to these ligaments may be difficult to appreciate on exam, but are associated with a high degree of ankle mortise instability that may require surgical intervention.34 The presence of proximal fibular pain necessitates X-rays of the tibia/fibula and an ankle X-ray, including a gravity view. The gravity view will help ascertain if there is considerable mortise instability that will require operative intervention. Maisonneuve fractures should be placed in a long-leg posterior splint with urgent orthopedic follow-up.
Can’t-miss Injury #2: Talar Fractures
Although less common than other ankle injuries, fractures to the talus (see Figure 2) can occur with rotational injuries to the ankle and have a high rate of complications. If the talar neck, dome, or lateral process is painful to palpation on exam, the provider should obtain ankle X-rays, including an oblique view. Talar neck fractures are the most common talar fracture but are often overlooked in the setting of ankle injuries.35 These fractures are caused by extremes of dorsiflexion. On exam, patients will have focal tenderness over the talar neck associated with edema and pain with range of motion. Talar neck fractures are best viewed on the lateral view of the ankle X-ray. The blood supply to the talus is distal and there is a retrograde supply to the talar body from branches of the posterior tibial artery. This leads to a risk of osteonecrosis if the talar neck is disrupted.36 Avascular necrosis of the talar body is a devastating consequence of talar neck fractures, making talar fractures high risk if not managed appropriately.37,38 Talar neck fractures (see Figure 3) also can lead to post-traumatic arthritis of the subtalar joint.36 These fractures require close follow-up by an orthopedist.
Figure 2. Bones of the Ankle |
 |
|
SOURCE: Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved. |
Figure 3. Talar Neck Fracture |
 |
Talar dome fractures (see Figure 4), or osteochondral dome fractures, occur with impaction in inversion and eversion ankle injuries. This results in trauma to the cartilage of the talus and its underlying subchondral bone.39 The most common location for these injuries is anterolateral or posteromedial. Radiographically, talar dome fractures are best visualized on the mortise view. However, up to 30% of talar dome compression fractures are not seen on radiography, and patients with these fractures are often mistakenly diagnosed with an ankle sprain.40 Clinically, patients present with point tenderness and pain with range of motion. Missed injuries can lead to non-union and early-onset arthritis; thus, specialist follow-up is imperative.
Figure 4. Talar Dome Fracture |
 |
Fractures to the lateral process of the talus, or snowboarder’s fractures, are uncommon, but their incidence is increasing because of the growing popularity of snowboarding.41 These fractures are thought to occur as a result of pathologic dorsiflexion and inversion, and they happen with greater frequency in snowboarders because of the impact of landing from a jump while their foot is held in dorsiflexion inside their boot.42
These are exceptionally difficult to diagnose, as they present identically to an inversion ankle sprain with pain in the location of the ATF ligament. The lateral talus is the insertion point of the ATF. On exam, pain is most prominent 1 cm distal to the lateral malleolus. Pain with dorsiflexion and external rotation should raise concern since this maneuver causes impingement on the fracture site but does not stress the ATF ligament and, thus, inversion ankle sprains should not hurt with this maneuver. These fractures have a miss rate of up to 60%, and missed injuries can lead to non-union, chronic ankle pain, and early-onset arthritis. They are best seen on mortise and oblique views. If a provider has clinical suspicion for a talar fracture (even if X-rays are negative), the patient should be placed in a walker boot or posterior splint with a non-weightbearing status and have follow-up imaging and reassessment by an orthopedic specialist in one week. CT scan is recommended in patients who present with a history of a snowboard injury or jump plus one or more positive Ottawa ankle criteria.41
Can’t-miss Injury #3: Navicular Fractures
The navicular bone (see Figure 2) is critical for maintaining the medial longitudinal arch; thus, delayed diagnoses can lead to chronic gait disturbances and disabling foot pain. Navicular fractures are classified as dorsal or tuberosity avulsion fractures or body fractures. Avulsion fractures are the most common fractures and are associated with a low-energy mechanism of injury, while body fractures require high-energy mechanisms like a motor vehicle collision.43 Dorsal avulsion fractures (see Figure 5) result from a disruption of the talonavicular ligament associated with inversion ankle injuries. Tuberosity avulsion fractures occur with forced eversion of the ankle and midfoot, causing traction to the posterior tibial tendon or deltoid ligament, which then results in the avulsion fracture. Tuberosity fractures (see Figure 6) must be differentiated from an accessory navicular on X-ray. An accessory navicular is usually bilateral and appears as a smooth corticated bone medial to the navicular, while a tuberosity fracture has an irregular trabecular appearance.44 These injuries are difficult to appreciate on initial routine X-rays and may be visible only in about half of cases;13 thus, they require a high index of suspicion. Dorsal avulsion fractures are best seen on lateral view, and tuberosity avulsion fractures on AP and external oblique views. Because of the high morbidity associated with these fractures, the emergency provider should palpate the medial navicular and N spot for every rotational ankle and foot injury. The medial navicular is the bony prominence just distal to the talus at the mid-arch of the foot. The N spot is the dorsal navicular between the anterior tibial tendon and the extensor hallucis longus tendon. Pain in these locations requires non-weightbearing and placement in either a walker boot or posterior splint, as well as specialist follow-up in one week.45
Figure 5. Dorsal Navicular Avulsion |
 |
Figure 6. Navicular Tuberosity Fracture |
 |
Can’t-miss Injury #4: Jones and Pseudo-Jones Fractures
Fifth metatarsal fractures are the most common metatarsal fractures in children and comprise about 5% of all fractures in children.46 These fractures occur with inversion ankle injuries or rotational foot injuries. Figure 7 depicts basic bony anatomy of the foot. Pain with palpation to the fifth metatarsal necessitates dedicated foot films to examine the zone-specific location of the injury. There are three zones of injury in which fifth metatarsal fractures can occur. Zone 1 injuries, also called pseudo-Jones fractures, occur during an inversion injury to the ankle when the peroneal brevis tendon or lateral band of the plantar fascia causes an avulsion injury to the base of the fifth metatarsal. These injuries can be appreciated on the lateral view of the ankle, but require a dedicated foot X-ray to determine displacement. Patients with pseudo-Jones fractures may bear weight as tolerated in a post-op shoe or walker boot and follow up with a specialist in one week. It is important to note that a fifth metatarsal apophysis can be mistaken as a zone 1 injury.47 An apophysis is an ossification center to which a tendon or ligament attaches. The fifth metatarsal apophysis is a vertically oriented bony fragment that runs parallel to the metatarsal shaft. Avulsion fractures are oriented transversely. It is important to recognize differences on X-ray, as a fifth metatarsal apophysis can be painful and swollen in the setting of fifth metatarsal apophysitis,13 also known as Iselin disease. Figure 8 shows both a fifth metatarsal avulsion fracture and a fifth metatarsal apophysis.
Figure 7. Basic Bony Anatomy of the Foot |
 |
|
SOURCE: Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved. |
Figure 8. Fifth Metatarsal Fracture and Fifth Metatarsal Apophysis |
|
This X-ray from a 12-year-old male shows both a fifth metatarsal fracture and a fifth metatarsal apophysis. There is a transverse lucency extending through the base of the right fifth metatarsal consistent with a nondisplaced fracture. The fracture line extends almost to the tarsal metatarsal joint but does not extend intra-articularly. This injury was sustained while playing football.
|
Zone 2 injuries are also referred to as Jones fractures. These occur with an adducted force applied to a plantar flexed foot48 and happen more commonly in the adolescent athlete than in younger patients.13 Jones fractures involve a fracture to the proximal metaphyseal diaphyseal junction. There is a limited vascular supply to this area, leading to a high risk of delayed healing and non-union with these injuries.49 Patients should be strictly non-weightbearing and placed in a posterior splint in the emergency department. They can be transitioned to a short leg cast in the outpatient setting. Zone 3 injuries can occur with blunt trauma, rotational injuries, or repetitive stress from athletic activities. These are proximal diaphyseal fractures located distal to the fourth and fifth metatarsal articulation. Management is the same as zone 2 injuries, with strict non-weightbearing and placement in a posterior splint with transition to a short leg cast.50 Zone I and II injuries should be followed up by an orthopedic specialist in one week.
Can’t-miss Injury #5: Lisfranc Injuries
Lisfranc injuries are complex and often missed injuries that are characterized by a ligamentous injury or fracture and/or dislocation to the tarsometatarsal joint. The Lisfranc joint is critical to stability of the midfoot, and mismanaged injuries can lead to debilitating foot pain and gait disturbances.51 These injuries are caused by plantar flexion with a rotational force identical to the mechanism of an inversion sprain. They occur more frequently in football players52 or children jumping from a height, hence their nickname of “bunk bed fractures.”53 On physical exam, plantar bruising is classic. Ligamentous injury may be subtle with only midfoot pain noted. Fracture dislocations are characterized by swelling and inability to bear weight.2 The patient will have pain with pronation and abduction of the foot.
In patients with a suspected Lisfranc injury, it is critical to obtain weightbearing images (AP, lateral, oblique) of the foot. Radiographic signs of Lisfranc injury on AP film include a separation greater than 2 mm between the base of the first and second metatarsals (see Figure 9a); “fleck sign,” which is a fracture at the base of the second metatarsal;54 and disrupted alignments of the lateral border of the first metatarsal with the lateral border of the medial cuneiform as well as the medial border of the second metatarsal with medial border of the middle cuneiform.55 As X-ray signs are subtle, a film of the contralateral foot is helpful for comparison (see Figure 9b). CT or MRI in the outpatient setting may be helpful if a Lisfranc injury is suspected but not seen on plain films.5 It is important for the emergency physician to have a high index of suspicion for these injuries, and if X-rays are negative but there is still clinical concern, the patient should be non-weightbearing and placed in a posterior splint or walker boot with close outpatient follow-up and referral to orthopedics.
Figure 9. Lisfranc Injuries |
|
Figure 9a represents a Lisfranc injury. This occurred after an inversion injury of the ankle and was missed on the patient’s initial emergency department visit.
|
|
Figure 9b shows weight-bearing images obtained on the same patient one month later, when she re-presented with ongoing midfoot pain and inability to bear weight. The stress view as well as visualization of the contralateral foot allows the lateral subluxation at the second tarso-metarsal joint of the left foot to be identified.
|
Can’t-miss Injury #6: Salter-Harris Fractures
In pediatric patients with open growth plates, the physician should palpate a sixth location: the tibial and fibular growth plate. It is critical not to be fooled into thinking that lateral ankle pain with normal X-rays in the pediatric patient is diagnostic of an ankle sprain. Pain over the tibial or fibular growth plate represents a Salter-Harris type I fracture and must be managed appropriately with placement in a posterior splint and non-weightbearing.30 Salter-Harris fractures will be discussed in more detail in the next section.
Ankle Fractures — General, Epidemiology
Ankle fractures make up about 5% of pediatric fractures and 15% of growth plate injuries. They occur more often in boys than girls and peak between the ages of 8 and 15 years.55,56,57 These injuries occur more often in overweight athletes58 and in basketball, soccer, and football players.59 As mentioned previously, pediatric patients are less prone to ligamentous injuries because ligaments tend to be stronger than open growth plates. As a result, minimal trauma that generally would cause a sprain in an adult (for example, an inversion injury) may cause physeal fractures in pediatric patients.32 However, it is also important to ensure that physical exam findings correlate with radiographic findings because accessory ossification centers seen on X-ray sometimes are misinterpreted as fractures.55
Distal Tibial Fractures
General
The distal tibial physis is responsible for 45% of overall growth of the tibia, and growth usually continues until 14 years of age in girls and 16 years of age in boys.56 Before the physis closes completely, there is an 18-month transitional period during which up to 15% of physeal fractures in adolescents occur.57 Fractures of the distal tibial physis are the second most common physeal fracture, second only to fractures of the distal radius.55 Fractures of the distal tibia are classified into Salter-Harris types I-IV.60
Salter-Harris Types I and II
Salter-Harris type I and II fractures have a lower risk of growth plate arrest, or premature physeal closure, than types III and IV and are managed similarly in the emergency department.56,61 A Salter-Harris type I fracture is a transverse fracture through the physis. It is important to note that these fractures can lead to widening of the physes but may not show any initial X-ray abnormalities. Thus, the emergency physician needs to have a high index of suspicion for these fractures when there is pain over the medial malleolus or tibial growth plate, even in the setting of negative X-rays. Salter-Harris type II fractures are the most common type, accounting for about 40% of distal tibial fractures.56,57 These fractures are through the physis, with extension of the fracture pattern through the metaphysis. Salter-Harris types I and II fractures can result in growth plate arrest in patients.62 In the emergency department, Salter-Harris types I and II fractures should be placed in a posterior splint with the patient non-weightbearing. The splint can be transitioned to a cast in one week when the patient follows up with orthopedics.13
Salter-Harris Types III and IV
Salter-Harris type III fractures extend through the physis and downward through the epiphysis and account for about 25% of distal tibial fractures.63 Near the epiphysis is the reserve zone of the physis that contains progenitor cells for continued physeal growth; thus, appropriate reduction of these fractures is critical, as inappropriate reduction can lead to physeal arrest.11,57 Salter-Harris type III fractures also represent intra-articular fractures, so anatomic reduction is critical to prevent intra-articular step off. CT scan may be helpful to determine the degree of displacement. Tillaux fractures are a Salter-Harris type III variant that occurs in adolescents during the 18-month transitional period when the tibial physis is closing medially to laterally, leaving the lateral physis susceptible to fracture and displacement.64 Tillaux fractures occur when an external rotation force is applied to the partially closed tibial growth plate.13 This results in an avulsion injury at the insertion of the anterior inferior tibiofibular ligament on the lateral distal tibial epiphysis.64 Tillaux fractures account for 3-5% of overall pediatric ankle fractures.56 Salter-Harris III fractures often require reduction. The technique is plantar flexion, internal rotation, and manual pressure over the displaced fragment. No more than two attempts at reduction should be made.56,57 Patients should be non-weightbearing and placed in a long leg splint with the foot in internal rotation. These injuries require urgent orthopedic follow-up.
Salter-Harris type IV fractures are the most severe and carry the highest risk of growth arrest.56 These fractures extend through the physis, metaphysis, and epiphysis, creating an unstable growth plate fracture fragment that also has an intra-articular component. Salter-Harris type IV fractures include trimalleolar fractures, defined as fracture lines in three anatomic planes (see Figure 10), and lateral triplane fractures. Lateral triplane fractures comprise 5-15% of pediatric ankle fractures56 and, like Tillaux fractures, they occur during the transitional period of physeal closure.57 In lateral triplane fractures, the metaphysis fracture line extends in the coronal plane, the epiphysis fracture in the sagittal plane, and the physeal fracture in the axial plane. This creates an unstable fracture fragment in the medial epimetaphysis of the tibial shaft.65 Triplane fractures typically occur with external rotation to a supinated foot. Anatomic reduction is critical and usually requires specialist consultation. Closed reduction is performed via axial traction and internal rotation. As with Salter-Harris III fractures, CT scan is helpful to determine the degree of displacement, and these patients should be placed in a long-leg splint with internal rotation.66 These patients require urgent orthopedic follow-up and management. Open reduction is recommended for physeal fractures with a gap of 3 mm or more.13,58,67
Figure 10. Salter-Harris IV Trimalleolar Fracture |
 |
Distal Fibula Fractures
Salter-Harris Fractures
The fibula is a non-weightbearing bone, so more aggressive weightbearing can be tolerated by patients with fractures to the fibula. Salter-Harris type I and II fractures comprise about 90% of distal fibula fractures.58 Salter-Harris type I fractures of the fibula are common and often are missed or misdiagnosed as a sprain. The classic history is an external rotation force. It is important for the emergency provider to palpate over the fibular physis, about 2 cm from the distal fibula, and not to assume that lateral ankle pain is secondary to sprain. Localized pain and swelling over the distal fibular physis is diagnostic. X-rays are usually normal in these fractures, making it a clinical diagnosis. Patients should be placed in a walker boot, weightbearing as tolerated, and primary care follow-up for repeat exam in one week. Salter-Harris type II fractures are not commonly recognized in the fibula and management is the same as for Salter-Harris type I fractures. Fractures of the distal fibula combined with a Salter-Harris type II injury of the distal tibia are a common ankle injury in pediatric patients.13 Isolated Salter-Harris type III and IV fractures of the fibula are rare and need to be distinguished from an accessory ossification center, os fibulare.58
Os fibulare is an accessory ossicle distal to the fibula that can be misinterpreted as a fracture.68 It is thought to be secondary to an old avulsion fracture or non-union of an accessory ossification center. The os fibulare may become symptomatic with overuse, and especially is seen in ballet dancers and gymnasts.69 Avulsion of the accessory ossification center also can occur and is based on clinical suspicion and pain with palpation.70 These avulsion fractures can be considered Salter-Harris II fractures.71 If painful with palpation on exam, the patient should be placed in a walker boot, weight-bearing as tolerated, with primary care follow-up.
Conclusion
Pediatric lower extremity injuries commonly present in the emergency department, especially with increasing sports specialization in young athletes. Injuries to the ankle and foot make up the majority of these injuries, and ankle sprains are a frequent occurrence. X-rays are not always necessary, as both the Ottawa Ankle Rules and the Low Risk Ankle Rule demonstrate. However, the emergency physician must be sure not to miss a high-morbidity injury that may masquerade as an ankle sprain. Thus, it is important to rule out Maisonneuve fracture, talar fractures, navicular fractures, Jones or pseudo-Jones fractures, Lisfranc injuries, and Salter-Harris fractures by a careful exam and obtain appropriate radiographic images. Pediatric patients are more vulnerable to ankle fractures than adult patients because children have open growth plates. Likewise, ankle fractures in the pediatric population have particular implications because of physeal anatomy. A comprehensive understanding of both common and high-morbidity pediatric ankle and foot injuries, as well as how to assess and treat them, is crucial for the emergency physician.
REFERENCES
- National Council of Youth Sports. National Council of Youth Sports Report on Trends and Participation in Organized Youth Sports 2008 edition. 2008. Available at: http://www.ncys.org/pdfs/2008/2008-ncys-market-research-report.pdf. Accessed June 4, 2016.
- Browne GJ, Barnett PL. Common sports-related musculoskeletal injuries presenting to the emergency department. J Paediatr Child Health 2016;52:231-236.
- Burt CW, Overpeck MD. Emergency visits for sports-related injuries. Ann Emerg Med 2000;7:1376-1382.
- Emery CA, Meeuwisse WH, McAllister JR. A survey of sport participation, sport injury and sport safety practices in adolescents. Clin J Sport Med 2006;16:20-26.
- Emery C. Risk factors for injury in child and adolescent sport: A systematic review. Clin J Sport Med 2003;13:256-268.
- Stracciolini A, Casciano R, Levely Friedman H, et al. Pediatric sports injuries: A comparison of males versus females. Am J Sports Med 2014;42:965-972.
- Soprano J. Musculoskeletal injuries in the pediatric and adolescent athlete. Curr Sports Med Rep 2005;4:329-334.
- Malanga GA, Ramirez-Del Toro JA. Common injuries of the foot and ankle in the child and adolescent athlete. Phys Med Rehabil Clin N Am 2008;19:347-371.
- Soprano JV, Fuchs SM. Common overuse injuries in the pediatric and adolescent athlete. Clin Pediatric Emerg Med 2007;8:7-14.
- Davis KW. Imaging pediatric sports injuries: Lower extremity. Radiology Clin North Am 2010;48:1213-1215.
- Chambers HG, Haggerty CJ. The foot and ankle in children and adolescents. Operative Techn Sports Med 2006;14:173-187.
- Peterson W, Rembitzki IV, Koppenberg AG. Treatment of acute ankle ligament injures: A systematic review. Arch Orthop Trauma Surg 2013;133:1129-1141.
- Sullivan JA, Lewis TR. Foot and ankle injuries in the adolescent athlete. In: DeLee & Drez’s Orthopaedic Sports Medicine. 4th ed. St. Louis, MO: Saunders; 2015;1661-1675.
- McCriskin BJ, Cameron KL, Orr JD, et al. Management and prevention of acute and chronic lateral ankle instability in athletic patient populations. World J Orthop 2015;6:161-171.
- Fong DT, Hong Y, Chan LK, et al. A systematic review on ankle injury and ankle sprain in sports. Sports Med 2007;37:73-94.
- Williams GN, Allen EJ. Rehabilitation of syndesmotic (high) ankle sprains. Sports Health 2010;2:460-470.
- Gerber JP, Williams GN, Scovill CR, et al. Persistent disability associated with ankle sprains: A prospective review of an athletic population. Foot Ankle Int 1998;19:653-660.
- Hopkins WP, Ryan JB, Wheeler JH. Syndesmosis sprains of the ankle. Foot Ankle 1990;10:325-330.
- Singh RK, Kamal T, Roulohamin N, et al. Ankle fractures: A literature review of current treatment methods. Open J Orthop 2014;4:292-303.
- Clark KD, Tanner S. Evaluation of the Ottawa Ankle Rules in children. Pediatr Emerg Care 2003;19:73-78.
- Al Omar MA, Baldwin GA. Reappraisal of use of X-rays in childhood ankle and midfoot injuries. Emerg Radiol 2002;9:88-92.
- Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiography in acute ankle injuries: Refinement and prospective validation. JAMA 1993;269:1127-1132.
- Anis AH, Stiell IG, Stewart DG, Laupacis A. Cost-effectiveness analysis of the Ottawa Ankle Rules. Ann Emerg Med 1995;26:422-428.
- Dowling S, Spooner CH, Liang Y, et al. Accuracy of Ottawa Ankle Rules to exclude fractures of the ankle and midfoot in children: A meta-analysis. Acad Emerg Med 2009;16:277-287.
- Boutis K, Grootendorst P, Wilan A, et. al. Effect of the Low Risk Ankle Rule on the frequency of radiography in children with ankle injuries. CMAJ 2013;185:E731-E738.
- Boutis K, Von Keyserlingk C, Willan A, et al. Cost consequence analysis of implementing the Low Risk Ankle Rule in emergency departments. Ann Emerg Med 2015;66:455-463.
- Ramasubbu B, McNamara R, Okafor I, Deiratany S. Evaluation of safety and cost-effectiveness of the low risk ankle rule in one of Europe’s busiest pediatric emergency departments. Pediatr Emerg Care 2015;31:685-687.
- Fousekis K, Billis E, Matzaroglou C, et al. Elastic bandaging for sports injuries prevention and rehabilitation: A systematic review. J Sport Rehabil 2016; Jun 14 [Epub ahead of print].
- Boyce SH, Quiqley MA, Campbell S. Management of ankle sprains: A randomized controlled trial of the treatment of inversion injuries using an elastic support bandage or an Aircast ankle brace. Br J Sports Med 2005;39:91-96.
- Aredevol J, Bolibar I, Belda V, et al. Treatment of complete rupture of the lateral ligaments of the ankle: A randomized clinical trial comparing cast immobilization with functional treatment. Knee Surg Sports Traumatol Arthrosc 2002;10:371-377.
- Jones MH, Amendola AS. Acute treatment of inversion ankle sprains: Immobilization versus functional treatment. Clin Orthop Relat Res 2008;455:169-172.
- Emery CA, Roy TO, Whittaker JL, et al. Neuromuscular training injury prevention in youth sport: A systematic review and meta-analysis. Br J Sports Med 2015;49: 865-870.
- Stufkens SA, van den Bekerom MP, Doornberg JN, et al. Evidence-based treatment of Maisonneuve fractures. J Foot Ankle Surg 2011;50:62-67.
- Millen JC, Lindberg D. Maisonneuve fracture. J Emerg Med 2011;41:77-78.
- Wu YJ, Jiang H, Wang B, Miao W. Fracture of the lateral process of the talus in children: A kind of ankle injury with frequently missed diagnosis. J Pediatr Orthop 2016;36:289-293.
- Dodd A. Outcomes of talar neck fractures: A systematic review and meta-analysis. J Orthop Trauma 2015;39:210-215.
- Kamphuis SJ, Meijs CM, Kleinveld S, et al. Talar fractures in children: A possible injury after go-karting accidents. J Foot Ankle Surg 2015;54:1206-1212.
- Eberl R, Singer G, Schalamon J, et al. Fractures of the talus: Differences between children and adolescents. J Trauma 2010;68:126-130.
- Melenevsky Y, Mackey RA, Abrahams RB. Talar fractures and dislocations: A radiologist’s guide to timely diagnosis and classification. Radiographics 2015;35:765-779.
- Dale JD, Ha AS, Chew FS. Update on talar fracture patterns: A large level I trauma center study. AJR Am J Roentgenol 2013;201:1087-1092.
- Kramer IF, Brouwers L, Brink PR, et al. Snowboarders’ ankle. BMJ Case Rep 2014 Oct 29; pii: bcr2014204220. doi: 10.1136/bcr-2014-204220.
- Wu Y, Jiang H, Wang B, et al. Fracture of the lateral process of the talus in children: A kind of ankle injury with frequently missed diagnosis. J Pediatr Orthop 2016;36:289-293.
- Ramadorai UE, Beuchel MW, Sangeorzan BJ. Fractures and dislocations of the tarsal navicular. J Am Acad Orthop Surg 2016;24:379-389.
- Rosenbaum AJ, Uhl RL, DiPreta J. Acute fractures of the tarsal navicular. Orthopedics 2014;37:541-546.
- Yngve DA. Stress fractures. In: Sullivan JA, Anderson SJ. Care of the Young Athlete. 1st ed. American Academy of Orthopedic Surgeons, American Academy of Pediatrics, 2000.
- Herrera-Soto JA, Scherb M, Duffy MF, et al. Fractures of the fifth metatarsal in children and adolescents. J Pediatr Orthop 2007;27:427-431.
- Riccardi G, Riccardi D, Maracarelli M, et al. Extremely proximal fractures of the fifth metatarsal in the developmental age. Foot Ankle Int 2011;32:S526-532.
- Lawrence SJ, Botte MJ. Jones’ fractures and related fractures of the proximal fifth metatarsal. Foot Ankle 1993;14:358-365.
- Herrara-Soto JA, Scherb M, Duffy MF, et al. Fractures of the fifth metatarsal in children and adolescents. J Pediatr Orthop 2007;27:427-431.
- Rosenberg GSJ. Treatment strategies for acute fractures and nonunions of the proximal fifth metatarsal. J Am Acad Orthop Surg 2000;8:332-338.
- Veijola K, Laine HJ, Pajulo O. Lisfranc injury in adolescents. Eur J Pediatr Surg 2013;23:297-303.
- Nunley JA, Vertullo CJ. Classification, investigation, and management of midfoot sprains: Lisfranc injuries in the athlete. Am J Sports Med 2002;30:871-878.
- Johnson GF. Pediatric Lisfranc injury: “Bunk bed” fracture. AJR Am J Roentgenol 1981;137:1041-1044.
- Kay RM, Tang CW. Pediatric foot fractures: Evaluation and treatment. J Am Acad Orthop Surg 2001;9:308-319.
- Crawford H. Fractures and Dislocations of the Foot. In: Flynn JM, Skaggs DL, Waters PM, eds. Rockwood and Wilkins’ Fractures in Children. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2010.
- Podeszwa DA, Mubarak SJ. Physeal fractures of the distal tibia and fibula (Salter-Harris Type I, II, III, and IV fractures). J Pediatr Orthop 2012;32(Suppl 1):S62-S68.
- Wuerz TH, Gurd DP. Pediatric physeal ankle fracture. J Am Acad Orthop Surg 2013;21:234-244.
- Kay RM, Matthys GA. Pediatric ankle fractures: Evaluation and treatment. J Am Acad Orthop Surg 2001;9:268-278.
- Zonfrillo MR, Seiden JA, House EM, et al. The association of overweight and ankle injuries in children. Ambul Pediatr 2008;8:66-69.
- Blackburn EW, Aronsson DD, Rubright JH, et al. Ankle fractures in children. J Bone Joint Surg Am 2012;94:1234-1244.
- Fong DT, Man CY, Yung PS, et al. Sport-related ankle injuries attending an accident and emergency department. Injury 2008;39:1222-1227.
- Rohmiller MT, Gaynor TP, Pawelek J, et al. Salter-Harris I and II fractures of the distal tibia: Does mechanism of injury relate to premature physeal closure? J Pediatr Orthop 2006;26:322-328.
- Mizuta T, Benson WM, Foster BK, et al. Statistical analysis of the incidence of physeal injuries. J Pediatric Orthoped 1987;7:518-523.
- Su AW, Larson AN. Pediatric ankle fractures: Concepts and treatments. Foot Ankle Clin 2015;20:705-719.
- Rohmiller MT, Gaynor TP, Pawelek J, et al. Salter-Harris I and II fractures of the distal tibia: Does mechanism of injury relate to premature physeal closure? J Pediatr Orthop 2006;26:322-328.
- Horner K, Tavarez M. Pediatric ankle and foot injuries. Clin Pediatr Emerg Med 2016;17:38-52.
- Charlton M, Costello R, Mooney JF, et al. Ankle joint biomechanics following transepiphyseal screw fixation of the distal tibia. J Pediatr Orthop 2005;25:635-640.
- Pill SG, Hatch M, Linton JM, Davidson RS. Chronic symptomatic os subfibulare in children. J Bone Joint Surg Am 2013;95:e115(1-6).
- Marsh JS, Daigneault JP. Ankle injuries in the pediatric population. Curr Opin Pediatr 2000;12:52-60.
- Nault ML, Kocher MS, Micheli LJ. Os trigonum syndrome. J Am Acad Orthop Surg 2014;22:545-553.
- Ogden JA, Lee J. Accessory ossification patterns and injuries of the malleoli. J Pediatr Orthop 1990;10:306-316.
Pediatric lower extremity injuries are common in the emergency department, especially with increasing sports specialization in young athletes. Acute care providers need to be familiar with common injury patterns, indications for radiographs, and more specialized imaging. Recognizing and maintaining a high degree of suspicion for high-morbidity injuries that may masquerade as an ankle sprain is critical. The authors review common injuries and also injuries that cannot be missed including Maisonneuve fracture, talar fractures, navicular fractures, Jones or pseudo-Jones fractures, Lisfranc injuries, and Salter-Harris fractures.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.



